Hepatic and bile ducts
The liver is the largest and heaviest organ with secretory function.
The weight of the liver is from 1.5 to 2 kg, it is located in the upper right corner of the abdominal cavity, adjacent to the arch of the diaphragm. The liver is the body's building block factory, with an important role in the metabolism and synthesis of blood components, performing the following functions:
- Metabolism of proteins, fats and carbohydrates
- Depot of carbohydrates, fats, proteins, iron, vitamins A, D, E and K
- Enzyme synthesis
- Elimination of toxins
- Blood depot and participation in the utilization of cellular elements and the blood coagulation system.
- Bile production
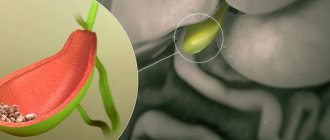
The liver continuously produces approximately 700 ml of bile per day. Bile is collected in the gallbladder, where it is concentrated. When required (after eating a fatty meal), bile is excreted.
The liver is supplied with blood in two ways. The portal vein system drains venous blood from the stomach, intestines, gallbladder, pancreas, and spleen. The portal vein is formed from the splenic vein, inferior and superior mesenteric veins. Venous blood is poor in oxygen but rich in nutrients obtained from the intestines. The hepatic artery supplies arterial blood to the liver. The venous outflow of blood goes from the hepatic artery to the inferior vena cava. The gaps between hepatocytes form bile ducts. The left and right hepatic ducts form the common hepatic duct, which has a branch, the cystic duct, coming from the gallbladder. The common hepatic duct continues as the common bile duct. Together with the pancreatic duct, the bile duct flows through the ampulla of Water into the duodenum. The ampulla of Vater has its own sphincter of Oddi.
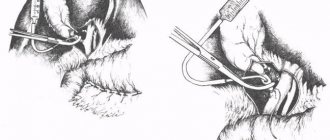
Drainage in surgery
Rice.
1. Schematic illustration of a corrugated elastic drainage strip. Rice. 2. Schematic representation of a multi-channel elastic drainage strip. Rice. 3. Schematic representation of silicone drainage tubes (various diameters). Rice. 4. Schematic representation of multi-channel drainage tubes in cross section. To treat wounds in the times of Hippocrates, Ibn Sina and A. Pare, metal drainages made of silver, copper and tin were used. D. is carried out using rubber, glass or plastic tubes, strips of rubber or specially made plastic strips (Fig. 1), gauze swabs inserted into the wound or drained cavity. Various soft probes and catheters can be used for drainage. The most common are rubber or plastic tubes of various diameters. In cases where it is necessary to introduce antiseptic or medicinal preparations into the drained cavities, or when there are indications for washing the cavities, two- and three-channel tubes are used (Fig. 2-4). To improve the outflow of contents, one or more holes are made at one end of the tube, the number and dimensions of which are determined by the diameter of the tube and the size of the cavity being drained.
Redon drainage tubes, which have become widespread among foreign surgeons, have a length of 50-52 cm with an internal diameter. 3, 4, 5 and 6 mm (with up to 56 holes).
According to physical-mechanical and toxicol. The characteristics and quality of surfaces most fully meet the requirements of drainage tubes made from natural latexes, silicone rubbers and polyvinyl chloride plastics. Polyvinyl chloride tubing has the greatest transparency and is much cheaper than latex and silicone tubing.
When draining surgical wounds, preference is given to tubes made of silicone rubber, which, in their elastic-elastic characteristics, hardness and transparency, occupy an intermediate position between latex and polyvinyl chloride tubes, but significantly exceed the latter in bio-inertness, which allows increasing the length of stay of drainage in wounds. They can be repeatedly subjected to sterilization treatment by autoclaving and hot (up to t° 200°) air.
Rice. 5. Schematic representation of plastic adapters of various shapes for collecting drainage systems.
As a rule, drainage tubes should be made of radiopaque polymer materials, which makes it possible to control the insertion of the tube into the drained cavity and its location in this cavity during the treatment process. To monitor the nature of the released fluid and to facilitate the subsequent change and sterilization of areas of the drainage system located outside the wound, a so-called drainage system is installed in it. control windows made of short glass or plastic tubes - adapters (Fig. 5). The possibility of infection penetrating into the depths of the wound through the lumen of the drainage is prevented by replacing the entire peripheral part of the drainage system with a sterile one twice a day, including graduated vessels for collecting discharge. An antiseptic solution is usually poured into the bottom of the latter (furacilin 1: 5000, diocide 1: 1000, rivanol 1: 1000).
There are a number of requirements for D.:
1. D. should ensure the outflow of fluid throughout the entire period of treatment of the cavity, wound, etc. Loss of drainage can be a serious complication that aggravates the outcome of surgery. This can be prevented by carefully fixing the drainage to the outer skin with a bandage, adhesive tape or silk suture, preferably with a rubber sleeve placed on the drainage tube near the skin.
2. The drainage system should not be compressed or bent either inside or outside the wound. The location of the drains should be optimal, i.e., the outflow of fluid should not be caused by the need to place the patient in a forced position in bed.
3. D. should not cause any complications (pain, pressure sores of tissues and large vessels, etc.). These requirements are fully met by the natural evacuation of liquid from drained cavities through a system of hollow tubes based on the siphon principle. In some cases, forced aspiration of discharge under slight negative pressure is used using water-jet suction, etc. (see Aspiration drainage). A simple method of aspirating discharge using a rubber balloon attached to the drainage was proposed by M. A. Kimbarovsky.
Rice. 6. The position of the patient during drainage of the pleural cavity with a closed drainage system with a two-chamber check valve (the doctor’s hand periodically squeezes the elastic chamber of the cylinder for fluid outflow, the arrow indicates the direction of outflow). Rice. 7. Schematic representation of the Heimlik valve for drainage of the pleural cavity (the arrow indicates the direction of fluid outflow; the valve is located on the right).
For D. of deep purulent wounds and purulent cavities, drainage is introduced into the wound cavity through the main or additional incisions, counter-apertures (see), which are made to ensure better outflow of discharge. To ensure effective D., patients are given a position that facilitates free outflow of wound contents due to gravity. Siphon drainage is used, for example, for D. of the biliary tract. For D. of the pleural cavity, siphon drainage according to Bulau is used (see Bulau drainage). After lung resection and in the treatment of pleural empyema, suction drainage according to Subbotin-Perthes or a water-jet or electric vacuum apparatus is used (see Aspiration drainage). A siphon drainage system equipped with a check valve, used by foreign surgeons, is advisable. The reed type check valve is placed in a clear plastic cylinder with tightly fitting adapters at the ends (Figures 6 and 7). The entire valve device consists of two semi-rigid elastic cylindrical chambers, the front of which serves to initiate the outflow of fluid from the pleural cavity by periodically squeezing its walls with fingers, and the second is the valve device itself, which is convenient to use for drainage using suction devices.
To carry out drainage of the chest and abdominal cavities, in a number of countries trocar catheters are produced from polyvinyl chloride plastic compounds or silicone rubber complete with a trocar stylet for single use (in sterile packaging) or repeated use. These catheters are inserted simultaneously with the trocar into the drainable cavity and connected to a closed drainage system after the trocar is removed. The drained cavity, therefore, is always closed and is not influenced by external pressure. If the puncture is unsuccessful, it can be repeated at another point without any complications, since the smooth distal cone of the trocar stylet, made of stainless steel or light alloys, fits tightly around the catheter and cannot cause additional damage. There are two additional side holes at the distal end of the catheter; the lumen of each of them is equal in area to the lumen of the internal channel.
Trocar catheters are produced in even numbers from 10 to 32 inclusive with a length of 20-40 cm or more; numbers 10-18 are used ch. arr. like children's. To determine the insertion depth, 2-3 divisions are marked on the catheters every 5 cm.
D. is widely used in surgery of the biliary tract, especially D. of the gallbladder and external D. of the common bile duct, which was first performed through the stump of the cystic duct in 1891 by R. Abbe and through an incision in the wall of the common bile duct in 1892 Lane (W. A. Lane). Kerte (W. Korte) used drainage with a side hole, which, along with the external drainage of bile, ensures that part of it enters the duodenum. Ker (H. Kehr) proposed Y-shaped drainages for D. of the biliary tract, Deaver (J.V. Deaver, 1904) - T-shaped drainages. A.V. Vishnevsky in 1925 proposed the original “drainage-siphon-manometer”, in which a drainage tube with a side hole is inserted into the common hepatic duct. E.V. Smirnov (1950), D.L. Pikovsky (1964) recommended after cholecystectomy for decompression of the bile ducts of the common bile duct with thin plastic tubes through the stump of the cystic duct. During reconstructive operations on the extrahepatic bile ducts, Vollcker (F. Vollcker, 1911) used plastic surgery on a rubber drainage, which was brought out through the duodenum. Praderi (R. Praderi, 1961) proposed external transhepatic D. of the hepatic bile ducts (see Choledochoduodenostomy, Choledochostomy, Cholecystogastrostomy, Cholecystoduodenostomy, Cholecystostomy, Cholecystoenterostomy). The introduction of rubber or plastic drains is often combined with the insertion of gauze swabs or the so-called. cigar drains proposed by S.I. Spasokukotsky, consisting of a gauze swab placed in the finger of a rubber glove with a cut end. For better outflow of contents, several holes are made in the rubber shell. “Cigar” drains, unlike gauze swabs, are easily removed without tissue trauma. The use of gauze tampons for D. is based on the hygroscopic properties of gauze, which creates an outflow of wound contents into the bandage. For the treatment of large deep wounds and purulent cavities, I. Mikulich in 1881 proposed the method of D. with gauze swabs, in which a square piece of gauze stitched in the center with a long silk thread is inserted into the wound or purulent cavity. The gauze is carefully straightened and the bottom and walls of the wound are covered with it, after which the wound is loosely packed with gauze swabs. Tampons are changed periodically without changing the gauze, which prevents tissue damage. If necessary, the gauze is removed by pulling the silk thread (see also Tamponade).
D. is also used for the introduction of antibiotics into cavities, as well as for the timely drainage of fluid and contents after surgery on hollow organs in order to prevent the formation of leaks and the development of peritonitis in case of insufficient sutures. For example, after cholecystectomy, rubber drainage and tampons are placed in the subhepatic space so that if the ligature slips off the stump of the cystic duct, bile is drained from the abdominal cavity through the drainage. For the prevention of intestinal paresis after surgery on the abdominal organs and in the treatment of peritonitis, gastric and intestinal dilation with a thin probe inserted through the nostril is widely used, and sometimes intestinal dilation using an enterostomy (see Enterostomy).
D. abdominal cavity - the main method of treatment for delimited ulcers of the abdominal cavity of any location. For diffuse purulent peritonitis, D. is used for peritoneal dialysis (see) or drains are introduced into additional counter-apertures to improve the outflow of discharge from the abdominal cavity.
For the treatment of ascites, edema of the brain, and during reconstructive operations on the extrahepatic bile ducts, internal D. is used. Unlike external D., with internal D. drainage remains in the tissues for the constant outflow of fluid into the subcutaneous tissue or cavities or for the formation of ducts during reconstructive operations. For internal D. in cases of cerebral hydrops, vein autoplasty is used (R. E. Pair, 1911), a tube from the meninges (R. I. Venglovsky, 1913), an omentum, and polyethylene and rubber drainages. Thanks to D., excess cerebrospinal fluid is drained from the cranial cavity or spinal canal into the abdominal, pleural cavity, retroperitoneal space, or left atrial appendage. For ascites, an omentum (see Thalma-Drummond operation) and a bundle of silk threads are used for permanent internal D.; during reconstructive operations on the biliary tract - rubber and plastic drainages.
In some cases, they resort to using the so-called. hidden or forgotten drainages, especially widely used in biliary tract surgery. A hidden drainage inserted into the common bile duct and into the duodenum can, if necessary, be removed using a duodenoscope. Rubber and plastic drainages put pressure on tissues and, with prolonged drainage, can cause serious complications—arrosion of blood vessels, bedsores of the intestine and other organs. Therefore, during D., contact of drains with large blood vessels should be avoided and drains should be removed in a timely manner. The timing of D. is different. Thus, drainage from the abdominal cavity is removed after 7-8 days, from the common bile duct - after 3 weeks. In D. of purulent cavities, drainages are removed after the discharge of pus has ceased and the cavity has decreased or almost completely disappeared.
Why is it necessary to drain the bile ducts?
Percutaneous transhepatic drainage of the bile ducts is necessary for decompression of intra- and extrahepatic ducts in some cases leading to obstruction.
A patient who requires ductal drainage usually has signs of jaundice due to obstruction within or outside the liver, increased levels of bilirubin in the blood and liver tissue, and extravasation into surrounding tissue.
Symptoms include yellowing of the skin and body fluids as a result of increased levels of bilirubin in the blood. A patient with jaundice has gray stool and dark urine. First, the sclera of the eye turns yellow, then the skin, then skin itching begins.
Drainage of intrahepatic bile ducts
Drainage of the bile ducts is a surgical intervention aimed at restoring the outflow of bile when the patency of the intrahepatic bile ducts is impaired. Most often, the causes of such a violation of the outflow of bile are gallstones, which can get stuck in the ducts, or tumor diseases, for example, cancer of the head of the pancreas, liver metastases or primary liver tumors, as well as tumors of the retroperitoneal space. Another rare cause of impaired bile outflow may be cholangitis.
When the outflow of bile is disrupted, biliary hypertension occurs, and the level of direct bilirubin in the blood increases. This leads to intoxication, damage to brain cells and the risk of seizures.
To identify violations of the outflow of bile through the intrahepatic bile ducts, the following non-invasive and invasive diagnostic methods are used:
Ultrasound of the liver and biliary tract
- relaxation duodenography
- endoscopic retrograde cholangiopancreatography
- percutaneous transhepatic cholangiography
- radioisotope liver scan (scintigraphy)
- laparoscopy
These methods make it possible to determine not only the presence of increased bile pressure in the bile ducts, but also to identify the localization of the pathological focus that causes a violation of the outflow of bile.
Among the methods of surgical treatment of obstructive jaundice, drainage of the bile ducts is pathogenetic, that is, it is carried out not to eliminate the cause of jaundice, but to eliminate biliary hypertension.
The choice of treatment for obstructed bile outflow through the intrahepatic bile ducts depends on the cause of biliary hypertension. In order to drain the bile ducts in modern hepatosurgery, the following is carried out:
External drainage of the bile ducts - restoration of bile outflow during obstruction of the biliary system. This is a minimally invasive method that can be used routinely.
Endoscopic cholecystectomy - removal of the gallbladder by an endoscopic (laparoscopic) method, used for gallstones, especially in the case of a “switched off” gallbladder
Endoscopic papillosphincterotomy is a minimally invasive endoscopic intervention in which an incision is made in the area of the so-called. Vater's nipple, through which bile is discharged from the common bile duct into the duodenum.
Choledocholithotomy is a surgical procedure that is usually performed in combination with removal of the gallbladder and usually involves removing stones from the lumen of the common bile duct. Such interventions can be performed, like cholecystectomy, openly or through laparoscopic access.
Percutaneous transhepatic cholangiostomy is a method where drainage of the bile duct is carried out under fluoroscopy or ultrasound control by inserting a long thin needle through the abdominal wall and liver tissue. Using this technique, a special plastic drain is left in the dilated bile duct, which is drained out.
External-internal bilio-duodenal drainage is an operation that has elements of external percutaneous transhepatic drainage of the bile duct, but the drainage tube is placed so that it discharges bile directly into the duodenum, which is more physiological, since it allows bile to participate in the digestion process . With this intervention, a longer drainage tube is used.
Biliary tract stenting is a minimally invasive intervention in which a thin cylindrical stent, which is a wire structure, is inserted into a narrowed section of the bile duct, which restores the lumen of the duct and prevents its re-narrowing.
The main goal of drainage interventions on the bile ducts is to restore the outflow of bile outward or inward into the lumen of the duodenum. Such operations today in leading surgical centers in the USA, Western Europe, Israel, India, Turkey, and South Korea are mostly carried out in a minimally invasive format, which often allows the patient to be discharged home literally the next day. Extensive experience in carrying out such interventions, high qualifications and first-class modern equipment for performing minimally invasive operations on the bile ducts - all this attracts many patients from all over the world, including from Russia to well-known foreign clinics.
Malignant causes
Impaired bile flow due to cancer is most common in elderly patients (often with jaundice).
The general health of this group of patients is often poor. Typically, the tumor is not resectable before symptoms of obstruction occur. The life expectancy of such patients in the absence of treatment ranges from 3 months to 1 year. Palliative treatment for such patients consists of a procedure to relieve the obstruction with a low complication rate, short hospitalization period, and rapid recovery period after the procedure.
Indications
The need for drainage of the bile ducts may be associated with the severity of tissue strictures. The list of indications includes:
- cholangitis, which is accompanied by purulent inflammation;
- acute form of pancreatitis;
- lack of positive results from surgical intervention on the biliary tract;
- damage to the common bile duct area (expansion of the bile duct, taking the form of a sac).
Another indication is impacted stones, which are difficult to remove. Medical drainage of the bile ducts is carried out in the presence of tumor formations.
Intervention can be carried out if there are changes due to ductal hypertension, if intraoperative cholangiography (a technique for examining the common passage in the bladder area) is necessary in the future. And finally, another indication is to monitor the restoration of bile flow into the duodenum.
Endoscopic retrograde drainage of the bile ducts (ERCP).
An endoscope is used for ERCP. This technique is recommended as the initial treatment procedure for distal stenoses. First, the ducts are retrogradely contrasted for diagnosis.
The preferred method for removing bile into the gastrointestinal tract is internal drainage. Therefore, a plastic or metal stent must be placed in the bile ducts using a guidewire. The choice of a plastic or metal stent depends on the type of pathology in the patient. For benign lesions, it is preferable to use a plastic rather than a metal stent due to its lower cost and ease of removal. A metal stent is usually installed for a long time.
How to rinse the gallbladder drainage tube
To ensure optimal drainage of the bile ducts, it is necessary to flush the tubes regularly, following certain rules. At the initial stage, they resort to the help of medical personnel, but in the future care will need to be provided to the patient himself or his relatives.
Flushing the drainage tube involves cleaning it with sterile solutions every day. For this purpose, 0.25% novocaine or saline solution is used in a volume of three to five ml.
Compliance with the rules of care for the drainage tube significantly extends its service life and is the prevention of cholangitis (an inflammatory process in the intrahepatic and extrahepatic bile ducts).
Percutaneous transhepatic drainage of bile ducts
Ultrasound-guided percutaneous transhepatic drainage is performed in cases of proximal stenosis or failure of the endoscopic approach. The access can be used for internal (bile bypasses the obstruction site through the catheter and enters the duodenum) and external (bile is drained and collected percutaneously through the catheter to the outside) drainage. Difficulties with ERCP do not always mean that the percutaneous approach is more difficult or associated with this error.
Since the puncture is usually performed under ultrasound guidance, there is a small risk of complications such as bleeding, pneumothorax, portobiliary fistula. A patient with pre-existing cholangitis is at risk of septic shock if percutaneous drainage is performed. If the patient has ascites, avoid placing percutaneous drainage, as infected bile may enter the ascites fluid.
Two-point technique
Initially, access is achieved using a thin needle (21/22G) blindly puncturing in the direction of the porta hepatis. Under X-ray guidance, the needle is pulled back while contrast material is injected until the needle enters the duct and it is visualized. A certain amount of contrast is then injected into the duct to visualize the biliary tree. In a patient with dilated ducts, the likelihood of imaging is high. The second step is to puncture one of the large intrahepatic ducts with an 18G needle, under X-ray control. Next, a guidewire and drainage can be installed. The two-puncture technique has a greater likelihood of complications than the micropuncture technique (Neff kit).
Micropuncture technique
Before the puncture, the doctor searches for a suitable direction for the puncture using an ultrasound machine. Access to the bile duct is achieved using a Neff percutaneous access kit (21/22G) and placement of a rigid .035”/.038” guidewire. A drainage catheter (eg, an 8.0 Fr pigtail catheter) may then be placed. The catheter can be secured to the skin using the StatLock® attachment. An extension tube and a bag for collecting bile (in the case of external drainage) or a stopcock (in the case of internal drainage) can be connected to the catheter.
Types of drainage and its features
External drainage of the bile ducts in Israel for elderly people is an alternative to surgery. This treatment is a minimally invasive endoscopic decompression procedure that helps restore the flow of bile in cases of bile duct blockage.
The patient is given a probe that removes bile out, eliminating its stagnation. At the same time, if necessary, a chemotherapy drug or a solution with radioisotopes for radiotherapy of oncological diseases can be administered through a probe. If you have chosen drainage of the bile ducts in Israel, you can find out the cost of the manipulation in advance from our consultant. But the exact prices will be announced to you only after a diagnostic examination, when they know exactly the cause of the pathology and the general condition of the body.
Internal drainage of the bile ducts in Israel is carried out based on the patient’s health condition: this procedure helps to establish the correct flow of bile to the intestines, normalize digestion and cure obstructive jaundice.
If you are still in doubt whether bile duct drainage is worthwhile in Israel, reviews from patients at the Top Ichilov Clinic will help you make the right decision.
The drainage of the bile ducts in Israel (prices can be found by leaving a request on our website) takes 1-2 hours - during this time the patient is conscious. Sedatives and painkillers administered intravenously help make the operation painless.
Drainage of the left and right hepatic duct
In the case of distal stenosis, the intrahepatic ducts can be punctured using an abdominal approach, through the anterior abdominal wall (left side of the liver). This avoids complications such as pneumothorax. With this access, the risk of dislocation of the drainage catheter is reduced and the patient's discomfort is reduced. A right approach may be necessary when there is a central obstruction or poor ultrasound visualization of the left lobe of the liver. This requires intercostal puncture, which increases the risk of drainage dislocation, increased discomfort for the patient and a greater risk of bile leakage during ascites.
Bile duct drainage in Israel: cost
When planning treatment abroad, please note that the prices for drainage of the bile ducts in Israel are more than affordable - this procedure in most Western clinics will cost you 30-50% more, while the quality of patient care at the Top Ichilov clinic invariably remains at a high level.
Bile duct drainage in Israel: only positive reviews
Thousands of patients from different countries choose the Top Ichilov clinic due to the optimal price-quality ratio of the procedures performed. The most important advantages of Top Ichilov are:
- high professionalism of the staff;
- the latest diagnostic and therapeutic equipment;
- modern drugs - painkillers, anesthetics - safe for the patient and making any procedure painless;
- well-established infrastructure, since the clinic is located on the territory of the Ikhilov state complex;
- full support by the International Department of all foreign patients who leave only positive reviews about undergoing diagnostics and treatment in our country.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
Internal and external drainage
If it is impossible to immediately pass the obstacle due to stenosis or there are clinical signs of cholangitis, the method of choice is the installation of external drainage. The most suitable catheter for external drainage is the Dawson-Muller Ultrathane® catheter. Depending on the patient's physical condition, an attempt to overcome the stenosis may be repeated after a few days.
Initially, the biliary duct may be so dilated that it is difficult to reach the area of stenosis with the guidewire. If the bile is drained outward for several days, the compression decreases and the duct becomes narrower and the stenosis can be successfully overcome, as the swelling around the stricture subsides. In order to pass the area of stenosis, an Amplatz guide is placed in the drainage catheter and temporary drainage is removed through an introducer with a diameter of 6-8 Fr. Using a manipulation catheter (HNBR ... - BMC, -KMP) and a hydrophilic coated guidewire (such as Roadrunner® or HiWire®) the area of narrowing is overcome. If placement of the drainage catheter over the hydrophilic guidewire fails, the rigid Amplatz guidewire must be reinserted and drainage placed over it. An external internal drainage catheter (ULT ...—CLB-RH) must be installed.
Why biliary endoprosthesis?
If the ductal stenosis can be resolved, it is possible to place an internal biliary drainage (eg Miller set with double Malecot stent: UBSS-10-7.5-MLR) instead of an external or external internal drainage catheter. The placement of a percutaneous drain means more discomfort for the patient and requires more attention and care. There is a risk of bile leakage, infection, and pain in the area of the puncture hole. Therefore, percutaneous drainage is usually quickly replaced with an endoprosthesis (only as a palliative treatment for inoperable cancer).
Result
The main result of drainage of the bile ducts should be considered a decrease in bilirubin levels. Gastroenterologists point out that it:
- Allows you to save the patient from probable death due to hyperbilirubinemia.
- Forms the prerequisites for returning to a restorative course in relation to a pathological condition, for example, surgery or chemoembolization. The same applies to radiofrequency ablation or systemic chemotherapy.
- Allows you to prolong life .
The earliest possible drainage of the bile ducts in inoperable forms of cancer makes it possible to extend the patient’s life by from six months to one and a half years.
Thus, the presented type of intervention should not be ignored, given its effectiveness and low-traumatic nature.
Zilver stent
Instead of a plastic stent, a metal stent, such as the Zilver biliary stent, can be placed percutaneously. The Zilver stent has a delivery device 40 cm long. A metal self-expanding stent is installed for a long time (better patency). Compared to plastic stents for percutaneous installation with a diameter of 12 Fr or more, the thinner delivery catheter of the Zilver stent reduces the likelihood of bleeding in the puncture trajectory, while the diameter of the Zilver stent exceeds that of its plastic counterparts. Migration of the stent is prevented by the mesh structure of the stent, tightly adjacent to the wall of the duct. The first cause of restenosis is the growth of tumor tissue at the edges of the stent, so it is important to choose the correct length of the stent.
Drainage of the area of bifurcations or the area of confluence of the cystic duct occurs through the mesh of the side wall of the stent. The growth of tumor tissue can occur through the mesh and block the lumen of the stent. This does not create a quick problem because the stent lumen is large enough. If the stent is obstructed, you can perform another puncture, access this area and install a second, longer stent inside the old one.
Kinds
There are four types of this surgical intervention: external, external-internal, internal and percutaneous. In the first case, the outflow of the contents of the bladder will occur through equipped conductor tubes to a special receiver.
When introducing external-internal drainage, we are talking about the fact that a significant part of the bile penetrates into the intestinal area through a canal artificially formed by the surgeon. While the remaining contents will be sent to a special receiver located outside.
Internal drainage involves the artificial formation of an endoprosthesis of such a duct, which ensures optimal pumping and removal of bile. Percutaneous drainage of the bile ducts is rated as the least traumatic.
External
It is one of the methods of preparing patients for subsequent surgery.
Experts point out that:
- The intervention is minimally invasive, it does not require specialized training and can be performed on any category of patients.
- The advantages of the technique include the ability to control the penetration of the contents of the gallbladder, purulent masses and blood.
- Through the catheter, the hollow part of the bladder and ducts can be washed with antiseptic compounds. This eliminates inflammatory processes.
- Through special access, which is carried out for the subsequent installation of drainage, it is possible not only to remove stones, but also to excise scars that narrow the ductal lumen.
Objective limitations to external drainage should be considered a violation of the degree of blood clotting, a decrease in platelet counts less than 50 G per liter. The next limitation is not only ascites (the presence of free fluid in the peritoneum), but also an aggravated form of liver failure.
Extensive, numerous metastases of a malignant nature should be considered an obvious contraindication. In addition, we should not forget about the presence of hypervascular tumors in the liver along the path of the catheter equipment.
After surgery, constant monitoring of drainage tubes is strongly recommended. During the first 24 hours, it is recommended to wash the catheter with a special mixture, including saline solution with novocaine or heparin.
Internal
The internal type of drainage of the bile ducts is carried out as a palliative (improving quality of life) treatment for patients with an aggravated form of oncology. In the presented situation, a permanent endoscopic prosthesis is equipped, which ensures optimal flow of bile into the intestinal cavity.
External-internal
The external-internal type of duct drainage is rated as the most effective. With this type of intervention, the patient and surgeon have the opportunity to control the degree of tube patency and flush the drainage with antiseptic solutions.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
In addition, most of the bile will not be excreted, but will penetrate through a specific anastomosis into the area of the duodenum. Thus, we can talk about the cessation of the formation or progression of electrolyte disturbances.
Due to external-internal drainage, we can talk about more successful and complete preparation of the patient for future surgery, if one is to be performed. Most often this is the removal of stones or tumors. In the case of palliative treatment, external-internal drainage can prolong the life of patients for up to 12 months.
Percutaneous
As part of percutaneous drainage, a contrast agent is injected into the intrahepatic bile ducts. Please note that:
- the intervention is performed under local anesthesia in the radiology department;
- is administered intravenously as a preliminary drug preparation ;
- 40-45 minutes before drainage, an antibiotic or a group of drugs is administered.
The percutaneous procedure is low-traumatic. This may be due to the high degree of flexibility of the thin needle, which, being in the puncture area, does not create an obstacle to the patient’s normal breathing.
There are a number of contraindications for such drainage. These are ascites, numerous liver lesions with metastases, hypocoagulation (impaired optimal blood clotting). Another limitation should be considered the inability to perform the procedure due to obesity of the fourth degree.