Types of disease
Rupture (perforation) of the esophagus can be caused by trauma or be spontaneous. Spontaneous rupture of the esophagus is also caused by banquet esophagus or Boerhaave's syndrome. This is a special type of injury in which the walls of a completely healthy esophagus are torn due to intraesophageal pressure. In gastroenterology, perforation of the esophagus and spontaneous rupture of the esophagus differ, first of all, by the reasons for its occurrence.
Esophageal rupture can be complete or partial. In the first case, the entire thickness of the organ wall is damaged, and in the second, one or more of its membranes are damaged.
Causes
If we talk about perforation of the esophagus, it can occur during various therapeutic and diagnostic procedures: tracheal intubation, tracheostomy, cardiac dilatation, surgical interventions in the neck, sternum, abdomen and other medical procedures. Ulcerative and tumor formations, foreign bodies, and chemical burns can also lead to rupture of the esophagus. Damage to the wall of the esophagus is also possible due to penetrating wounds in the neck or chest.
If pressure increases inside the esophagus, spontaneous rupture of the organ wall may occur. The main cause of this condition is severe vomiting, which can occur when drinking large amounts of alcohol or overeating. Most often, a rupture of the esophagus occurs when a person tries to forcibly restrain the urge to vomit. That is why the pathological condition is called “banquet esophagus”.
In rare cases, spontaneous esophageal rupture occurs under the following circumstances:
- straining during childbirth or lifting heavy objects;
- coughing;
- blunt abdominal trauma;
- epileptic seizure.
The risk group includes males over sixty years of age.
Total information
Statistics on the occurrence of esophageal ruptures depend on their origin. Traumatic ruptures can occur at any age, while a violation of the integrity of this organ due to any diseases, due to which its wall weakens, occurs, as a rule, in middle and older working age. The peak incidence falls in the age group from 35 to 45 years. Spontaneous rupture of the esophagus is most often diagnosed in men after 60 years of age.
Males suffer from traumatic ruptures of the esophagus several times more often than females, since they more often choose a traumatic type of activity. With a non-traumatic type of esophageal rupture, there are three men for two injured women.
Children suffer relatively rarely - the walls of their esophagus are quite elastic, so they can stretch and resist traumatic influences from the outside.
note
If a rupture of the esophagus is diagnosed in childhood, this indicates some kind of disturbance in the intrauterine development of the fetus.
Story
Dutch physician Hermann Boerhaave (1668-1738), who first described spontaneous rupture of the esophagus in 1724.
Spontaneous rupture of all layers of the wall of the thoracic esophagus was first described in the world medical literature in 1724 by the Dutch physician, doctor of medicine, full member of the Paris Academy of Sciences Hermann Boerhaave ( Herman Boerhaave, 1668-1738). On October 28, 1723, Hermann Boerhaave was urgently summoned from Leiden to the Grand Admiral of the Dutch Fleet, Baron Jan Gerrit van Wassenaer. Van Wassenaer vomited after eating a large meal during lunch, after which he suddenly experienced severe pain in the left side of his chest and shortness of breath. Upon arrival, Boerhaave noted that the patient had a weak pulse and anuria that persisted despite drinking a large amount of fluid. Later, Boerhaave noted the appearance of areas of swelling of the subcutaneous tissue, upon palpation of which crepitus (subcutaneous emphysema) occurred. On October 29, 1723, 18 hours after the first symptoms appeared, Grand Admiral Jean Gerrit van Wassenaer died.
At the autopsy of Grand Admiral Hermann Boerhaave, he discovered a transverse rupture of all layers of the wall of the esophagus in the lower third of his thoracic region, particles of food taken by the Grand Admiral (roast duck and olive oil), free gas and liquid in the left pleural cavity, as well as signs of purulent mediastinitis . Boerhaave called spontaneous rupture of the esophagus a fatal disease of the esophagus.
Longitudinal rupture of the esophagus, which occurs most often, was first described by I. Dryden in 1788.
The lifetime diagnosis of this syndrome was first made by V. Myers in 1858.
The first case of recovery of a patient with Boerhaave's syndrome was described by NW Frink in 1947, his patient survived thanks to drainage of the pleural cavity. The first successful operation to repair a rupture of the esophagus in Boerhaave's syndrome was performed in the same year by the British surgeon of Australian origin N. R. Barrett (NR Barrett, 1903-1979), who published a report on this topic in the British scientific and medical journal "British Journal of Surgery" .
Causes of esophageal rupture
There are two large groups of causes of esophageal rupture:
- traumatic;
- non-traumatic.
In many cases, with a non-traumatic type of pathology, an external impact was also observed, after which the wall of the esophagus lost its integrity. Spontaneous ruptures “out of the blue” are much less common.
Traumatic causes of esophageal rupture can be:
- external;
- medical.
External causes mean injury in various situations that are not related to the performance of medical procedures.
External injuries to the esophagus can occur:
- at home;
- in production;
- in situations of a criminal nature;
- in case of major disasters;
- during traffic accidents;
- in wartime.
Everyday ruptures of the esophagus are observed infrequently - it is difficult to get injured in everyday life and then rupture the esophagus. Thus, a rupture of the esophagus can occur when falling from a height onto a massive sharp object. As a rule, such injuries are observed when basic safety rules are violated - most often such people experience polytraumas (multiple simultaneous violations of the integrity of various organs, tissues and structures of the human body).
Esophageal ruptures in production conditions occur in the absence of an established labor protection system or when production workers ignore safety rules. This is most often observed in construction conditions.
In situations of a criminal nature, esophageal ruptures occur most often. As a rule, these are injuries from sharp objects - knives, sharpening points, daggers, and so on. Such injuries are most often associated with injury to other structures of the neck, and less commonly, to the chest.
Esophageal ruptures are often detected in people injured in major disasters - natural or industrial. Quite often this is observed among those who, during a disaster, fell under large fragments of various buildings.
note
During road traffic accidents, esophageal ruptures are most often combined with other types of injuries - usually to the head, neck, chest and upper torso.
In wartime, damage to the esophagus can occur due to shrapnel or gunshot wounds.
In some cases, the described disorder occurs during various medical procedures - such ruptures of the esophagus are called iatrogenic. Medical actions that can lead to them are:
- diagnostic;
- medicinal.
Diagnostic procedures during which esophageal rupture most often occurs are as follows:
- esophagoscopy – examination of the esophagus using a fiberscope;
- biopsy - collection of tissue fragments from the esophageal wall if any disease is suspected.
Treatment procedures with possible damage to the esophagus are:
- bougienage is a manipulation during which metal rods (bougies) of various diameters are inserted into the lumen of the esophagus to expand the lumen of the organ;
- opening of abscesses;
- tracheal intubation - insertion of a tube into it, which is connected to a ventilator;
- surgical interventions on the neck, chest and upper abdomen - in fact, any of these can lead to rupture of this organ.
The reasons why the esophagus may rupture during medical procedures are:
- lack of sufficient experience of the medical worker who performs the manipulation;
- individual characteristics of the patient;
- technical difficulties;
- rude actions of medical personnel.
Spontaneous rupture of the esophagus occurs due to its previous pathologies - against their background, the structure of the esophageal wall is disturbed, it weakens, therefore even the slightest external influence can lead to the occurrence of the described disorder. The reasons why the wall of the esophagus becomes weak are:
- previously suffered and treated injuries;
- somatic pathologies;
- congenital disorders.
After previous injuries (stab, cut, laceration, gunshot wounds, as well as burns), a weak location with reduced elasticity is formed in the wall of the esophagus - it is in this place that a rupture occurs.
Among the somatic disorders, the background for the development of the described disorder can be:
- neoplasms – benign and malignant;
- bedsores - a violation of the trophism of the tissues of the esophageal wall, which occurs with prolonged pressure on it from foreign bodies of the esophagus;
- ulcerative esophagitis - inflammation of the wall of the esophagus, accompanied by the appearance of deep defects in it;
- reflux esophagitis is an inflammatory process in the wall of the esophagus that occurs due to the reflux of aggressive acidic stomach contents into its lumen.
Non-traumatic esophageal rupture occurs when intraesophageal pressure increases. This occurs under circumstances such as:
- coughing. The diseases that accompany it predispose to rupture of the esophagus - bronchitis (inflammation of the bronchial mucosa), pneumonia (inflammatory damage to the lung parenchyma) and others;
- severe vomiting. It can occur with such pathologies of the gastrointestinal tract as pancreatitis (inflammation of the tissues of the pancreas), food toxic infection (poisoning after eating food containing a large number of pathogenic infectious agents), acute dilatation of the stomach (an increase in its volume against the background of a weakening of the tone of the gastric wall) and so on.
Some clinicians argue that rupture of a compromised esophagus can occur when straining:
- during childbirth;
- for constipation;
- when lifting weights.
Esophageal rupture: why it occurs and how to restore its mucosa
Esophageal rupture is an emergency condition involving disruption of the integrity of all layers of the esophageal wall with the formation of a perforation defect, which occurs spontaneously or as a result of traumatic injury. The situation is characterized by a sharp pain syndrome behind the sternum, in the epigastric region, radiating to the back, shoulder girdle, and lower back.
The patient requires hospitalization for urgent medical care. The defeat is dangerous due to complications, the development of traumatic shock and fatal bleeding is possible. With late diagnosis, purulent inflammatory reactions occur in the mediastinum, pleural area, septic shock, and toxin poisoning.
Esophageal rupture: reasons for the formation of a through hole
Traumatic perforation and spontaneous rupture of the esophagus have different causes. This is a rare pathology; 1% of all cases occur in the thoracic surgery department. In males, the gap occurs 3 times more often than in females.
In most cases, pathology occurs as a consequence of chronic diseases of the esophageal tube or incorrectly performed medical examinations. Spontaneous perforation occurs as an independent disease in isolated episodes.
A type of esophageal rupture is also a condition called Boerhaave's syndrome (more about it).
Rupture due to trauma
A traumatic lumen in the esophagus can form as a result of therapeutic and diagnostic manipulations:
- fibrogastroduodenoscopy - a method of examining the esophageal tube, stomach, duodenum using a flexible endoscope to assess the condition, the effectiveness of treatment, take a biopsy, remove foreign bodies;
- tracheotomy is an emergency surgical operation to restore air access to the trachea in case of sudden blockage of the respiratory tract;
- bougienage - a medical procedure to expand the alimentary tract with a special probe (bougie), done for stenosis of the esophagus;
- cardiodilatation - artificial expansion of the junction of the cardiac part of the stomach and the esophagus during spasm;
- tracheal intubation - insertion of a special tube into the trachea for artificial ventilation of the lungs when air is obstructed in the respiratory tract;
- surgical procedures in the cervical region, chest, and abdominal organs.
Other types of injury:
- internal burn of the esophagus, including chemicals;
- ulcers or swelling on the walls of the tube;
- stuck foreign bodies inside the cavity;
- penetrating injuries of the chest, neck.
Causes of spontaneous rupture
Factors that provoke spontaneous rupture of the esophagus are associated with disruption of the muscular layer of the esophagus. Changes occur with reflux disease, with drug-induced esophagitis, with ulcers as a result of infection in AIDS patients.
- increased vomiting after eating, drinking liquid or alcoholic beverages - intraesophageal pressure rises to 200 mmHg;
- repeated gag reflex with impaired functions of the vomiting center in the brain;
- increased intra-abdominal, then intra-esophageal pressure - a condition that occurs during lifting heavy objects, straining during defecation, straining during childbirth, as well as uncontrollable coughing, epileptic seizures, and blunt trauma to the abdominal area.
Banquet rupture of the esophageal mucosa
The reflux of stomach contents or gases into the esophagus causes an increase in internal esophageal pressure. Perforation occurs in its weakest area, which is located on top of the diaphragmatic ring. This circumstance occurs when restraining the gag reflex at the table while eating. This pathological condition is called banquet esophagus.
Perforated damage in the esophagus can be complete, when all layers of the wall are affected, and incomplete, with damage to one or more membranes.
Esophageal rupture: symptoms
Perforation of the cervical portion of the esophagus threatens purulent inflammation of the fatty tissue of the neck ( cervical phlegmon ). A rupture in the thoracic region is often accompanied by inflammation of the mediastinum ( mediastinitis ), cardiac sac ( pericarditis ), and serous pulmonary membranes ( pleurisy ). A complete tear of the abdominal esophagus is dangerous due to the occurrence of an inflammatory process of the peritoneum ( peritonitis ).
The clinical picture of the rupture does not depend on the location and occurs with a gradual increase:
- state of shock;
- toxic damage;
- pulmonary and heart failure.
Immediately after the injury, the patient suddenly feels pain behind the sternum or in the epigastrium, the pain intensifies at the moment of swallowing.
- breathing becomes difficult, shortness of breath occurs;
- the pulse becomes frequent, the pupils dilate;
- face, lips, hands turn pale or blue, sticky cold sweat appears;
- an accumulation of air mass forms in the cervical area - subcutaneous emphysema;
- There may be vomiting of food that has just been eaten, streaked with blood.
When a hollow tube ruptures, errors in diagnosis are possible; a wide clinical variety often simulates another pathology: acute pancreatitis, thromboembolism, aortic aneurysm, perforated duodenal or gastric ulcer, acute infarction.
How is the diagnosis made?
For diagnosis, anamnesis, physical examination, and instrumental measures are used. Palpation reveals emphysema under the skin and tension in the abdominal muscles. A boxed sound is tapped in the lungs percussively, and when listening, weakened breathing is observed.
Survey fluoroscopy
If a rupture is suspected, an X-ray examination of the thoracic and abdominal area is indicated. There are two types of X-ray examinations - with and without contrast.
- X-ray without contrast does not provide complete information about the damage. The images indirectly confirm the perforation; there is a noticeable displacement of the heart muscle and lungs, which occurred as a result of pressure from the air mass;
- An X-ray contrast agent helps provide reliable and complete information about perforation and damage to nearby tissues. A series of images in several projections makes it possible to monitor the passage of fluid through the defective opening into the mediastinum. In order to wash off the contrast from the walls after the procedure, the patient is given a few sips of warm water to drink.
Next, the patient is sent to the endoscopy room to identify indications for endoscopy . The doctor carefully studies the entries in the medical record, compares them with complaints, and finds out contraindications, since the procedure is not safe. Information is needed to select the method of endoscopy and anesthesia suitable for the patient. The essence of the examination and the rules for conducting it are explained to the person.
To determine the exact location and size of the hole, and at the same time to perform surgery, a rigid endoscope is used. Sanitation of the false opening into the mediastinum is done, the cavity is freed from food debris, pus, and contrast.
CT scan
Detects the presence of gas and mediastinal abscesses, the location of air accumulation, and determines the fluid level. The procedure helps to establish the exact location of the rupture, its width, length, direction of the fistula, and type of communication with other structures.
Ultrasound examination
Using ultrasound, the pleural and abdominal areas and internal organs are examined. The method makes it possible to determine the presence of a liquid component in the cavity of the pleura, peritoneum, in the space under the lungs or under the diaphragm.
Esophageal rupture: consequences
The leading role is given to surgical intervention, which solves several problems. The perforated defect is eliminated by suturing the gap, followed by suturing and sealing. During the operation, the issue of providing enteral nutrition is resolved - the probe is inserted into the stoma through the anterior abdominal wall.
Stimulators of esophageal regeneration can alleviate the condition.
Useful video
Sometimes the esophagus ruptures when vomiting. You can learn about restoring the digestive system in this video.
Development of pathology
The mechanism for the occurrence of a rupture of the esophagus, which is traumatic in nature, is simple - under the influence of a traumatic force, the integrity of the esophageal wall is disrupted. Such gaps are usually extensive.
With spontaneous ruptures, changes in the wall of the esophagus can progress over many years. Such damage can be limited - in this case, a through defect is formed in a limited area of the esophageal wall.
Depending on the characteristics, the following types of esophageal rupture are distinguished:
- by quantity – single and multiple;
- by the presence of complications - with or without them;
- in shape – linear, with torn edges;
- by degree - incomplete (only some layers of the esophageal wall are damaged), complete (a through defect in the esophageal wall is formed);
- in size – from 0.7 cm;
- by localization - can occur anywhere in the esophagus. The weakest location is the supradiaphragmatic area of the esophagus - its damage, according to various sources, accounts for about 70-80% of spontaneous ruptures.
Epidemiology
Spontaneous ruptures of the esophagus are a rare disease; they account for 2-3% of all cases of esophageal injury. Among all patients of the specialized department of thoracic surgery, spontaneous ruptures of the esophagus are detected in 0.25%. They most often occur in men over 50 years of age. 40% of the patients abused alcohol. The medical literature describes isolated cases of spontaneous rupture of the esophagus in newborns (I. Aaronson et al., 1975), but this disease practically does not occur in children over one year of age and adolescents.
Symptoms of esophageal rupture
The clinical picture of esophageal rupture consists of symptoms:
- local;
- general
The main local signs of the described pathology are:
- pain;
- swallowing disorder;
- increased secretion of saliva.
Characteristics of pain from esophageal rupture will be as follows:
- by localization - in the area of violation of the integrity of the esophagus. These can be locations from the place of “connection” of the esophagus with the pharynx to its entry into the stomach;
- by distribution - irradiation into neighboring areas is observed. When the abdominal part of the organ ruptures, the patient may feel as if his entire abdomen hurts;
- by nature – cutting, twisting;
- in terms of severity - as a rule, strong, which is associated not only with a violation of the integrity of the esophageal wall and irritation of the nerve endings, but also with the release of the contents of the esophagus into the surrounding tissues;
- by occurrence - in case of injury, they appear at the moment the damage occurs; in case of non-traumatic rupture, they may precede it for some time. The pain intensifies with any active actions - coughing, bending, turning the head, and so on.
Impaired swallowing is observed not only due to the fact that food, when passing through the esophagus, “falls” into the resulting defect - the walls of the organ convulsively contract in response to injury, which leads to its spasm.
note
Increased secretion of saliva during rupture of the esophagus is of a reflex nature.
Violation of the patient’s general condition occurs somewhat later than local symptoms. As a rule, it is associated with the entry of non-sterile contents of the esophagus into the tissue. The symptoms will be:
- hyperthermia – increased body temperature. Can reach 37.8-38.7 degrees Celsius;
- increased breathing;
- increased heart rate;
- severe general weakness;
- malaise;
- a sharp decrease in working capacity - physical and mental.
General symptoms of esophageal rupture progress rapidly, and the patient’s condition can literally worsen before our eyes.
Etiology and pathogenesis
A predisposing factor for spontaneous rupture of the esophagus may be changes in the muscular layer of the esophageal wall (drug-induced esophagitis, peptic ulcer of the esophagus against the background of gastroesophageal reflux disease, infectious ulcers in patients with AIDS), and the immediate cause is a sudden increase in pressure inside the esophagus with a closed pharyngeal-esophageal sphincter in combination with negative intrathoracic pressure, which occurs in the following pathological conditions:
- intense vomiting after a heavy meal, liquid and/or alcohol consumption (pressure in the stomach during vomiting can increase to 200 mm Hg), as well as with eating disorders such as bulimia;
- repeated vomiting due to dysfunction of the vomiting center at the bottom of the fourth ventricle of the brain;
- an increase in intragastric and then intraesophageal pressure when lifting heavy weights, straining during bowel movements, intense coughing, childbirth, or an epileptic attack.
A conscious desire to prevent vomiting in a public place, for example at a banquet table (“banquet esophagus”) can contribute to a sharp increase in intraesophageal pressure.
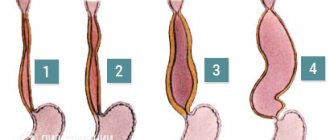
The typical location of a rupture of the esophagus in Boerhaave's syndrome (marked by an arrow) is the left wall of the lower thoracic esophagus directly above the diaphragm. Designations: 1 - thoracic esophagus, 2 - diaphragm, 3 - abdominal (abdominal) esophagus, 4 - stomach
Diagnostics
The diagnosis of esophageal rupture is made based on the patient’s complaints, anamnesis (history) of pathology, and the results of additional research methods (physical, instrumental, less often laboratory).
The anamnesis reveals the following:
- whether the patient has previously suffered from any diseases of the esophagus;
- if this violation is traumatic in nature, then the circumstances of the injury are clarified.
On physical examination the following is noted:
during a general examination, the patient’s general condition is of moderate or severe severity, the skin and visible mucous membranes are pale, often with a cyanotic (bluish) tint, the tongue has reduced moisture, and is covered with a white coating. The doctor notes the casualty's shallow breathing and the appearance of sweat;- upon local examination, when the esophagus is ruptured in its cervical part, tissue swelling is noted - this is emphysema, which refers to the penetration of air (in this case from the esophagus) into the tissues of the neck. If a rupture of the esophagus occurs in the abdominal part, then upon examination it may be revealed that the upper parts of the abdomen do not take part in the act of breathing;
- upon palpation (palpation) - pain is noted in the affected area; if the cervical part of the esophagus is ruptured, crepitus (tissue crunching) is detected, which occurs due to emphysema; if the abdominal part of the esophagus is ruptured, tension of the abdominal muscles in the epigastrium and pain there are determined. If breathing is impaired, then palpation confirms the presence of cold sweat;
- with percussion (tapping) - in the event of a rupture of the thoracic part of the esophagus above the lungs due to pneumothorax, a percussion sound occurs, as if someone is knocking on a box or other hollow object;
- during auscultation (listening) - with a rupture of the thoracic part of the esophagus, sharply weakened breathing is heard, with a rupture of the abdominal part - a weakening of peristaltic intestinal sounds.
The indicators of central hemodynamics that are affected are:
- tachycardia - increased heart rate;
- hypotension – decreased blood pressure.
Of the instrumental research methods in the diagnosis of esophageal rupture, the following are carried out:
- X-ray examination of the chest organs - used if a rupture of the thoracic esophagus is suspected;
- plain radiography of the abdominal organs - it is carried out if a rupture of the abdominal part of the esophagus is suspected;
- bronchoscopy – performed for the purpose of differential diagnosis if bronchial pathology is suspected;
- esophagogastroscopy is the most informative method, during which, using a fiberscope (a type of endoscopic equipment), the esophagus is examined from the inside, during which damage to the esophageal wall is detected;
- diagnostic laparoscopy – used in controversial cases of suspected rupture of the abdominal esophagus;
- Ultrasound examination of the abdominal organs - carried out for the purpose of differential diagnosis in case of damage to the abdominal segment of the esophagus.
This is a basic set of research methods. Other methods may be required, the advisability of which depends on the integrity of which part of the esophagus has been compromised.
Laboratory methods are not very informative and are prescribed to a specific patient according to indications.
Differential diagnosis
Esophageal rupture is one of those disorders that require differential diagnosis with a number of very diverse diseases and pathological conditions. This is due to the proximity of the esophagus to various organs and tissues, which include various functional systems - primarily digestive, cardiovascular and respiratory.
Most often, differential diagnosis of the described disorder is carried out with such pathologies as:
- coronary heart disease (CHD) – oxygen starvation of the myocardium (heart muscle), which develops due to damage to the coronary arteries (vessels supplying the myocardium);
- myocardial infarction – necrosis of its area, which occurs due to the sudden onset of severe oxygen starvation;
- purulent mediastinitis – purulent-inflammatory lesion of the mediastinum (a complex of organs located between the lungs);
- dissecting aortic aneurysm - a violation of the structure of the aortic wall, in which blood flows between its layers;
- perforated gastric ulcer – the occurrence of a through defect in the wall of the stomach at the site of development of the ulcer;
- pancreatic necrosis – necrosis of the parenchyma (working tissue) of the pancreas, which occurs when simultaneously ingesting a large amount of fatty foods and alcoholic beverages;
- cardiac tamponade - release of a large amount of blood into the heart sac followed by compression of the heart;
- tracheal rupture – violation of the integrity of its wall;
- bronchial rupture – violation of the integrity of the bronchial wall;
- spontaneous pneumothorax is a sudden rupture of lung tissue with the release of air into the pleural cavity.
Consequences of esophageal rupture
The consequences of esophageal rupture are divided into two groups:
- non-infectious;
- infectious.
Non-infectious complications include:
bleeding;- hematoma - accumulation of coagulated blood in the soft tissues of the neck or mediastinum;
- subcutaneous emphysema - swelling of soft tissues due to air that entered them through a defect in the esophagus;
- fistulas are a pathological communication between the esophagus and other structures. Most often, such a fistula is “blind” - it ends in the soft tissues. Bronchoesophageal fistulas are also often diagnosed;
- pneumothorax - entry of air into the pleural cavity;
- hemothorax is the presence of blood in the pleural cavity.
Infectious complications are a more numerous group of consequences in case of esophageal rupture. Most often this is:
- abscess - a limited abscess;
- phlegmon - diffuse purulent lesion of the soft tissues of the neck or mediastinum;
- purulent mediastinitis – purulent-inflammatory lesion of the mediastinum;
- pleurisy is an inflammatory process in the pleura (a connective tissue film, one layer of which lines the inside of the pleural cavity, and the other “wraps” the lungs;
- pleural empyema - a purulent process in the pleura;
- pericarditis - inflammatory damage to the pericardium (heart sac);
- peritonitis is an inflammatory lesion of the peritoneum (the connective tissue film that lines the inside of the abdominal wall and covers the abdominal organs). Develops when the abdominal part of the esophagus is damaged;
- sepsis – a generalized spread of infection through the blood and/or lymph throughout the body with its “settling” in various organs and tissues and the subsequent possible development of secondary ulcers;
- meningitis - inflammation of the meninges;
- encephalitis - inflammatory damage to brain tissue;
- infectious-toxic shock - a violation of microcirculation in tissues under the influence of toxic substances (in this case, toxins of an infectious pathogen).
Treatment of esophageal rupture
In most cases, the main treatment method is surgery. They try to delay its involvement if there is a suspicion of a shallow (incomplete) rupture of the esophagus, but it can transform into a complete one, so in most cases surgery is inevitable. During surgery, the esophagus is inspected, the location of the damage is determined, and the integrity of the esophageal wall is restored (suturing the defect). If there is massive damage to the esophagus, plastic surgery will be required. The details of the operation depend on which part of the esophagus was damaged.
Prescriptions in the postoperative period are as follows:
- parenteral nutrition - the patient is given intravenous drips of protein, fat and carbohydrate preparations, since he cannot eat food for some time;
- painkillers;
- dressings;
- antibacterial drugs – for the prevention and treatment of postoperative complications.
Prevention
Measures to prevent esophageal rupture are:
- avoiding situations that could lead to external injury to the esophagus;
- careful, gentle performance of medical procedures on the esophagus - diagnostic and therapeutic;
- prevention, diagnosis and relief of diseases and pathological conditions of the esophagus, which can lead to weakening of its wall - neoplasms, bedsores, esophagitis, and so on;
- prevention, identification and treatment of pathologies from other organs that can also contribute to the occurrence of this disorder - bronchitis, pneumonia, and so on;
- avoiding straining.
Clinical picture
The classic picture of Boerhaave syndrome is characterized by the Mackler triad:
- vomiting of eaten food (in some patients there is an admixture of blood in the vomit);
- subcutaneous emphysema in the cervicothoracic region due to the accumulation of air in the subcutaneous fatty tissue (in 15%-30% of patients);
- severe cutting pain in the chest (less often in the abdomen), suddenly occurring during an attack of vomiting (may resemble pain from a stomach and duodenal ulcer), which can radiate to the left shoulder girdle and left lumbar region and increases with swallowing.
In most cases, the syndrome is manifested by shortness of breath, symptoms of shock (pallor, sometimes cyanosis, dilated pupils, weak pulse, profuse sweat, cold extremities, thirst, feeling of fear), abdominal pain, often in the epigastrium. In the first hours after perforation, pain symptoms of uncertain localization dominate; in some patients with symptoms of an “acute abdomen”, later signs of purulent intoxication, mediastinitis, and pleurisy begin to predominate.
Depending on the clinical and anatomical features, some authors distinguish 2 variants of spontaneous rupture of the esophagus: thoracic (caused by perforation of the thoracic esophagus, clinically manifested by pneumothorax, pneumomediastinum, and later purulent mediastinitis and pleural empyema) and abdominal (caused by rupture of the abdominal esophagus, clinically manifested by picture of peritonitis).
Quite often, diagnostic errors are made with Boerhaave's syndrome: spontaneous rupture of the esophagus, due to the rarity of this surgical disease, the variety of clinical manifestations, often simulating various pathologies of other organs, and the ignorance of most doctors, is mistaken for other diseases, most often for a perforated gastric or duodenal ulcer intestines, less often - acute myocardial infarction, pulmonary embolism, dissecting aortic aneurysm and acute pancreatitis.
Forecast
The prognosis for esophageal rupture varies. If the patient has uncomplicated forms of this disorder, which are quickly stopped, then complete recovery occurs.
The prognosis worsens under such circumstances as:
- late visit to the clinic;
- wait-and-see tactics;
- development of complications.
The mortality rate from ruptures of the esophagus is quite high - according to various sources, out of ten patients, from two to eight die with such a diagnosis.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
1, total, today
( 45 votes, average: 4.62 out of 5)
Biliary dyskinesia - causes, symptoms, forms and treatment methods
Iron taste in the mouth: causes in women and men