The human pancreas is an organ capable of performing two completely different functions. Despite its small size, the pancreas is of great importance for the body. What happens when its function is disrupted, and what diseases of the pancreas and treatment exist?
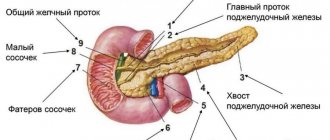
Organ structure
Anatomically, the organ consists of three main sections: head, body and tail. Despite the structural features, each department performs the same functions. First of all, this is the production of enzymes that are necessary for digestion, as well as hormones, such as insulin and glucagon, that control blood glucose levels. Enzymes produced by the gland enter the intestine through its ducts, which open into the lumen of the duodenum. The structure of the organ is divided into two parts, depending on its functional purpose. Thus, the exocrine (exogenous) part of the gland is more developed and occupies about 70-75% of the organ’s mass. In its structure, one can distinguish alveoli, represented by secretory cells that produce secretions, and excretory ducts. The intrasecretory (endogenous) part is the islets (cells) of Langerhans, where the secretion of various hormones occurs:
- A-cells - their main purpose is to produce glucagon;
- B or beta cells produce insulin;
- D cells produce another hormone – samostatin.
In the intrasecretory part of the gland there are more beta cells.
Exocrine function of the pancreas
The secretory function of the pancreas is divided into two types:
- • Ecbolic function - consists in the synthesis of more than twenty enzymes and proenzymes by its cells and their release into the duodenum. Digestive enzymes make up more than 90% of the proteins in pancreatic juice and are involved in the breakdown of food in the intestines.
- • Hydrokinetic function - consists of producing water, bicarbonates and other electrolytes. This function affects the neutralization of stomach contents, creating an alkaline environment in the intestines, favorable for the activity of pancreatic and intestinal enzymes.
Enzymatic function
It comes down to the formation and release of digestive juices, which are 90% water and 10% sediment. This sediment is represented by protein substances and mineral compounds. The juice that the organ secretes contains various enzymes: trypsin, chemotrypsin, amylase, alkaline phosphatase and many others. Each of these enzymes is involved in the digestion of a specific type of food. For example, trypsin breaks down proteins into their constituent amino acids. It is released as inactive trypsinogen, but is activated by enzymes in the intestine. When the pancreas malfunctions, for example, in inflammatory or autoimmune diseases, trypsin and other enzymes are activated in the gland itself, which provokes its destruction; it literally digests itself. A number of electrolytes, such as sodium, potassium, chlorine, calcium, zinc, copper and bicarbonates, neutralize the acidic contents of the duodenum, while simultaneously creating optimal conditions for the activation of enzymes, and complete digestion becomes possible.
Hormonal function
The gland produces a number of important hormones: insulin, glucagon and somatostatin. Insulin is produced by beta cells from its precursor, proinsulin. Glucose stimulates its production. As soon as its level in the blood increases, its production is stimulated. Insulin in the blood is in a free or bound state, and its breakdown occurs in the liver and kidneys under the influence of insulinase and proteolytic enzymes. Insulin controls the transport of glucose into cells and insulin-sensitive tissues, stimulates the breakdown of glycogen (a polysaccharide formed by glucose residues), which reduces blood sugar levels. Glucagon is a polypeptide; its secretion also occurs under the influence of glucose, some amino acids, and the sympathetic nervous system. As soon as the level of glucose in the blood decreases, the production of glucagon is triggered, because under its action gluconeogenesis is stimulated - a metabolic process leading to the formation of glucose from non-carbohydrate compounds. During this process, glucose and ketone bodies are formed.
The role of the pancreas in digestion
_Title The role of the pancreas in digestion _Author _Keywords
The pancreas (P) plays an important role in the digestive process. The exocrine function of the pancreas is to secrete pancreatic juice, which is crucial in intestinal digestion. The exocrine function of the pancreas is divided into ecbolic, which provides the release of enzymes, and hydrokinetic, which consists of the secretion of water and bicarbonates. From 1000 to 3000 ml of pancreatic juice is released per day, which has a complex composition: 98% of it consists of water, the rest is enzymes, inorganic substances and electrolytes. Its relative density ranges from 1.007 to 1.042, pH 7.5 – 8.8. The alkaline reaction of the juice is due to the presence of bicarbonates. In addition, the juice contains small amounts of magnesium, copper, and zinc; of the anions - bicarbonate ion, which neutralizes hydrochloric acid coming from the stomach. Pancreatic juice contains 2 groups of enzymes: those produced in active form (amylase, lipase, nuclease) and proenzymes, or zymogens, produced in an inactive state and activated in the duodenum under the influence of other enzymes (trypsinogen, chymopepsinogen, proelastase, procarboxypeptidase).
All produced enzymes ensure the hydrolysis of proteins, fats and carbohydrates. Thus, proteases (trypsin, chymotrypsin, elastase, etc.) hydrolyze proteins to low molecular weight peptides and amino acids; amylase promotes the breakdown of carbohydrates into di- and monosaccharides (glucose, fructose, galactose), and lipase hydrolyzes fats into monoglycerides and fatty acids (and this process occurs in the presence of bile, calcium and magnesium ions at pH 8.8 - 9.0). Nervous and humoral mechanisms take part in the regulation of the exocrine pancreas.
Parasympathetic nerves (nuclei of the vagus nerve are located in the medulla oblongata) have a stimulating effect on the exocrine activity of the pancreas. Activation of the vagus nerve is achieved by the initiation of conditioned and unconditioned reflexes (sight, smell, taste of food; stretching of the body and antrum of the stomach), as well as hematogenously during hypoglycemia, increasing the concentration in the blood of gastrin, cholecystokinin-pancreozymin, fatty acids, tryptophan, amino acids and peptides. In addition, stimulation of the secretory activity of the pancreas is carried out through local (humoral) mechanisms. Thus, the entry of food chyme containing acid and fats into the duodenum causes the cells of the small intestine to secrete secretin, which, in turn, stimulates the secretion of pancreatic juice, rich in bicarbonates, but practically free of enzymes and proenzymes. On the contrary, cholecystokinin-pancreozymin formed by the cells of the small intestine and other stimulants hematogenously promote the formation and secretion of juice rich in enzymes and proenzymes by the pancreas. When the sympathetic nervous system is irritated (pain, mental and physical stress), suppression of pancreatic secretion is observed.
The endocrine function of the pancreas is the secretion of glucagon, insulin, somatostatin and pancreatic polypeptide, respectively, by A, B, D and PP cells. Pancreatic hormones, in addition to controlling anabolic processes as such, directly affect digestion through their effectors. Glucagon regulates the metabolism of liver glycogen, which is important in the homeokinesis of blood sugar, excretory and endocrine functions of the pancreas. Insulin is an anabolic hormone and regulates the processes of glyco- and lipogenesis. Somatostatin controls the secretion of glucagon and insulin, and also affects the motility of the digestive tract.
Disorders of the pancreas
Disorders of the digestive process in the small intestine are directly related to changes in enzyme synthesis caused by pancreatic dysfunction. In the presence of pathological processes in it, the action of lipase, which hydrolyzes fats, is inhibited, which leads to their insufficient digestion and excretion with feces up to 80% of the mass entering the body. The breakdown of proteins is also impaired, as may be evidenced by creatorrhea, a characteristic feature of which is the presence of an increased volume of muscle fibers in the stool. Digestive insufficiency can lead to such negative consequences as dyspeptic syndrome, dehydration, acid-base imbalance and intestinal autointoxication. External secretion of the pancreas is caused by the presence in the body of a number of inflammatory diseases and some other pathological processes:
- pancreatitis in acute and chronic stages;
- cholelithiasis;
- the presence of parasites in the intestines;
- duodenitis, duodenal ulcer, which results in a decrease in the production of pancreatic juice;
- tumors;
- vaterites;
- excess body weight, hormonal imbalance, resulting from metabolic disorders, causing dystrophic lesions of the pancreas;
- allergic restructuring of the body;
- Vagal dystrophy, long-term atropinization;
- tumors that destroy the pancreas.
The development of obstructive processes in the pancreas that impede or completely block the outflow of pancreatic juice into the duodenum, and the resulting hypertension that results from this pathology can cause acute pain in this area, as well as internal ruptures and destruction of the parenchyma of the organ. As a result of the destruction of the pancreas, its enzymes and destruction products are absorbed into the blood and surrounding organs, which leads to the development of necrosis and the formation of a body intoxication syndrome.
Why does the pancreas produce less enzymes than needed?
There are many reasons why the pancreas stops producing the required amount of enzymes. But basically it comes down to three risk factors:
- Alcohol
The liver and pancreas are a little similar: both organs cannot tolerate alcohol. This is their Achilles heel. Alcohol damages pancreatic cells and leads to the development of inflammation. Therefore, alcohol lovers sooner or later develop pancreatitis. Often - in combination with cholelithiasis and alcoholic hepatitis. Naturally, an inflamed pancreas cannot produce the required volume of enzymes.
— At holidays and parties they remember that it’s a good idea to go out into the air and deal a nicotine blow to the pancreas. It stimulates the reaction of blood vessels and, together with the toxic effect of alcohol, destroys gland cells, writes Sergei Vyalov.
- Fatty food
The pancreas is very sensitive to the levels of cholesterol and triglycerides in the blood. Therefore, large amounts of fatty foods often lead to disruption of gland function and the appearance of symptoms. Most likely, at the initial stage of the disease you will feel pain in your back or lower back. When the pathological process is advanced, the pain becomes girdling.
If the pancreas receives a triple blow - alcohol, tobacco, fatty foods - an attack of acute pancreatitis occurs. This is exactly what happens on New Year's Eve, when ambulances en masse transport patients with inflammation of the pancreas to hospitals.
- Sweets
The pancreas produces the hormone insulin, which is responsible for regulating blood glucose levels. A large amount of sugar in the diet is a high load on the pancreas, because it has to produce more insulin to utilize glucose. Over time, the beta cells that produce insulin become depleted, blood sugar levels become persistently high, and type 2 diabetes develops.
Pancreatic enzymes
There are several types of pancreatic enzymes:
- • Amylolytic enzymes (amylases) break down complex carbohydrates into dextrins, maltose, maltooligosaccharides and glucose.
- • Lipolytic enzymes (lipases) break down fats into fatty acids and monoglycerides that pass through the enterocyte membrane.
- • Proteolytic enzymes (proteases) break down proteins by breaking internal bonds in the middle of amino acid chains and synthesizing peptides.
- • Nucleolytic enzymes (nucleases) break down nucleic acids. Phosphodiesterases present in pancreatic juice are divided into two groups: ribonuclease breaks down ribonucleic acid, and deoxyribonuclease hydrolyzes deoxyribonucleic acid.