Serous-fibrinous peritonitis is a pathology based on the inflammatory process of the peritoneal layers, accompanied by the accumulation of serous-fibrous exudate in the peritoneal cavity. The disease is characterized by severe pain in the abdominal cavity, tension in the abdominal muscles, nausea, vomiting, upset stool, increased body temperature and deterioration in the general condition of the patient.
Serous peritonitis is an inflammatory process in which serous exudate is observed in the abdominal cavity.
The main cause of the development of all peritonitis is infection of the peritoneal layers as a result of bacterial microorganisms entering the abdominal cavity.
The main reasons for the development of peritonitis are:
- Acute or chronic appendicitis;
- Blunt and penetrating traumatic injury to the abdomen;
- Acute inflammatory processes of the internal female genital organs;
- Perforation in the gastrointestinal tract of ulcerative formations;
- Damage to the intestinal walls or bile ducts.
Among the bacterial microorganisms that can cause the development of peritonitis, both gram-negative and gram-positive bacteria are noted. In this regard, the selection of antibacterial therapy becomes significantly more complicated.
Based on the mechanism of pathogenic flora entering the abdominal cavity, peritonitis is divided into two types: primary and secondary.
Primary peritonitis develops when infection spreads from other foci of infection in the body.
Secondary peritonitis is a complication of local diseases of the gastrointestinal tract.
At the Yusupov Hospital, patients with serous-fibrinous peritonitis undergo specialized diagnostics, effective treatment and, if necessary, rehabilitation measures. Specialists have extensive clinical experience both in Russia and foreign countries. The Yusupov Hospital is equipped with the latest medical technologies that speed up the patient’s recovery process.
Local serous-fibrinous/serous peritonitis
Local peritonitis is an inflammatory process of the peritoneum, limited to a specific area and localized around the organ that is the cause of the pathological process.
Local serous-fibrinous peritonitis occurs due to the development of adhesions and the ability of the peritoneum to limit the inflammatory process. Most often, local serous peritonitis is closely associated with an acute disease of one or another abdominal organ (stomach, duodenum, gallbladder, segment of the small or large intestine, pelvic organs, kidneys). The main reason for the development of such peritonitis is perforation due to peptic ulcer of a hollow organ (stomach, duodenum, ulcerative colitis, gangrenous appendicitis, etc.). Local inflammatory processes in the abdominal cavity occur much more easily than generalized peritonitis; in some cases, patients even remain able to work. However, even with this course of the disease, untimely diagnosis and treatment can lead to a destructive process and the formation of abscesses in the abdominal cavity.
Clinical picture
To make a diagnosis, the doctor needs to collect a detailed history of the disease. Most often, patients with serous-fibrinous peritonitis report the following complaints:
- Abdominal pain, the localization of which depends on the source of inflammation;
- Nausea;
- Vomiting (possibly mixed with bile and contents of the large intestine);
- Suffering face;
- Pale skin;
- Cold sweat;
- Immobility;
- Forced position of the body (on the back or on the side with the legs brought to the stomach);
- Increased body temperature;
- Drop in blood pressure;
- Impaired consciousness (as the patient’s condition progresses);
- Pointed facial features;
- Yellowish tint of the skin and mucous membranes;
- Bloating.
Pediatric peritoneal diseases
There are exudative and nodular-adhesive forms. The exudative form is the result of sowing into the peritoneum of miliary and submiliary tubercles, which do not undergo cheesy degeneration, but stop at the stage of granulation formation and tend to reverse development. This seeding is accompanied by copious serous exudate, which can reach significant sizes and is clinically detected as a mobile effusion. The nodular-adhesive form corresponds to cheesy peritonitis, flowing without effusion. With it, initially, predominantly in the mesentery, around the navel, less often in the ileocecal region, not sharply limited, moderately dense infiltrates are formed. Of these, due to the proliferation of connective tissue, caseinization and calcification, dense, nodular, sharply limited, round or sausage-shaped tumors are formed. There is also a form in which there are only minor cheesy areas, while the intestinal loops are glued together. In these cases, the tumor is not felt, but the swollen abdomen is difficult to feel, and the examining finger has difficulty penetrating it.
Clinical illness begins with weakness and vague symptoms, as well as mild abdominal pain and sometimes vomiting. Then comes a slight fever. Gradually the abdomen enlarges, becomes uneven and gives characteristic palpation and percussion changes. The spleen is usually not particularly enlarged. Subsequently, the temperature persists with characteristic remissions. In favorable cases, after approximately 3 months, the temperature begins to gradually decrease; in unfavorable cases, diarrhea and lack of appetite can greatly disturb the general condition of the patient. Sometimes incomplete blockage of the intestines may also occur. There is also a breakthrough through the navel, either in the benign form of an ordinary fecal fistula, or in the malignant form - the opening of a purulent cavity to the outside.
In addition to generalized, there is also limited tuberculous disease of the glands and peritoneum, which can be expressed by various symptoms depending on the location and accompanying adhesions. Mention should be made of tuberculosis emanating from the cecum, which partially occurs in the form of lymphadenitis and can be confused with acute appendicitis.
The prognosis is conditionally favorable; nevertheless, when the patient is placed in hygienic conditions and rational treatment is carried out, the vast majority of patients recover. The exudative form is considered somewhat more favorable.
Diagnostics
Making a diagnosis of serous fibrinous peritonitis is associated with certain difficulties, so this process should only be carried out by a qualified doctor. At the Yusupov Hospital, specialists every day encounter various emergency conditions that require immediate diagnosis and treatment. The hospital has innovative equipment that is successfully used for diagnostic purposes to obtain results as quickly as possible.
After collecting anamnestic data, to complete the examination, doctors use:
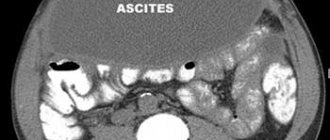
- Palpation and auscultation to determine the characteristic symptoms of the disease. When listening to bowel sounds, it is due to the accumulation of free fluid in the abdominal cavity. Noises are usually weakened or completely absent.
- X-ray examination of the abdominal organs. A characteristic sign of a subphrenic ulcer is the presence of a layer of air. A specific symptom of “cups” is with intestinal obstruction.
Treatment
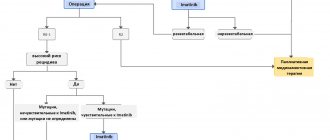
The only truly effective treatment for this pathology is surgery, which is most often performed through wide laparotomy. For local serous peritonitis, it is possible to perform laparoscopic (minimally invasive) surgery. The purpose of the operation is to detect and eliminate the cause of the disease (removal of the appendix in case of appendicitis, suturing of a stomach ulcer, etc.) and to carry out high-quality sanitation of the abdominal cavity.
Rational antibacterial therapy is carried out by intravenous or intramuscular administration of medications in various combinations, thus affecting a wide range of bacterial microorganisms.
An important stage of treatment is infusion detoxification therapy, as well as the prescription of immunomodulators. In especially severe cases, it is important to use hemosorption, hemodialysis and other detoxification methods.
The prognosis for detecting local peritonitis is relatively favorable; this pathology responds well to conservative and surgical treatment with timely diagnosis. The mortality rate in this process is quite low, in severe forms it does not exceed 17%. Preventive measures include timely identification and treatment of pathologies that could lead to this condition.
The Yusupov Hospital brings together specialists from various fields who have achieved significant success in their work. It is these doctors who take an active part in the diagnosis and treatment of patients with serous fibrinous peritonitis. Specialists at the Yusupov Hospital use modern technical innovations in their work to obtain the best results. Close cooperation with European colleagues allows the hospital to remain a leading medical institution in the Russian Federation. Pleasant communication with the medical staff will brighten up your stay in the hospital, and a rich rehabilitation program will allow you to return to your previous lifestyle in a short time. You can make an appointment or consultation with a specialist at the Yusupov Hospital by phone.
Peritonitis treatment. Rusakov V.I. MCPC 1997
All patients with acute peritonitis are subject to emergency surgical treatment in combination with intensive preoperative preparation, correction of homeostasis during surgery and conservative treatment in the postoperative period.
The volume and duration of preoperative preparation depend on the patient’s condition, the severity of dehydration, hemodynamic disturbances and the characteristics of peritonitis (the nature of the main pathological process). With the general satisfactory condition of the patient and normal hemodynamic parameters, preoperative preparation should be minimal: hygienic measures, painkillers and pumping out gastric contents. If the patient does not tolerate the insertion of the tube, gastric decompression can be done on the operating table under anesthesia.
The patient's serious condition, decreased blood pressure, and severe intoxication require intensive but short-term preparation for surgery. The volume and duration of preparation should be determined individually, but when fulfilling the motto, take the patient to the operating table as soon as possible and eliminate the cause of peritonitis. In extremely severe patients who are dangerous to take to the operating table, lengthening the preoperative preparation to two or even three hours will be more beneficial, since it will significantly eliminate dehydration, hypokalemia, hypoproteinemia, hypovolemia, raise blood pressure and improve heart function.
Preoperative preparation should be carried out according to the following plan:
- 1. Immediate administration of 2 ml of a 2% solution of promedol or 2 ml of a 1% solution of omnopon subcutaneously or intravenously.
- 2. Subcutaneous injection of 2-3 ml of 20% camphor oil and 1 ml of 10% caffeine solution.
- 3. Pumping out the gastric contents and leaving the tube constant.
- 4. Hygienic measures, shaving the abdominal wall.
- 5. Intravenous infusion of saline solutions (Ringer's solution) 500-600 ml with ascorbic acid (up to 500 mg).
- 6. Intravenous infusion of protein drugs (transfusion of 200-300 ml of plasma, albumin or immunoglobulin gives a good effect).
- 7. Intravenous infusion of up to 500 ml of a 5% glucose solution with an appropriate amount of insulin under the skin (4 units per 10 g of dry glucose).
- 8. Transfusion of 150-200 ml of freshly citrated blood or oxygenated blood.
- 9. Intravenous infusion of 100-150 ml of 0.5% methyluracil solution.
- 10. In the presence of acidosis, intravenous infusion of 200-300 ml of 4% sodium bicarbonate solution.
- 11. If there is a significant decrease in blood pressure, 50-60 mg of prednisolone or 100-150 mg of hydrocortisone in a 5% glucose solution are administered intravenously.
- 12. Intravenous or intramuscular administration of at least 1,000,000 units. broad-spectrum antibiotics.
- 13. Oxygen therapy.
- 14. Bilateral lumbar novocaine blockade according to A.V. Vishnevsky (especially indicated in the presence of pancreatitis, cholecystitis, intestinal obstruction and severe pain).
- 15. Cold on the stomach.
- 16. Care, constant attention.
During the period of preoperative preparation (in the first minutes of the patient’s stay in the hospital), blood and urine are taken for examination for a more specific correction of homeostasis, which is continued during the operation and in the postoperative period until vital functions are fully compensated and normal indicators are stable.
Once a diagnosis of peritonitis is made, treatment has three main goals:
- 1) elimination of the cause that caused peritonitis;
- 2) abdominal toilet;
- 3) ensuring evacuation of the contents of the gastrointestinal tract.
The surgeon's tactics for appendiceal peritonitis, strangulated hernia, perforated gastric ulcer, intestinal obstruction and a number of other acute surgical diseases of the abdomen are outlined in the relevant chapters. Let us dwell only on the principles of surgical treatment of acute peritonitis.
For diffuse and total peritonitis, the operation should be performed under general intubation anesthesia with the use of muscle relaxants. It is advisable to administer an intravenous infusion of a 0.5% solution of methyluracil, which reduces the negative effect of painkillers on the body, and to turn off the reflexogenic zones with novocaine.
After opening the abdominal cavity, the contents are pumped out and an inspection is performed. The audit must be done very carefully. Exudate is removed with an electric suction and sometimes with gauze pads. Unnecessary damage to the serous membrane, which is very vulnerable to inflammation, should be avoided. Eliminate the cause of peritonitis in the most rational and appropriate way for the patient. Repeat the toilet of the abdominal cavity. It is advisable to fill the abdominal cavity with a 0.8% solution of methyluracil with 1,000,000-2,000,000 units. penicillin or other antibiotic and pump out the contents. This procedure can be repeated 2-3 times.
If the effusion was serous or serous-fibrinous with a small amount of fibrin, then after administration of 150-200 ml of a 0.8% solution of methyluracil and 500,000-1,000,000 units. With an antibiotic, the abdominal wound can be sutured tightly. A permanent tube is left in the stomach. In case of severe paresis, decompression is carried out using long probes that are inserted through the esophagus and stomach into the small intestine, sometimes right up to the bowel valve. The colon is drained through the anus. In particularly severe cases, with diffuse or total purulent peritonitis and severe intestinal paresis, it becomes necessary to perform an enterostomy and apply a cecostomy and drain the small intestine through the bowin's valve. This method provides decompression of the large and small intestines.
The slightest doubt about the smooth course of the postoperative period necessitates drainage of the abdominal cavity. After operations for local peritonitis, it is enough to insert 1-2 thin synthetic tubes and 1-2 strips of rubber gloves. They ensure a good outflow of contents from the abdominal cavity, and the tubes in the postoperative period also serve for the administration (if indicated) of antibiotics and other medications. A good effect is achieved by administering 0.5 g of kanamycin in Ringer's solution three times a day.
After operations for diffuse and, especially, total peritonitis, good drainage of the abdominal cavity is ensured. Gauze swabs cannot be used. They are permissible only in exceptional cases, when it is necessary to isolate an unremovable lesion from the free abdominal cavity and in case of unstoppable bleeding. Synthetic drainage tubes (about 3-4 mm in diameter) and strips of glove rubber are brought to the source of peritonitis, as well as into the side canals of the peritoneal cavity, into the peritoneal sinuses and into the pelvis, making, if necessary, additional incisions or punctures with a trocar in the iliac and subcostal areas . If the exudate was fibrinous-purulent, and even more so with an admixture of feces or urine, these drainage tubes are used to carry out constant washing of the peritoneal cavity in the postoperative period.
Before drainage, the laparotomy wound is sutured in layers with interrupted sutures. We suture wounds in patients with peritonitis, like in all other patients, and do not get suppuration.
Constant washing (irrigation) of the abdominal cavity after operations for severe peritonitis has found very widespread use in the last 10 years. The meaning of this washing is not only to provide a physical and chemical effect on the flora and the inflammatory process, but to be able to regulate homeostasis. Therefore, it is also called peritoneal dialysis.
We will not dwell on the history of the creation of a method of immediate and continuous washing of the peritoneal cavity with various solutions. Much has been written about this in books by A. M. Zabludovsky (1922), Makkal (1928), V. Ya. Shlapobersky (1958) and in many articles in periodicals.
A solid scientific justification for the use of constant lavage of the abdominal cavity for peritonitis was given by Kh. G. Gafurov (1957), who was the first to use this method of treatment: “In case of large contamination of the abdominal cavity with intestinal contents (fecal peritonitis), after eliminating the focus of peritonitis, we recommend the use of long-term abdominal irrigation cavity with a large amount (up to 10 liters) of warm 1% sodium chloride solution.” Kh. G. Gafurov considered it necessary to introduce antibiotics into the abdominal cavity after stopping the lavage. Adding drugs to the liquid used for lavage is completely natural, since this achieves a complex effect on infection, inflammation, and homeostasis.
At the Leningrad Institute of Emergency Medicine, peritoneal dialysis has been used for the treatment of peritonitis since 1963 with the following composition of dialysate fluid: physiological saline solution or Ringer-Locke solution with the addition of 0.002 g of heparin, 10 ml of 1% novocaine solution, 500,000 units. penicillin, 1 g streptomycin and 1 g colimycin per liter of liquid. V. D. Fedorov (1974) adds 1 g of kanamycin to one liter of dialysate fluid and considers (with a consumption of 5-6 liters of fluid per day) this to be sufficient to ensure a therapeutic concentration of the antibiotic in the abdominal cavity and in the blood. However, it is better to complement antimicrobial therapy with intravenous and intramuscular antibiotic administration. V.D. Fedorov comes to this conclusion. V. S. Savelyev et al. (1976) use Ringer-Locke solution for dialysis (4-12 liters per day) with the addition of 0.25 g of kanamycin per liter of liquid.
M. V. Danilenko et al. (1970) highly appreciate the use of dimexide in the treatment of purulent peritonitis, which, according to the authors, has antiseptic, anti-inflammatory, analgesic, anti-adhesive and diuretic effects, and also promotes the passage of drugs through biological membranes. Dimexide is administered before suturing the wound into the abdominal cavity in the amount of 300 ml of a 25% solution mixed with antibiotics.
With peritoneal dialysis, up to 1200 ml of dimexide can be administered per day. O. S. Misharev et al. (1976) use a furagin solution 1: 13000 or a solafur solution 1: 1000 for dialysis. S. L. Freidman, A. N. Khlebnikov (1976) warn about the possibility of complications from nitrofuran compounds. I. I. Deryabin, M. N. Lizanets (1972) recommend changing the composition of the dialysate fluid in order to influence the level of electrolytes and water in the body. It is advisable to add a 0.8% solution of methyluracil and proteinase inhibitors to the dialysis fluid, which should be considered mandatory for enzymatic peritonitis.
The technique of peritoneal dialysis is as follows. After eliminating the cause of peritonitis and treating the abdominal cavity, through additional small incisions or punctures of the abdominal wall with a trocar, three or four synthetic or silicone tubes with a diameter of 0.4-0.5 cm are inserted into both subcostal and iliac regions, placing their central ends with multiple holes on the sides into the deepest parts of the peritoneal cavity. V. S. Savelyev et al. (1974) recommend introducing six tubes: two adductors (in the subcostal areas) and four outlets, two of which are located at the level of the navel under the abdominal wall and two in the iliac areas. The authors give preference to the fractional dialysis method. The tubes are secured to the skin with one or two sutures. The wound of the anterior abdominal wall is sutured tightly or to drains that lead to the source of peritonitis.
Next, dialysis is carried out either by periodic (3-4 times a day) injection into the abdominal cavity of dialysate fluid in a volume of 500-2000 ml mixed with antibiotics for 1-2 hours or by constant lavage with a flow rate of 3-4 to 10 liters of fluid per day . You can combine fractional dialysis with constant dialysis, accordingly changing the composition of dialysis fluids and the concentration of antibiotics. V. D. Fedorov (1974) established that massive lavage of the abdominal cavity is possible with a consumption of at least 5-6 liters of fluid per day.
Dialysis fluid is administered through one of the tubes at a rate of 60-100 drops per minute. The solution flows out through the other 2-3 tubes. If there is difficulty in the inflow or outflow of fluid, the purpose of the tubes is changed. The operation of the flushing system requires constant monitoring. Fluid retention in the abdominal cavity can cause a temporary cessation of its flow. Peritoneal dialysis must be carried out with constant monitoring of the main indicators of homeostasis and, accordingly, change the composition of the dialysate fluid, its osmotic pressure and the intensity of lavage.
Otherwise, you can harm the patient by washing away electrolytes, proteins and water from the body or, on the contrary, oversaturating with salts and causing overhydration. The proposal of R. T. Panchenkov, I. V. Yarem, B. M. Urgaev (1976) to use lymph dialysis for severe forms of peritonitis is tempting.
Peritoneal dialysis is continued from 2-3 to 5-7 days. Constant irrigation should be stopped as soon as the patient’s condition improves, the pronounced symptoms of peritonitis disappear and the main indicators of homeostasis are normalized.