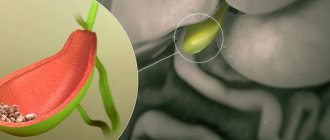
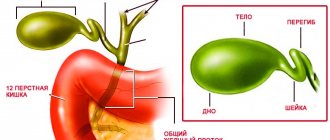
The gallbladder is a small pear-shaped organ located under the liver. It accumulates and concentrates bile, which is produced in the liver and helps the body absorb fats.
When eating foods containing fats, the gallbladder is emptied, sending bile through a channel called the bile duct - common bile duct. The bile duct conducts bile into the duodenum, where it participates in digestion.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
Who needs to have their gallbladder removed?
The most common reason for gallbladder removal is cholelithiasis, that is, the presence of stones in the bladder with chronic inflammation of its wall. Stones can form for many reasons, for example:
- in people with obesity,
- in case of hormonal imbalance,
- for rapid weight loss.
Long-term gallstone disease increases the risk of gallbladder cancer, blockage of the ducts of the liver and pancreas by stones, which can lead to death. The doctor assesses the person’s condition, indications and contraindications for surgery - and based on this, a decision is made on the need for surgical intervention.
Gallstones are an indication for cholecystectomy.
A case from the practice of gastroenterologist Daniela Purgina, an expert on the website Pokhmelye.rf.
Gallstone disease is such a common disease that it is difficult to single out just one case. It occurs in patients of any age, although it is predominantly found in those over 25 years of age. Probably the most interesting case is a patient who was 3 years old when he came to see me. Yes, yes, even at this age gallstones can occur. In his case, this was due to an operation on the intestines, as a result of which the circulation of bile acids was disrupted.
Another reason for removing the gallbladder may be formations inside it: polyps, tumors. Gallbladder polyps are a common finding on abdominal ultrasound.
The gallbladder should be removed only in extreme cases, such as:
- large polyp size or rapid growth,
- suspicion of gallbladder cancer,
- a large number of polyps.
It happens that the gallbladder is turned off from the digestive system: simply put, it stops working. This can happen due to gallstone disease or other reasons. In this case, it also needs to be removed: it no longer performs its functions, but only serves as a dangerous source of inflammation in the body.
It is extremely rare that the gallbladder can be removed due to long-standing bladder dyskinesia that cannot be treated with medications. Impaired motor function of the gallbladder, sometimes accompanied by severe pain in the right hypochondrium, comparable in intensity to hepatic colic, can bother you for years. However, medications do not always bring relief or have an incomplete effect. In this case, the doctor may suggest cholecystectomy. In Russia, such treatment tactics are not yet being considered, but they are already being used in European countries.
Advice from an expert on the website Pokhmelye.rf, gastroenterologist Daniela Purgina.
Discuss further tactics with your gastroenterologist. Not all situations require immediate surgical intervention. In some cases, it is possible to observe or even dissolve stones with the help of medications - all these issues require an individual solution. If you and your doctor decide to take a wait-and-see approach, be sure to follow the recommendations regarding diet. Fatty, fried, spicy foods and alcohol can cause exacerbation of cholelithiasis.
Preparation for surgery
Removal of gallstone
, which can be performed laparoscopically or abdominally, requires some preparatory procedures. So, the patient undergoes tests:
- urine;
- blood (general and biochemistry);
- for syphilis and hepatitis.
The patient also does:
- ultrasound examination of the abdominal organs;
- fluorography;
- ECG;
- colonoscopy;
- fibrogastroscopy.
You definitely need to see a therapist who will give you a referral to a hospital.
Repeated blood tests and an ECG may be required in the hospital. If the pathology is complex, a repeat ultrasound examination is prescribed. The patient is announced the date of the operation.
6 hours before it is forbidden to eat or drink. A cleansing enema is prescribed 3-4 hours in advance.
Contraindications to cholecystectomy
Usually there are absolute and relative indications for any operation. The doctor must assess the risk to the patient before and during organ removal.
- Surgery is absolutely contraindicated for people with severe acute and chronic diseases in which removal of the gallbladder would lead to death.
- Relative contraindications include those health problems that can make the postoperative period more difficult and prolonged, and cause complications. However, the consequences of these diseases can be foreseen and influenced: for example, normalizing blood pressure in patients with hypertension, glucose levels in people with diabetes.
What to do if surgery is contraindicated and stones need to be removed? For such cases, there is a procedure for non-surgical stone crushing. Why, then, is this procedure not performed on everyone who suffers from cholelithiasis? At the moment, it shows little effectiveness, it has many contraindications and risks, and usually it ends with the patient having the entire bladder removed anyway. For more information about how this procedure is carried out and why doctors do not favor it, read the article about crushing gallstones.
In some cases, you can try to dissolve the stones using Ursosan or other ursodeoxycholic acid preparations. Not all stones can be dissolved: this depends on their composition, size and other factors. Read about the cases in which it is possible to use tablets, what the disadvantages of this method are, and whether it is possible to dissolve stones using traditional methods in the article about litholytic therapy.
An expert on the website Pokhmelye.rf, gastroenterologist Daniela Purgina, warns about a common mistake.
What I strongly do not recommend to you is to try to dissolve the stones yourself using folk remedies. It just doesn't work! If it worked, we would prescribe this treatment to patients ourselves. The most common recipe is lemon juice with olive oil; as a result of taking them together, you may see stone-like formations in the stool, and you will think that they came out; but in fact, in the body, under the influence of enzymes, a saponification process simply occurred and you produced soap within yourself. Only very small stones or sand can come out, but even trying to expel small stones is dangerous, because they can get stuck in the bile duct or get into the pancreatic duct, and this can lead to the development of pancreatitis.
How much does gallbladder removal cost?
Russian citizens under a compulsory health insurance policy (CHI) have the opportunity to undergo free planned removal of the gallbladder. Details should be obtained from doctors at your place of residence. It usually takes time for the state to allocate money (quota) for such an operation.
In some cases, surgical intervention can be performed under voluntary health insurance (VHI) or for a fee, which often happens when the patient does not want to wait in line for planned hospitalization.
In case of complicated cholelithiasis requiring hospitalization in the surgery department, the operation is performed free of charge and in a short time. But this does not mean that you need to wait for complications to arise: if you suspect any inflammation of the gallbladder, you should consult a doctor as soon as possible.
Our advantages:
- Comprehensive examination before surgery as soon as possible. The average examination time is about 5 hours. The examination can be carried out both on an outpatient and inpatient basis.
- Individual approach to each patient, the ability to perform operations at any convenient time.
- The cost of examination and treatment is known in advance, according to the preliminary plan.
- The operation is performed by an experienced surgeon specializing in modern endovideosurgical technologies.
- The most modern equipment Olympus 4K, Thunderbeat, which is not available in most municipal and private medical institutions in Moscow.
- Postoperative period using the Fast-track , that is, accelerated recovery, the ability to perform the operation in a hospital for one day*.
- Individual rehabilitation programs developed individually for each patient, outpatient support and monitoring after surgery.
The material was prepared by oncologist, endoscopist, chief surgeon of the Medicine 24/7 clinic, Konstantin Yuryevich Ryabov.
* Depends on the age and concomitant pathology of the patient, discussed separately during the consultation.
What happens during surgery
There are two ways to remove the gallbladder: open and laparoscopic. Preparation for cholecystectomy in any case includes the administration of anesthesia.
- Laparoscopic method. For planned surgical intervention, when the day is chosen in advance and the patient does not have acute inflammation of the gallbladder at the time of the intervention, the laparoscopic method is most often chosen. In this case, several incisions are made (usually 3-4) in the area above the navel on the right, through which trocars are inserted: essentially, long tubes. The necessary instruments are inserted into them for sequential application of clamps, cutting off the gallbladder, stopping bleeding and suturing the wound. A video camera is also inserted into the trocars, which allows you to observe and film the entire process. After completion, several small scars remain on the skin of the abdomen. The duration of surgery in this case is on average 1 hour.
- Open method. In cases where wider access is needed, including to other organs (for example, to the liver or its ducts), as well as in complicated cholelithiasis with a risk of rupture of the bladder during removal, an incision is made in the area of the right hypochondrium or the midline of the abdomen, from the sternum to the navel. The duration of such surgical intervention can be several hours. Similar to the laparoscopic method, the surgeon ties the gallbladder, compresses the vessels and bile ducts, and cuts off the bladder. If stones are suspected of getting into the ducts or the bladder ruptures, the necessary manipulations are performed. After all problems have been eliminated, the wound is sutured and a special tube - a catheter - is usually left in place, since fluid can accumulate at the incision site. After some time, it is removed, and after the wound has healed, the sutures are removed.
Under the compulsory medical insurance policy, surgery to remove the gallbladder can be performed free of charge.
Removal methods, advantages of laparoscopic surgery
The principle of cholecystectomy is the same, only the approaches to the organ differ: laparotomy, minimal access, laparoscopy with modifications (minilaparoscopy, SILS, NOTES).
In the modern world, endoscopic interventions are replacing standard laparotomy. Moreover, possible modifications of access for the endoscope have appeared, which minimizes surgical trauma, reduces pain and speeds up rehabilitation. The single-port SILS approach is actively developing, and in women the NOTES transvaginal approach is used. Another type is minilaparoscopy, the main difference of which is the size of the ports (not 10 and 5 mm, but 5 and 3 mm).
What complications can there be?
Any surgical procedure carries the risk of potential complications. After removal of the gallbladder, you may experience:
- inflammation of the bile ducts, peritoneum (peritonitis);
- bleeding;
- also, in some cases, wound suppuration and slow healing are noted, especially in elderly, weakened people, and patients with diabetes.
But these problems arise quite rarely. In general, gallbladder removal is a surgery with a low risk of complications.
Do you need to limit yourself to food for the rest of your life?
Russian manuals for doctors tell you to eat according to “table number 5” throughout your life, while foreign ones say that in the absence of complaints, a diet is not needed. But this does not mean that you should eat exclusively burgers: we are talking about a varied diet, which includes vegetables, fruits, carbohydrates, and fats. For example, read the article about what you can eat if you have liver disease.
Here's what our expert, gastroenterologist-hepatologist Ekaterina Kashukh says about this:
Modern dietary guidelines come to the ineffectiveness of long-term diets and the concept of “correction of eating behavior.” My patients after cholecystectomy, among those who eat whatever they want within reasonable limits, and among those who sacredly honor table 5, have the same number of problems with the gastrointestinal tract. Only the first ones look happier. Expert of the site pokhover.rf Ekaterina Kashukh
Problems after gallbladder removal
Pain in the right side
In many cases, removal of the gallbladder occurs without negative consequences and the person quickly returns to normal life. But sometimes problems arise.
Most often, this is pain in the right hypochondrium, which is associated with the body’s adaptation to the fact that it no longer has a reservoir for bile. Within a few weeks after surgery, pain and discomfort in the right hypochondrium should go away. In some cases, the doctor may prescribe antispasmodics, anti-inflammatory and choleretic drugs to relieve symptoms.
Very rarely does a situation arise in which a stone has passed from the gallbladder into the ducts and gone unnoticed. In this case, along with pain in the right side, there will be an increase in body temperature, chills, nausea, and vomiting. In such cases, you need to seek medical help as soon as possible.
Abnormal stool and bloating
Bile flows from the ducts into the intestines and is involved in digestion. When its quantity decreases in the intestines, constipation occurs, and when outflow increases, diarrhea occurs. After removal of the gallbladder, diarrhea is more common, which is due to the lack of a reservoir for the accumulation of excess bile.
But sometimes bile is also released unevenly, which leads to the proliferation of bacteria in the small intestine, where there should be very few of them. This condition is called small intestinal bacterial overgrowth. In this case, the person notices bloating, increased formation of gases, and bursting pain in the abdomen from gases. To eliminate problems with stool and bloating, the doctor usually prescribes drugs to normalize the flow of bile and intestinal antibiotics.
Surgical treatment of cholelithiasis in women
In contrast to very sensitive skin, the vagina is an ideal route to access the gallbladder: it is well supplied with blood, relatively impervious to pain and very elastic. It is through the vagina that the patient can quickly and safely remove a gallbladder full of stones. In this case, the posterior vaginal fornix can be better disinfected than, for example, the navel.
Thanks to minimally invasive operations using this method, postoperative pain in patients is minimized, the risk of infection is reduced, and the recovery period after surgery is shortened. Moreover, the risk of hernias is also minimal! However, the decision to choose the optimal surgical method is made individually for each patient.
Prevention of consequences
It should be understood that any surgical intervention is traumatic for the body, and it needs time to adapt and recover. Therefore, you should follow the recommendations of doctors.
- You should not adhere to any long-term diet after removal of the gallbladder in the absence of problems with stool and abdominal pain: a varied healthy diet is necessary.
- If you have diarrhea or bloating, you should limit your intake of fatty, spicy foods, drinks containing caffeine, and the consumption of dairy products, as well as treating bile outflow dysfunction.
- It is necessary to control weight and hormonal levels in the presence of relevant diseases.
An expert on the site Pokhmelye.rf, gastroenterologist Daniela Purgina, refutes the typical misconception regarding cholecystectomy.
It is a very common belief that after removal of the gallbladder, you need to constantly take some kind of medication to drain bile. In fact, there is no need for this. Taking choleretic drugs is completely unjustified, since the bladder has been removed and there is nowhere to drive the bile from; it will go from the liver through the ducts to the intestine. Ursodeoxycholic acid drugs are prescribed only if there is a risk or stones have been identified in the bile ducts.
What is postcholecystectomy syndrome
The operation to remove the gallbladder is scientifically called cholecystectomy. Such a surgical intervention can go without problems, but it can cause some complications.
If, after cholecystectomy, problems with the outflow of bile occur, accompanied by characteristic symptoms, doctors call this postcholecystectomy syndrome (PCES). Symptoms may occur immediately after surgery or some time later.
This pathological condition is most often associated with dysfunction of the sphincter of Oddi, which plays a key role in the normal outflow of bile and pancreatic juices. The fact is that the contractility of this sphincter of the duodenum is impaired. According to studies, the disease is diagnosed in approximately 10–15% of patients after gallbladder removal. Manifestations may vary from person to person, but in any case you will need to see a doctor and begin treatment to avoid more serious complications.
What causes PCES to develop?
The development of postcholecystectomy syndrome is associated with various problems that arise in the gastrointestinal tract after removal of the gallbladder. One of the most common causes is disruption of the normal functioning of the sphincter of Oddi, which is located on the wall of the duodenum. This structural element of the digestive system is a circular muscle responsible for the supply of bile and pancreatic enzymes to the intestinal cavity. Upon a signal, the sphincter of Oddi opens, which is accompanied by the outflow of bile and pancreatic juices into the intestines, and also closes upon a signal.
Pathological changes in the sphincter of Oddi develop in most patients precisely after surgery to remove the gallbladder. As doctors explain, the mechanism of the disease works like this:
- In the absence of a bladder, signals about its filling do not arrive to the sphincter, which leads to the formation of constant tension in the orbicularis muscle and the development of congestion in the pancreatic gland and hepatic ducts.
- An uneven outflow of bile leads to a decrease in its bactericidal effect in the small intestine, and bacteria begin to multiply excessively in it. These microbes are opportunistic, that is, they should even be present in small quantities in the intestines, but when there are a lot of them, problems arise (gas formation, pain in the navel).
Among the most common causes of symptoms of PCES are also:
- the presence of residual calculi (stones) in the bile ducts after surgery;
- progressive bile duct cyst;
- biliary dyskinesia;
- stone formation as a result of obesity or diabetes.
Sometimes the cause of this pathological symptom complex may be severe postoperative pain, which is not relieved by non-narcotic analgesics, and the accumulation of effusion (fluid) in the area of the surgical intervention.
Rarely (about 5% of clinical cases) the true reasons for the development of changes in the functionality of the sphincter of Oddi remain unknown to doctors.
How does PCES manifest itself?
As already mentioned, the symptoms of postcholecystectomy syndrome can vary. Just in case, after surgery to remove the gallbladder, listen to your body - and if alarming phenomena occur, consult a doctor. Bad signs can appear either a few days or several weeks after surgery.
The most common manifestations of PCES include:
- dyspeptic symptoms, which are manifested by a feeling of bitterness in the mouth, nausea, flatulence;
- diarrhea or constipation;
- aching, cramping pain of varying intensity in the right hypochondrium, which radiates to the right shoulder and collarbone;
- bloating, excess gas formation;
- hypovitaminosis conditions associated with insufficient absorption in the intestine;
- jaundice and chills with an increase in body temperature of 38°C and above (if stones remain in the bile ducts after surgery).
The disease can take various clinical forms. Sometimes after removal of the gallbladder the following consequences occur:
- relapses of stone formation in the biliary tract;
- strictures (narrowing of the lumen) of the common bile duct;
- papillitis (inflammation of the papilla of the excretory duct in the duodenum;
- the formation of adhesions that disrupt the outflow of bile fluid in the subhepatic space;
- inflammation of the pancreas;
- ulceration of the gastroduodenal digestive tract.
Pain in this area can occur not only after surgery, but also with the entire organ. Read the article about how to identify the disease by the nature of the pain and how to treat pain in the gallbladder.
A case from the practice of gastroenterologist Daniela Purgina, an expert on the website Pokhmelye.rf.
I rather remember a whole group of cases where a patient with asymptomatic cholelithiasis had his gallbladder removed, and after the operation, postcholecystectomy syndrome developed or, even worse, hologenic diarrhea (that is, diarrhea with bile). So the tactics should be in the maximum effort to preserve the organ.
Modern diagnostics
To confirm postcholecystectomy syndrome, the patient needs a series of examinations. As a result, the doctor will be able to determine the main causes of the development of the pathological condition and the degree of functional disorders of the digestive system. Unfortunately, most patients do not immediately turn to specialists.
Diagnostics usually includes the following steps:
- Conversation with the patient, detailed discussion of complaints, study of the medical history and life of the patient, identification of the leading pathological signs from all complaints.
- Clinical examination of a person, allowing to determine the localization of the source of the disease and assess the extent of the disorders.
- A set of laboratory tests, which includes general and biochemical blood tests with assessment of the functioning of the liver and pancreas, analysis of thyroid hormones, tests for viral hepatitis.
- Ultrasound examination of the organs of the hepatobiliary zone (standardly includes the liver, gall bladder and bile ducts. Since the gall bladder has already been removed, only the ducts and liver are examined).
- Esophagogastroduodenoscopy.
- If necessary, endoscopic examination of the bile ducts (endosonography, endoscopic retrograde cholangiopancreatography), manometry of the sphincter of Oddi, MRI and abdominal organs is also performed.
A complete and detailed diagnosis of suspected PCES allows the doctor to draw conclusions about why the disorders began, how far they have gone, whether there are any serious complications, and what therapy is suitable for treatment. Read on to learn how to treat post-operative problems.
How to be treated
The main thing in the treatment of PCES is to eliminate the factors that triggered the development of symptoms. The main principles of such therapy are:
- eliminating the influence of factors contributing to the occurrence of pathological manifestations;
- symptomatic treatment of dysfunctions of the organs of the hepatobiliary region;
- prevention of possible complications.
As a rule, in addition to drug intervention, doctors recommend in the first stages an increase in the frequency of food intake to 5–7 times a day to normalize the outflow of bile. Any strict diet is usually not required; this is discussed individually.
In order to eliminate the symptoms of the disease, the patient may be prescribed:
- analgesics and antispasmodics, since inflammation is accompanied by pain and spasm of the sphincter of Oddi;
- proton pump inhibitors to reduce acidity in the upper gastrointestinal tract if there is inflammation there;
- drugs to normalize the flow of bile;
- antacids to combat high acidity;
- non-absorbable antibiotics to eliminate bacterial overgrowth in the small intestine.
Sometimes medications cannot correct the problem, in which case surgery is indicated. Surgical treatment methods are aimed at restoring the patency of the bile ducts and normalizing the functioning of the sphincter of Oddi.
How to avoid complications after gallbladder removal
Doctors are well aware that postcholecystectomy syndrome is a common occurrence. However, today there are no special measures to prevent it. When you have your gallbladder removed, you must remember that PHES may not catch up with you months later.
In order to reduce the risk of its occurrence, you should follow the principles of a healthy lifestyle: a balanced diet, giving up bad habits, adequate sleep and moderate physical activity. People with high cholesterol levels and endocrine system disorders should be regularly examined by doctors.
The prognosis for cure for PCES directly depends on how effectively the problem that caused its development was dealt with.