Failures in the functioning of the liver, the formation and transmission of bile can cause intrahepatic and intravesical cholestasis (cholestatic syndrome). It is very easy to identify this pathology, which causes a lot of problems for pregnant women. It is enough to take a biochemical blood test and undergo an ultrasound of the abdominal cavity.
Comprehensive ultrasound of the abdominal cavity, including ultrasound of the liver and ultrasound of the gallbladder - 1000 rubles.
CLICK TO SIGN UP
When liver tissue is damaged and the oxidation of cholesterol into bile acids is impaired, this is intrahepatic cholestasis. With reduced absorption and evacuation activity of the bladder of a patient with chronic non-calculous cholecystitis, they mean “mild” intravesical cholestasis.
Without proper production of bile, the process of digestion and removal of toxic substances from the body is impossible. One of the diseases of the internal organs or an external negative effect on the body can give impetus to the development of cholestasis.
What is cholestatic syndrome?
The content of the article
The pathology caused by the improper flow of bile into the duodenum and its stagnation inside the liver is called cholestasis. The manifestation of the disease will be shown by a blood test, where indicators of a high concentration of components that should leave the organs along with bile will be visible. An excess of complex components in the liver determines the clinical picture of the disease.
Factors that cause symptoms:
- the intestines contain less bile or none at all;
- the amount of bile that enters the blood is higher than normal;
- components of bile and its toxic metabolites affect liver cells and tubules.
In a healthy person, 80% of copper is excreted from the body with bile. Large accumulations of copper are detected by histochemical examination. The amount of copper is determined by biopsy. Copper binding protein is detected by orcein staining. Such studies provide second confirmation of the syndrome. Accumulated copper during cholestasis does not have a hepatoxic effect on the body, because the copper that enters the hepatocyte is in a non-toxic form.
Cholestasis is manifested by the liver excreting water, the basic ingredients of bile, and tubular flow decreases. With the further development of the disease, hepatocytes begin to enter the bloodstream of those components that the body of a healthy person removes. Therefore, bile is concentrated in hepatocytes, canaliculi, and damaged Kupffer cells. If such a process occurs outside the liver, then the accumulation of bile will be in the liver parenchyma and will also fill the ducts. The dysfunctions caused are reversible when the time interval of the disease is short. Over a long period of time, irreversible damage may occur, characteristic of biliary fibrosis, as well as cirrhosis.
Forms of cholestasis
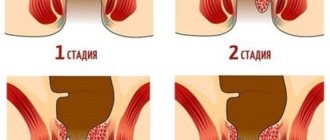
Depending on the place of development and localization of the pathology, cholestatic syndrome can be: intravesical, intrahepatic.
The first type is characterized by bile stagnation, when the extrahepatic bile ducts are blocked, and for the second type, deposits will be in the intrahepatic bile ducts and hepatocytes.
According to the manifestations of jaundice in cholestasis syndrome, there are: anicteric and icteric.
When the color of the skin changes towards yellow, the icteric form of cholestasis is identified. Anicteric cholestasis is considered a prestage of the icteric form. Sometimes the anicteric stage lasts for months; this form of the disease is difficult to treat.
Based on the criteria associated with clinical symptoms, cholestasis occurs:
- acute , when symptoms appear sharply and clearly expressed;
- chronic , when symptoms increase over several months, are not always noticeable and to a weak degree.
Chronic cholestasis can be complicated by the formation of pigmented stones in the biliary tract, accompanied by cholangitis.
If you monitor the destruction of cells, you can distinguish cholestasis with cytolysis and without cytolysis. Cytolysis is considered a violation of the integrity of liver cells. It can occur when exposed to hepatotropic viruses, drugs, and toxic substances.
According to the mechanism of occurrence of the syndrome, cholestasis is distinguished:
- negative , when the amount of excreted bile decreases;
- dissociative , with a delay in the release of certain components;
- total , if the mechanism of passage of bile through the duodenum is disrupted.
Cholestasis during pregnancy
What causes intrahepatic cholestasis in pregnant women is not clear. There are a number of theories that identify the main groups of reasons:
- increased sensitivity to sex hormones of liver cells due to genetic disposition;
- the normal synthesis of enzymes that ensure the transport of bile from cells through the ducts is disrupted;
- the synthesis of bile acids is impaired from birth due to a deficiency of certain enzymes. This disorder can cause the formation of atypical bile acids.
The main changes in pregnant women with the syndrome:
- the amount of bile components in the blood is increased;
- the level of secretion in the duodenum is reduced;
- on the part of bile, there is an effect on hepatocytes and biliary tubules.
Symptoms of the disease in pregnant women, which begin to appear by the third trimester, are irritation and jaundice. In some patients, skin itching can be pronounced and cause a lot of inconvenience, while others tolerate it easily. Intrahepatic cholestasis leads to excoriation of the skin in pregnant women, usually on the arms, legs, and forearms. Symptoms of jaundice appear in only a tenth of women; usually these signs disappear on their own after two weeks after the baby is born. Still, you should not rely on the fact that everything will go away on its own; if you feel any changes in your health, you should consult a doctor, since all the signs can reappear due to hormonal imbalance.
Treatment of pregnant women is complicated by their piquant situation, so non-traditional treatment methods, such as oatmeal masks and chamomile decoction, are used to reduce symptoms. You can even use cold water; it relieves the condition by slowing down the blood flow, so the urge to itch decreases. It is recommended to sleep in a cool room, as well as follow a diet.
Pediatric cholestasis
The causes of childhood cholestasis may be metabolic disorders from birth, consequences of viral diseases, cardiovascular failure, malignant pancreatic tumors, parasitic lesions, genetic predisposition, sclerosing cholangitis.
The manifestation of cholestatic syndrome in children depends on the age at which the disease began and the characteristics of the body. The disease should be treated after the root cause of the disease has been eliminated. For example, if bile stagnation is caused by a malignant neoplasm, then you need to fight the tumor first, and then the symptoms of the syndrome. The child’s therapy is comprehensive: in addition to medications, vitamins A, E, D, K, as well as choleretic drugs can be prescribed.
Often, cholestasis in this group of patients cannot be cured with medications alone; then a surgical operation is performed, which is aimed at removing stones and draining blocked ducts. The danger of cholestasis is that it develops in children in a latent form. To avoid complications and severe forms of the condition, you need to start treatment in a timely manner.
Main signs of cholestasis
Cholestasis is manifested by the following symptoms:
- Skin itches. A primary symptom that may appear on its own for some time. It is characteristic that it is stronger at night than during the day.
- Brown or yellow formations (xanthomas) appear on the chest, back, and elbows.
- Yellow symmetrical formations appear on the eyelids (xanthelasmas).
- Purulent rash, scratching depending on the degree of itching.
- Scratching in different areas, pustular rash.
- There is a change in the color of the surfaces of the eyes, mouth, mucous membranes, and skin to a yellow color (jaundice).
- Melanin levels decrease, the skin becomes dark (hyperpigmentation).
- A large amount of fats is excreted along with feces, due to insufficient processing of them by the body (steatorrhea), feces are characterized by an unpleasant odor, and excrement is difficult to wash off.
- The stool becomes discolored and the urine becomes dark.
- Due to reduced absorption of vitamin K, which dissolves intestinal fats, bleeding increases.
- Changes in metabolism due to stagnation of bile in the liver lead to a lack of vitamins (hypovitaminosis) A, D, E, and a deficiency of component A leads to night blindness - poor twilight vision, dry eyeballs, and skin.
- Body weight decreases.
- Stones may form in the gallbladder and ducts (cholelithiasis).
Why is bile needed?
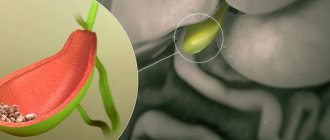
The gallbladder is a bile storage organ. When food enters the body, it releases a portion of bile into the lumen of the duodenum. What exactly is bile for? She:
- dissolves fats into water-soluble fatty acids;
- works as a bactericidal agent - kills dangerous microorganisms;
- neutralizes the acidic pH of gastric juice, which enters the intestines along with the food bolus;
- activates intestinal enzymes;
- stimulates the motility of the gastrointestinal tract;
- promotes the absorption of vitamins, amino acids, cholesterol and other substances;
- removes toxins from the body;
- participates in parietal digestion;
- stimulates the production of hormones that regulate the functioning of the pancreas.
Do not try to straighten the bend in the gallbladder. We tell you how to live with it. There is no diagnosis of a bent gallbladder, but patients persistently strive to straighten their gallbladder. Our article explains why you don’t need to do this.
Causes of pathology
The disease can develop for various reasons. The intrahepatic form of cholestasis is manifested by a smaller flow of bile into the duodenum. This may occur due to hepatocellular pathology. If the tubules are damaged due to damage to the intrahepatic interlobular duct, then the syndrome is called canalicular, as well as extralobular ductular cholestasis, and if hepatocytes are destroyed, then hepatocellular.
Viruses, medications, alcohol, and toxic effects make it difficult for the liver to function normally. Canalicular cholestasis with hepatocellular cholestasis can be caused by any form of liver damage, as well as impaired metabolism and heart problems. The etiology of introlobular cholestasis is in the malfunction of the vacation, basolateral membranes. If the epithelium of the bile duct is damaged, patency is complicated, the composition of bile and acid metabolism are disrupted, then ductular cholestasis develops.
Intrahepatic cholestasis may appear due to factors such as ductopenia, hypoplasia of the extrahepatic and intrahepatic ducts, Alagille syndrome, infection, viruses, exposure to the drug Thiabendazole, cystic fibrosis, sarcoidosis, istiocytosis X, reactions associated with transplant rejection, cholangiocarcinoma, hepatitis, autoimmune deficiency A1- antitrypsin, cholangitis, amyloidosis, congestive liver, circulatory disorders, hepatic vein thrombosis.
Extrahepatic cholestasis begins to manifest itself when the positive effect of the main intrahepatic and extrahepatic ducts is counteracted. One of the common causes is the presence of stones in the bile ducts.
The progression of the extrahepatic form of the syndrome may be due to the presence of stones, malignant neoplasms in the ducts, damage to the duodenum, hepatic artery aneurysm, pancreatitis, malfunction of the pancreas, the appearance of cysts, hemobilia, abscess, parasitic and other infections.
Intravesical cholestasis (mild chronic) can occur in the chronic form of non-calculous cholecystitis, when the activity of the gallbladder decreases - an unbalanced composition of bile is formed.
Why does stagnation of bile develop in the gallbladder?
The most common causes of cholestasis are:
1. The shape of the gallbladder may have changed: it is pear-shaped, there is deformation of the gallbladder, such as constriction, bending of the neck, twisting, and others. This happens from birth or is a way of life.
2. The tone of the biliary tract is affected by stress, neuroses, and the state of the autonomic nervous system. There are two forms of dyskinesia - disturbances in the movement of bile due to the tone of smooth muscles: hypertonic, or hyperkinetic (increased tone of the gallbladder); hypotonic (decreased tone of the gallbladder). These variants of dyskinesia are often combined with hypertension or hypotension of the biliary sphinctors and the sphincter of Oddi, where the common bile duct exits into the duodenum.
3. The tone of the gallbladder is also affected by disruptions in the level of thyroid hormones: hypothyroidism causes lethargy, and hyperthyroidism causes spasms.
4. The amount of plant fiber in food is also the basis for the normal functioning of the bile, but if the food is mainly meat, with a lot of fatty, flour, unnatural products + alcohol, then bile will definitely not be secreted normally. Therefore, stagnation often occurs in people with excess weight and diabetes.
5. Disruption of the liver cells themselves - of course affects the structure of bile. Therefore, by the way, if the gallbladder has already been removed due to stones, this does not mean that now everything will be fine with the bile itself. Thick bile can also produce stones in the liver ducts.
Not the most pleasant result:
Digestion and fat absorption disorders
problems with stool
· formation of a sediment of cholesterol in the gallbladder, then it thickens and stones are formed
· in case of severe liver dysfunction, the stones may be bilirubin or cholesterol stones are impregnated with calcium salts, since bile has an alkaline reaction. Then they can no longer be dissolved.
· the growth of stones further complicates the flow of bile and impairs digestion.
· Stagnation of bile itself certainly does not lead to the formation of atherosclerotic plaques and aging of blood vessels. But if the bile is thick, you can be sure that low-density cholesterol is increased, and high-density cholesterol is insufficient for the formation of energy from it in cells. This is as obvious as smoke means there is a fire somewhere.
· energy deficiency in cells, decreased performance, tendency to excess weight due to improper digestion of fats and excess entry into the blood of heavy cholesterol, bilirubin, and toxins not removed in time.
decreased immunity due to improper digestion, intoxication and energy deficiency
risk of liver damage (hepatitis, cirrhosis) due to intrahepatic stagnation of bile, which has nowhere to be released in a timely manner
You see that bile stagnation creates global risks of accelerated aging of the body and loss of vitality, the risk of surgery for cholelithiasis and simply unpleasant symptoms: heaviness in the right side, discomfort, bitterness in the mouth, abnormal stool.
Should we continue to ignore it?
Diagnosis of intravesical and intrahepatic cholestasis
The media and the Internet should not become sources of treatment for the disease. Only special diagnostic methods reveal pathology, and competent specialists prescribe the necessary treatment.
The patient is physically (externally) examined by a doctor. At this stage, abrasions, rashes, redness, scratching, and icteric skin color may be detected.
Biochemical laboratory experiments and analysis of the concentration of serum bile acids will help diagnose the disease with greater accuracy. If the syndrome is detected, blood biochemistry will show elevated cholesterol, bilirubin, phospholipids, acids, and enzymes.
Patients continue to be evaluated to identify extrahepatic “surgical” cholestasis. It may appear at first glance to be intrahepatic in symptoms.
The next step in diagnosis will be an ultrasound of the abdominal cavity, where an enlarged gallbladder is observed and manifestations of blockage of the bile ducts are identified.
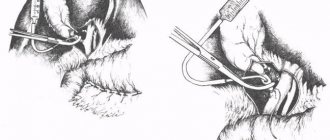
If an increase in the volume of the ducts is detected, cholangiography is prescribed, otherwise the diagnosis is indicated by the clinical picture. For example, if the presence of stones is suspected, then ERCP is performed. When this study does not detect stones, they may be referred for a liver biopsy, but before that the doctor determines the absence of an extrahepatic type.
Biliary obesity
We continue the series of publications by traditional Chinese medicine doctor Vera PASTUSHENKO (Tomsk) about the causes of obesity. As it turns out, not everyone is equally susceptible to this evil. A detailed study revealed that there are distinctive features in people with different types of metabolism and physique.
In the last issue, readers learned about the types of obesity, as well as ways to get rid of excess weight in “meat” people. Among the people of “meat” there are people of “bile”; their increase in body weight occurs according to a special scenario.
Recall that obese people can be divided into three groups. The first group includes people of “meat”, the second group includes people of “fat”, the third group includes people of “dampness”. The body shape can also vary and resemble a triangle, rectangle, pear, hourglass and apple. In accordance with the types of obesity, people with “meat” (Roy Ren) often have the traits of the “Bile” constitution. Why, you ask?
Treatment, prevention of the syndrome
Preventive measures for bile stagnation are aimed at preventing disturbances in the function of the liver and bile ducts. Patients are recommended to walk in the fresh air, light jogging in the morning, race walking, exercises for the abdominal muscles, therapeutic massage, avoidance of harmful alcohol, overeating, and adhere to a strict diet.
The purpose of treatment depends on the form of the syndrome, the stage of the disease, aggravating factors and the characteristics of the organism. Conservative treatment algorithm:
- Diet therapy, correct diet.
- Etiological treatment consists of treating diseases that accompany the development of the disease.
- Basic therapy - ursodeoxycholic acid (UDCA) is prescribed to reduce cholangiocytes damaged by bile acid.
- Therapy aimed at reducing painful manifestations and relieving the symptom of itchy skin.
- Treatment of exacerbations.
If the stage of the syndrome is advanced, then surgical intervention can be used. If treatment is not started in a timely manner, then in such forms the disease can cause irreversible consequences.
Treatment with folk remedies
After consulting with a doctor, you can resort to traditional medicine to relieve inflammatory processes:
- Recipe for a drink made from birch leaves: pour a small amount of leaves into 0.5 liters of boiled water, boil for 10 minutes on fire. You can take 100 ml up to three times a day. Children, pregnant women, and people with acute liver failure should not drink.
- Herbal decoction. Method of preparation: pour boiling water in equal parts of St. John's wort, corn silk, immortelle flowers, 30 minutes. boil on fire. After straining, take the decoction 25 ml up to three times a day half an hour before meals. Use is contraindicated for more than two weeks, as well as for high acidity and stomach problems.
- Nettle and rosehip 10 g and 20 g, respectively, pour 200 ml of boiled water, leave for about an hour. Take twice a day for no more than two weeks. Cannot be used for thrombosis, varicose veins, or individual intolerance.
- Oil remedy recipe: 1 tbsp. Mix honey with 3 drops of mint oil. Application: 3 times a day, no more than 4 weeks. Contraindications: men over 50 years old, with individual intolerance, children, pregnant women and during lactation.
- Lemon oil can be added to drinks 1 drop. Use: up to 2 times a day for no more than 4 weeks. Contraindications: allergies, childhood, pregnancy.
- Beet salad. Take 1 tbsp four times a day. l. Restrictions on use for stomach diseases.
Traditional methods are used only with the permission of a doctor.
Treatment of bile stagnation. Hospital or home?
To confirm the assumption of bile stagnation, liver tests are needed. An abdominal ultrasound examination is also performed, which helps to identify the presence of deposits in the bile ducts or gallstones.
To confirm an accurate diagnosis, test results will be required:
Treatment of cholestasis is carried out simultaneously in several directions:
- fight against bile stagnation
- liver support and healing
- itching relief
To relieve itching, special creams and ointments, antihistamines or corticosteroids are used. In parallel with this treatment, choleretic drugs and drugs responsible for reducing the concentration of bile acids are prescribed.
It is advisable to follow dietary recommendations that include the consumption of essential polyunsaturated fatty acids and fat-soluble vitamins (A, D, E and K).
Stagnation of bile. Treatment of bile stasis with folk remedies
Traditional methods of treatment are acceptable to use, but these are not the main methods for treating bile stagnation. Top 8 folk methods alleviate the patient’s condition:
- performing abdominal exercises and a special massage method
- drinking a decoction based on mint, rose hips, and corn silk
- the use of anti-inflammatory, choleretic herbs: peppermint, buckthorn bark, watch, St. John's wort, wormwood, immortelle
- drink a decoction of aloe, calendula, ginseng, yarrow, mint, coriander
- tubage
- heated unrefined vegetable oil
- eating a piece of lard
- Beet juice will help remove excess bile
Treatment of bile stagnation at home
Bile stasis is treated at home in one of the following ways:
- choleretic herbs
- sunflower oil
- salted lard with garlic
- beet juice
- pumpkin seed
- corn silk
Herbs: immortelle, St. John's wort, dandelion roots, corn silk, rose hips are sold in the pharmacy. Prepare and take according to the indicated recipe.
Take 0.5 cups of sunflower oil warm, then place it on a heating pad and warm the right side. During the day, drink rosehip decoction.
Lard and garlic are eaten without bread, then the right side is warmed on a heating pad, and a rosehip infusion is drunk throughout the day.
Boil the beets until half cooked and squeeze out the juice. Drink in large sips 30 minutes before meals.
Pumpkin seeds are hulled and consumed raw.
Proper diet
Together with drug treatment for a patient with bile stagnation, the doctor creates a proper nutrition menu. Patients exclude spicy, fried, various types of baked goods, canned goods, spices, rich meat broths, and any fatty foods from their diet. The diet is formed from dishes containing vegetables and fruits.
The patient's morning should begin with drinking medicinal mineral water; it is also recommended to consume fermented milk products daily. Eating before bed is prohibited, and during the day you need to eat in modest portions, but often (from five to seven times a day). Without strict adherence to dietary recommendations, cholestasis cannot be cured.
More than half of all food consumed must be heat-treated and served warm. You can eat oat and buckwheat porridge. Please note that you need to cook by steaming, in a slow cooker and in the oven. It is recommended to exclude cold drinks or warm them to room temperature before drinking; to do this, you can leave the drink in a warm room for a while.
What you can and cannot eat if you have bile stagnation
The diet includes rye bread, savory products, honey, and jam. Dairy products include sour cream, cheeses, and curd products (low-fat). Juices and drinks made only from sweet berries and fruits. You can also drink compotes and weak tea. You should eat a lot of greens, vegetables, fruits, and berries. Soups should be vegetable with cereals, pasta, or lean meat: rabbit, veal, chicken, turkey. It is recommended to limit vegetable fats in the diet to 50 g per day.
When dieting, it is prohibited to consume lard, animal fats, soup made from fatty meats and fish. Not all greens are allowed; green onions, sorrel leaves, and spinach should be avoided. You can't have radishes, radishes. As for drinks, alcohol, strong coffee, and any cold drinks are prohibited. Nutritionists also do not recommend canned foods (pickled vegetables, caviar, smoked foods) for consumption. Exclude from the menu confectionery pastries, chocolate, ice cream, spices, mustard, horseradish, sour varieties of fruits and berries.
For treatment, it is very useful to drink skim milk - it is a good source of calcium. When a sign of cholestasis occurs in the form of itching, you need to see a doctor for a liver examination; this symptom may appear much earlier than others; it should not be ignored, because delays often lead to liver failure. Treatment started in a timely manner can relieve symptoms and improve liver function.
If you find an error, please select a piece of text and press Ctrl+Enter
Diet for bile stagnation
There is a very short recipe, and it is the most effective. Food for biliary dyskinesia should be as simple as possible. During the day, a maximum of vegetables, porridge and a minimum of fatty and floury foods, limit smoked foods, products with preservatives and a flavor enhancer - glutamate. For sluggish gallbladder, you can use spices, but this does not mean that chili peppers are good for the liver. Everything is in moderation.
Coffee and strong tea - only in the morning. Alcohol - without zeal.
Food must contain plant fiber. Therefore, using the NutriDetox green smoothie is very convenient. It can be alternated with Svobodium. You perform a daily cleanse and maintain perfect digestion without any effort.