A peptic ulcer is a defect in the mucous membrane of the stomach (gastric ulcer) or the initial parts of the duodenum (duodenal ulcer), which penetrates beyond the muscular plate. Almost all ulcers are caused by the bacteria Helicobacter pylori or by taking NSAIDs. Typical symptoms include burning epigastric pain that usually relieves after eating. Diagnosis is made based on endoscopy and testing for Helicobacter pylori. Treatment includes suppression of acid production, eradication of H. pylori (if present), and avoidance of the negative effects of NSAIDs.
The size of the ulcers can range from a few millimeters to several centimeters. Ulcers differ from erosions in depth; erosions are more superficial and do not penetrate beyond the muscular plate of the mucous membrane. Ulcers can occur at any age, including early childhood and childhood, but are most common in middle-aged adults.
Etiology
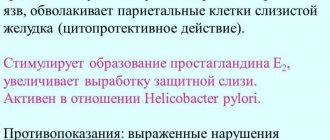
H. pylori and NSAIDs interfere with the normal defense and repair of the mucous membrane, making it more sensitive to acid. H. pylori is present in 50–70% of patients with duodenal ulcers and in 30–50% of patients with gastric ulcers. After eradication of the H. pylori infection, peptic ulcer relapse occurs in only 10% of cases, compared with 70% of relapses in patients receiving treatment aimed only at suppressing acid production. NSAIDs are now responsible for >50% of peptic ulcer cases.
Smoking is a risk factor for the development of ulcers and their complications. Smoking also interferes with ulcer healing and increases the recurrence rate. The risk increases with the number of cigarettes smoked per day. Although alcohol is a strong stimulant of acid secretion, there is no definitive link between small amounts of alcohol and ulcers or delayed healing. A very small number of patients have gastrin hypersecretion caused by gastrinoma (Zollinger-Ellison syndrome).
50–60% of children suffering from duodenal ulcers have a family history.
Diseases with similar symptoms
Perforation of the stomach can be classified under such concepts as “acute abdomen”, therefore this disease must be differentiated from:
- pancreatitis;
- cholecystitis and appendicitis;
- tumor decay;
- renal and hepatic colic;
- thrombosis of mesenteric veins;
- rupture of an aortic aneurysm in the abdominal cavity;
- heart attack;
- pleurisy.
A timely visit to a specialist and carrying out diagnostic measures will help to establish an accurate diagnosis and begin timely treatment of a dangerous disease.
Clinical manifestations
Symptoms depend on the location of the ulcer and the age of the patient; a large number of patients, especially older patients, have few or no symptoms. The most common pain is often localized to the epigastrium and relieved by eating or antacids. The pain is described as burning or gnawing, sometimes like a feeling of hunger. The disease has a chronic and relapsing course. Only half of the patients have characteristic symptoms.
Symptoms of stomach ulcers often do not have a consistent pattern (for example, eating sometimes makes the pain worse rather than better). This is true for pyloric ulcers, which are often associated with symptoms of stenosis (eg, bloating, nausea, vomiting) caused by swelling and scar tissue.
Duodenal ulcers
tend to experience more constant pain. The pain is absent when the patient awakens, occurs in the middle of the morning and is relieved by eating, but returns 2–3 hours after eating. Pain that wakes the patient at night is a common symptom of duodenal ulcers and should be considered as evidence of this disease. In newborns, perforation and bleeding can be a manifestation of a duodenal ulcer. Bleeding may also be the first recognized sign in young children, although repeated vomiting or abdominal pain may be a clue to the diagnosis.
Stomach ulcer
The diagnosis of peptic ulcer can be suspected based on history and confirmed by endoscopy. Empirical therapy is often initiated before a definitive diagnosis is established. However, an endoscopy procedure allows a biopsy or cytological brush scraping to be taken from affected areas of the stomach and esophagus to differentiate between simple ulcers and ulcerative gastric cancer. The incidence of malignant duodenal ulcers is extremely low, so biopsy of duodenal ulcers is generally not justified. Endoscopy can also be used to definitively diagnose H. pylori infection, which should be tested for if an ulcer is detected.
Gastrin-producing tumors and gastrinoma should be suspected in the presence of multiple ulcers, in atypical localization of ulcers (eg, postbulbar), if they are refractory to treatment, or if there is significant diarrhea and weight loss. In such patients, serum gastrin levels should be determined.
Possible consequences
During the previous two stages, a person gradually develops peritonitis. The degree of the condition worsens again: the patient is inhibited, the skin acquires an earthy tint and becomes sticky from sweat. The anterior wall of the peritoneum is tense. The volume of urine produced decreases significantly, sometimes even leading to anuria.
If a patient has an atypical form of gastric ulcer, then perforation is possible into the retroperitoneal tissue. In addition, the hole may be covered by food or surrounding organs. It is possible to limit the process in the presence of many adhesions. There are several types of perforation cover:
- permanent;
- long;
- short-term.
These types of perforation are usually much easier. There are known cases of self-healing.
In addition to peritonitis, hypovolemia, shock and sepsis can complicate the progression of gastric disease.
Complications
Bleeding
Bleeding (moderate to severe) is the most common complication of peptic ulcer disease. Symptoms include hematemesis (vomiting red blood or “coffee grounds”); bloody stools (hematochezia) or black, tarry stools (melena); weakness, orthostatic collapse, fainting, thirst and sweating caused by blood loss.
Ulcerative perforation of the stomach
A peptic ulcer can penetrate the stomach wall. If adhesion prevents leakage into the peritoneal cavity, open penetration does not occur, but limited perforation occurs. In addition, the ulcer can penetrate into the duodenum and penetrate into the adjacent closed space (bursa) or other organs (for example, pancreas, liver). The pain can be intense, constant, radiate beyond the abdomen (usually to the back if the pain is caused by penetration of an ulcer of the posterior wall of the duodenum into the pancreas) and changes with changes in body position. Typically, CT and MRI are needed to confirm the diagnosis. If conservative treatment fails, surgical treatment is required.
Free perforation
Ulcers that penetrate the peritoneal cavity without being limited by adhesion are usually located on the anterior wall of the duodenum or, less commonly, the stomach. The clinical picture of an acute abdomen develops. Epigastric pain is sudden, intense, prolonged, quickly spreading throughout the abdomen, often becoming pronounced in the right lower quadrant, sometimes radiating to one or both shoulders. Usually the patient lies motionless, because even deep breathing increases the pain. Palpation of the abdomen is painful, peritoneal symptoms are pronounced, the muscles of the abdominal wall are tense (like a board), bowel sounds are reduced or absent. Shock may develop, which is indicated by an increase in heart rate, a decrease in blood pressure, and a decrease in urine output. Symptoms may be less severe in older or dying patients or in those taking glucocorticoids or immunosuppressants.
Pyloric obstruction
The narrowing may be caused by scarring, spasm, or inflammation associated with an ulcer. Symptoms include repeated, large volumes of vomiting, more often occurring later in the day and 6 hours after the last meal. Loss of appetite with constant bloating or fullness after eating is also characteristic of gastric outlet stenosis. Prolonged vomiting can cause weight loss, dehydration and alkalosis.
If stenosis is suspected based on the medical history, gastric retention can be confirmed by physical examination, gastric aspiration, or x-ray. If gastric aspirate shows significant retention, the stomach should be emptied and endoscopy or x-ray should be performed to determine the site, cause, and extent of obstruction.
Swelling or spasm caused by an active pyloric ulcer is treated with gastric decompression with a nasogastric tube and acid suppression (eg, intravenous H2 blockers or proton pump inhibitors). Dehydration and electrolyte disturbances resulting from prolonged vomiting or prolonged nasogastric aspiration should be actively identified and corrected. Prokinetic drugs are not indicated. Obstruction usually resolves after 2–5 days of treatment. Long-term obstruction may result from scar formation and is relieved by endoscopic pyloric balloon dilatation. In some cases, surgery is necessary to resolve the stenosis.
Symptoms of the disease
Perforation of the stomach wall has 3 main stages:
- State of shock.
- False prosperity.
- Peritonitis.
The immediate stage of shock occurs during perforation and entry of gastric contents onto the layers of the peritoneum. A person feels an unbearable “dagger” pain that appears in the upper layers of the abdominal cavity, which quickly spreads to the entire abdominal area. Most patients at this point begin to thrash and scream. The overall severity of the condition increases rapidly:
- pressure decreases;
- pulse slows down;
- the skin becomes moist, cold and pale;
- the patient takes a forced position - on his side, with his knees brought up to his stomach.
After a certain period of time (about 7 hours), the pain subsides, and in some cases disappears completely. Abdominal bloating gradually increases, it becomes less tense, and bowel sounds disappear on auscultation. Arterial hypotension persists, arrhythmia begins to appear and tachycardia increases. The stage of false well-being can last up to 12 hours.
Treatment
· H. pylori eradication (if present)
Acid suppressants
Treatment of gastric and duodenal ulcers requires eradication of H. pylori if present.
For duodenal ulcers, it is especially important to suppress nocturnal acid production. Methods for reducing acid production include a variety of medications, each of which is effective, but differs in price, duration of treatment and ease of dosing. In addition, drugs with a mucosal protective effect may be prescribed. Gastroenterological Center
Diagnosis of gastric ulcer disease
Gastric perforation requires an accurate diagnosis, which can only be established based on a correctly collected anamnesis. To diagnose the disease, you must consult a specialist. Gastroenterologists and endoscopists deal with these types of problems.
It is very important to be examined promptly if you suspect that you have gastric perforation. Symptoms should never be ignored, as the advanced stage of the disease can lead to irreparable consequences. Absolutely every patient suspected of having this disease needs to contact an endoscopist and gastroenterologist, especially if there is a probable presence of a closed perforation. At the same time, studies do not show complete data for diagnosis, but they are necessary as part of preparation for surgery.
Gastric perforation is determined in the following ways:
- Survey radiography.
- Ultrasound of the abdominal cavity.
- Esophagogastroduodenoscopy.
- If the diagnosis is complicated and a covered perforation is suspected, laparoscopy is used.
Prevention and prognosis
During perforation, the prognosis is quite difficult, since late diagnosis of this condition sometimes leads to the death of the patient. Among young men, the fatal outcome is about 2-6% (taking into account the clinical picture, time of assistance provided and some other factors); among older people, this rate increases several times.
Prevention of the disease is secondary - it is necessary to promptly diagnose and treat those diseases that could bring the patient to this state.