Ascites is a pathological condition in which fluid accumulates in the abdominal cavity. The reasons for it are different. The most common cause of ascites is cirrhosis of the liver. It also occurs as a complication of oncological diseases, while the patient’s condition worsens and the effectiveness of treatment decreases.
- What types of cancer can cause ascites?
- Why does cancer cause fluid to accumulate in the abdomen?
- Manifestations of ascites in cancer
- What complications does ascites lead to?
- Diagnostic methods
- Treatment of ascites in oncology
- Prognosis for ascites in cancer patients
- Prices
Some numbers and facts:
- In the early stages of cancer, moderate ascites develops in approximately 15–50% of patients;
- Severe ascites develops in approximately 7–15% of cancer patients;
- With ascites, up to 5-10 liters of fluid can accumulate in the abdominal cavity, in severe cases - up to 20 liters.
Why does cancer cause fluid to accumulate in the abdomen?
In liver cancer, the causes of ascites are the same as in cirrhosis (in fact, liver cancer in most cases develops against the background of cirrhosis): impaired blood outflow, increased pressure and congestion in the veins, impaired albumin synthesis and a decrease in oncotic pressure of the blood.
In case of malignant tumors of other organs (stomach, intestines, uterus, ovaries), ascites occurs due to damage to peritoneal cancer cells. Because of this, fluid absorption is impaired. If tumor cells invade the lymph nodes, ascites may occur due to impaired lymph flow.
Dangers
Pulmonary edema is life-threatening. Oxygen starvation develops in the lung tissues, and they can no longer cope with their function.
If the disease is not treated, serious complications can occur that threaten vital systems.
Possible complications include:
- Pressure jumps;
- Airway obstruction;
- Difficulty and depressed breathing;
- Extreme increase in heart rate;
- Fulminant swelling, which can be fatal.
Timely treatment can save you from such complications.
Manifestations of ascites in cancer
If a small amount of fluid accumulates in the abdominal cavity (100–400 ml), there are no symptoms. In such cases, ascites is often discovered accidentally during an ultrasound or CT scan of the abdominal organs.
Gradually, as ascites increases, the abdomen increases in volume. The patient feels heaviness in the abdomen, aching pain. Due to fluid retention, body weight increases. Compression of the internal organs occurs, and symptoms of abdominal ascites such as nausea and vomiting, belching, upset bowel movements and urination occur. The appearance of the navel changes: it bulges, as during pregnancy. The patient feels weak, constantly tired, and his appetite decreases.
What complications does ascites lead to?
With severe, long-term ascites, fluid accumulates in the pleural cavity, and hydrothorax develops. This leads to even greater respiratory distress and severe shortness of breath.
*By analogy with the abdominal cavity, in the chest there is a thin membrane of connective tissue - the pleura, the parietal layer of which lines the walls, the visceral layer covers the lungs.
With portal hypertension, microorganisms from the intestine can penetrate the ascitic fluid. Spontaneous bacterial peritonitis develops. The situation is aggravated by the fact that there are few antibodies in the ascitic fluid, so the immune response is weak.
A rare but very serious complication of ascites is hepatorenal syndrome. In this case, cirrhosis and liver failure lead to serious impairment of kidney function, up to severe renal failure. Patients with hepatorenal syndrome live on average from 2 weeks to 3 months. The causes of this condition are not fully known. It is believed that blood flow in the kidneys is impaired due to excessive use of diuretics, intravenous contrast during radiography and computed tomography, and certain medications.
general information
During the oncological process, fluid accumulation in the lungs is sometimes observed. This fact itself may indicate:
- Pulmonary edema;
- Exudative pleurisy;
- Consequences of chemotherapy.
Let us be clear: the term “fluid in the lungs” itself does not exist in medicine. When it is pronounced, the first two of the above states are meant.
If we talk about edema, then the liquid mass accumulates in the alveoli involved in gas exchange. The presence of liquid mass makes breathing difficult.
The accumulation of liquid mass in the alveoli occurs at different rates - for some it happens faster, for others it happens more slowly. This becomes an important aspect, taking into account which edema is classified as acute and chronic.
With pleurisy, excess liquid mass forms in the pleural cavity. These sheets are connective tissue plates that line the surface of the lungs and the inside of the sternum cell. The pleura is usually affected by metastases from a tumor located in other organs.
Pleurisy, as a rule, signals a late stage of oncology. Fluid accumulation occurs in a number of cases:
- The presence of foci of metastasis in the lymph nodes adjacent to the bronchi;
- Overlapping of the bronchial lumen by a tumor;
- The development of pneumonia caused by cancer.
The accumulation of liquid mass can also be a consequence of radiation or chemotherapy treatment.
Sometimes doctors encounter cases where oncology is not the cause of the accumulation of liquid mass. Heart disease, for example, can cause heart failure and cause fluid to accumulate in the lungs.
Diagnostic methods
External signs of ascites become clearly visible when the amount of fluid in the abdominal cavity reaches 0.5–1 liter. The abdomen is noticeably enlarged. When the patient stands, he looks drooping; when lying down, he is spread out, with his sides protruding. Doctors call this picture figuratively “the belly of a frog.”
If during an examination the doctor detects signs of ascites in the patient, he may prescribe the following diagnostic methods:
- Ultrasound, CT and MRI help to diagnose ascites and assess the amount of fluid in the abdominal cavity, the condition of internal organs, detect a malignant tumor, assess the number, size, localization of pathological foci, the degree of tumor invasion into various organs and tissues;
- A biochemical blood test helps assess liver and kidney function, determine electrolyte levels, and the degree of protein reduction;
- A blood clotting test helps identify disorders associated with liver dysfunction (the liver synthesizes some clotting factors);
- Diagnostic laparocentesis is a procedure during which a puncture of the abdominal cavity is performed under ultrasound guidance and a small (about a tablespoon) amount of ascitic fluid is obtained. It examines the levels of leukocytes and erythrocytes, total protein and albumin, glucose, and amylase. Conduct tests for the presence of microorganisms, cytological examination for the presence of tumor cells.
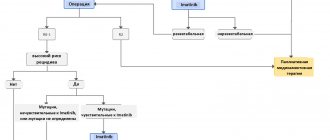
Treatment of ascites in oncology
Treatment of ascites in cancer patients is a complex task. The quality and life expectancy of the patient and the effectiveness of antitumor therapy depend on the correct approach to solving it. Ideally, you need a clinic that specializes in the treatment of ascites in cancer patients.
Conservative treatment
This therapy helps remove up to 1 liter of fluid per day. It significantly improves the condition in approximately 65% of patients. But it can only be used for moderate ascites. Many patients with advanced cancer do not tolerate fluid and salt restriction well. Therefore, conservative therapy is not considered as the main method of treating ascites in oncology.
Laparocentesis
Laparocentesis is a procedure during which a trocar is inserted into the abdominal cavity under ultrasound guidance - a special instrument in the form of a tube with sharp edges (reminiscent of a needle, only thicker) and fluid is removed. Laparocentesis is performed under local anesthesia under sterile conditions, with the patient sitting or lying down during the procedure. The trocar is inserted along the midline of the abdomen or along the line that connects the umbilicus to the ilium. During the procedure, up to 5-6 liters of fluid can be safely removed from the abdominal cavity.
After laparocentesis, the doctor may insert a peritoneal catheter into the abdominal cavity - a tube connected to a reservoir to drain ascitic fluid. With severe ascites, the catheter can be left in place for several days.
Possible complications during and after laparocentesis:
- A drop in blood pressure when a large amount of fluid is removed. To prevent this from happening, the ascitic fluid is removed slowly, and the patient’s pulse and blood pressure are constantly monitored;
- Protein deficiency due to the loss of a large amount of albumin along with ascitic fluid. To combat protein deficiency, albumin is administered intravenously;
- Pain. If necessary, painkillers are prescribed after laparocentesis.
- Fluid that remains after the procedure in some parts of the abdominal cavity. To drain all the fluid, your doctor may place more than one peritoneal catheter in different locations.
- Peritonitis as a result of penetration of microorganisms into the abdominal cavity. A rare complication. For its prevention and treatment, antibacterial drugs are prescribed, and surgical intervention may be required.
- Impaired fluid outflow through the peritoneal catheter. Most often it occurs due to the fact that the end of the catheter is “sucked” to the wall of the abdominal cavity or internal organs. Often, to cope with this problem, it is enough to change the position of the body. If this does not help, the catheter may need to be replaced.
- Fluid discharge after catheter removal. To collect it, a special reservoir is placed at the puncture site for 1–2 days.
- Fusion of the omentum (part of the peritoneum) or part of the intestine with the abdominal wall occurs with repeated punctures. If this causes significant bowel disruption, surgical removal of the adhesions may be required.
Intraperitoneal chemotherapy
Some patients are prescribed intraperitoneal chemotherapy - the chemotherapy drug is injected in high doses into the abdominal cavity, sometimes preheated to 41 degrees (this chemotherapy is called hyperthermic). This helps reduce ascites. Systemic chemotherapy is administered.
One of the new drugs for the treatment of ascites in cancer patients is the monoclonal antibody Catumaxomab. It is also administered intraperitoneally. Catumaxomab interacts with receptors of tumor and immune cells and induces an immune response. But the drug only acts on cancer cells that have certain molecular genetic characteristics.
Surgery
Omentohepatophrenopexy is indicated for some patients. During this operation, the omentum is sutured to the liver or diaphragm. Due to the occurrence of such contact, the absorption of ascitic fluid improves.
Peritoneovenous shunting is used as a palliative surgical intervention. A catheter is installed in the abdominal cavity, which connects it to the venous system. The catheter is equipped with a valve - it opens when the pressure in the abdominal cavity exceeds the central venous pressure. In this case, fluid is discharged into the veins.
Deperitonization of the walls of the abdominal cavity is an intervention during which the surgeon removes sections of the peritoneum, thereby creating additional pathways for the outflow of ascitic fluid.
Other types of surgical treatment are also used.
Why we are our advantages
- In our clinic there is an unshakable rule: only an individual approach to each patient! Treatment methods are prescribed based on the characteristics of your body. If you are recommended for inpatient treatment, comfortable rooms are at your service, and you will always be under the care of the clinic’s specialists. When hospitalized for laparocentesis, the length of hospital stay does not exceed two days. There is also a day hospital for patients. Moreover, in our clinic it is possible to install an abdominal port system, which allows you to remove ascitic fluid as it accumulates, while eliminating the need for repeated punctures. In addition, the installation of a port system from leading manufacturers of medical equipment allows the patient to lead a normal lifestyle, without any special restrictions.
- Treatment is carried out according to the latest methods and standards of European clinics; the medications used in conservative therapy are of the latest generation, causing virtually no side effects.
- Thanks to modern methods of treating ascites, the risk of complications in our clinic is minimized; with timely treatment, the occurrence of undesirable consequences during laparocentesis does not exceed 1%.
- The clinic staff are experienced surgeons of the highest category, among whom there are candidates and doctors of science.
If you or a loved one suffers from ascites, do not delay treatment. Make an appointment, because timely treatment can save a person not only from the symptoms of the disease that affect the quality of life, but also from the risk of developing severe complications.