If stones are detected in the common bile duct, then this form of gallstone disease is called choledocholithiasis.
.
Historical information
The disease has been known since ancient times. Gallbladder stones were first discovered during autopsies of corpses and described by Galen, a great surgeon, writer and philosopher who lived in the second half of the 2nd century AD in ancient Rome. During the Renaissance, in the writings of Gentile de Foligno in 1341, there is also a mention of cholelithiasis.
A detailed description of gallstones appeared in the middle of the 18th century (C. Galeati), and at the same time the study of their chemical composition was undertaken for the first time. All information about cholelithiasis contained in the works of various authors was summarized by Albrecht Haller (1755). In his works, he showed that gallstones are found not only in humans, but also in horses, pigs, cows, marmots, monkeys and other animals.
What's happening?
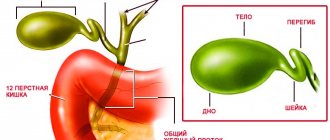
The formation of gallstones occurs as a result of the precipitation of dense particles of bile. Most stones are made up of cholesterol, bilirubin (bile pigment) and calcium salts. They interfere with the normal functioning of the gallbladder, which serves as a reservoir of bile.
Sometimes, due to bumpy driving, overeating, or other provoking factors, a stone can come out at the mouth of the bile duct (biliary colic) and block it. As a result, the outflow of bile from the bladder is disrupted, its walls become overstretched and the person feels severe pain. This can lead to inflammation of the gallbladder - acute cholecystitis. Inflammation can also spread to nearby organs - the pancreas, duodenum, stomach.
Gallstone disease (GSD)
Gallstones are a common disease that develops in people over the age of 40. This disease is especially common among the urban population of industrialized countries. According to most researchers, about 10% of men and up to 25% of women in European countries suffer from cholelithiasis.
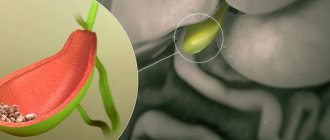
With cholelithiasis, calculi (stones) form in the gallbladder and bile ducts. These stones consist of the usual components of bile - bilirubin, cholesterol, calcium salts. Most often, mixed stones are found, containing in greater or lesser proportions the indicated components. If a stone consists of 90% cholesterol, then such a stone is called “cholesterol”, if it is made of bilirubin - “pigment”, and if it is made of calcium salts - “lime”. The size and shape of stones in gallstone disease can vary. Dimensions generally vary from 1–2 mm to 3–5 cm; the shape can be round, oval, polyhedron, etc.
Causes of gallstone disease
The main site of gallstone formation is the gallbladder, and in very rare cases, the bile ducts. Currently, in clinical medicine there are three main reasons for their formation: stagnation of bile in the bladder, metabolic disorders, inflammatory changes in the wall of the gallbladder . Metabolic disorders cause a change in the ratio of the concentrations of cholesterol, phospholipids (lecithin) and bile acids in bile. The concentration of cholesterol increases and phospholipids decreases. Such bile is considered to be lithogenic. Under such conditions, bile cholesterol easily falls out in the form of crystals; these crystals are grouped and combined with each other, which leads to the formation of stones. It is known that gallstone disease often develops in patients with metabolic diseases such as diabetes, obesity, and hemolytic anemia. When bile stagnates for a long time in the bladder, it becomes infected. The infection leads to damage to the wall of the gallbladder and desquamation of its epithelium. All this contributes to faster deposition of cholesterol crystals and the formation of gallstones. In the damaged wall of the gallbladder, the absorption process of some bile components is disrupted, their physicochemical ratio changes, which also contributes to stone formation. In addition, with cholestasis in the bile located in the gallbladder, the concentration of cholesterol, bilirubin, and calcium may increase, which increases the lithogenicity of the bile. This is facilitated by eating foods rich in cholesterol, obesity, and taking oral contraceptives.
Clinical manifestations of cholelithiasis
Gallstone disease can be asymptomatic (the so-called latent form of cholelithiasis). In this case, gallstones are discovered as an incidental finding when examining patients for another disease.
Patients with gallstones may be bothered by dyspeptic disorders : an unpleasant metallic taste, bitterness in the mouth, nausea, bloating, a feeling of heaviness in the right hypochondrium, especially after eating fatty foods. Such phenomena are caused by impaired motility of the biliary tract and gastrointestinal tract with the reflux of bile into the stomach and esophagus. This form of cholelithiasis is called dyspeptic.
The classic clinical manifestation of cholelithiasis is hepatic (biliary) colic, which is characterized by intense cutting, stabbing, tearing, and less often paroxysmal pain in the right hypochondrium and epigastric region. These pains often radiate to the lumbar region, right shoulder blade, and right forearm. The pain can also spread to the heart area and be mistakenly perceived as an angina attack. Pain occurs most often after an error in diet (eating fatty, spicy foods), during physical activity, psycho-emotional stress, or bumpy driving. The occurrence of pain is associated with the movement of stones in the biliary tract and their infringement in the neck of the gallbladder or cystic duct, increased pressure in the gallbladder or ducts as a result of impaired outflow of bile. Often an attack of hepatic colic is accompanied by nausea and repeated vomiting mixed with bile, which does not bring relief to the patient. Colic can last from a few minutes to several hours. Patients are restless and often change position, trying to find a comfortable position that reduces the intensity of pain. This form of cholelithiasis is called painful paroxysmal.
Diagnosis of cholelithiasis
The diagnosis of cholelithiasis is made on the basis of: patient complaints, medical history, physical examination by a doctor and mainly according to instrumental examination data. At the same time, to make a diagnosis, it is often enough to conduct only one ultrasound examination of the abdominal organs, in which stones are detected in the lumen of the gallbladder or in the ducts. The patient examination can also be supplemented with X-ray examination. In this case, radiocontrast techniques are used, such as oral cholecystography or intravenous cholecystocholangiography. With the first method, the patient takes a special radiocontrast drug inside, several hours before taking an x-ray, which is captured by the liver cells and released into the bile. During cholecystocholangiography, a radiopaque contrast agent is administered intravenously; it is also captured by liver cells and released into the bile. After contrast, an x-ray is taken and if a defect in the filling of the lumen of the gallbladder or ducts is detected, this may indirectly indicate the presence of stones (stones) in them, although the same x-ray picture can be given by both polyps and a cancerous tumor of the gallbladder. Currently, the X-ray method for diagnosing cholelithiasis is practically not used due to its low information content, low cost-effectiveness, and lack of ease of use.
Treatment of cholelithiasis
Currently, surgical treatment is the only possible way to radically get rid of cholelithiasis.
There are still no effective drugs that can cause the dissolution of stones in the gallbladder and bile ducts. Some drugs can dissolve only certain types of stones, but with long-term use they cause serious side effects and complications.
There is an alternative, less traumatic surgical method for treating gallstone disease, such as extracorporeal shock wave lithotripsy. The essence of the method is the destruction of gallstones by a shock wave generated by a special device. The shock wave is strictly focused on the gallbladder, under its influence the stones are crushed into small fragments and sand, which in some cases, along with bile, are released into the duodenum. Despite the simplicity of this treatment method and its low invasiveness, the effectiveness of treatment remains very low even today. This is due to the fact that not all stones can be crushed. In 10–30% of cases, fragments of destroyed stones are large and cannot exit through the natural opening of the common bile duct. In this case, they can become pinched in the neck of the gallbladder and lead to a severe attack of hepatic colic, or get stuck in the common bile duct and disrupt the flow of bile into the duodenum, which will lead to the development of obstructive jaundice. Both of these conditions require immediate hospitalization in a surgical hospital! The shock wave not only destroys stones, but in some cases causes serious damage to the liver and gallbladder walls. The use of extracorporeal lithotripsy in patients with gallstone disease should be carried out according to certain indications: single cholesterol (X-ray negative) stones with a diameter of no more than 3 cm, occupying no more than half of a well-functioning gallbladder. This bloodless method is especially indicated in the treatment of elderly and senile patients. Contraindications for lithotripsy are: x-ray positive stones (with the inclusion of calcium salts), stone diameter more than 3 cm, multiple stones occupying more than half of the gallbladder, disabled gallbladder, history of frequent renal colic, inflammatory diseases of the hepatoduodenal zone.
To date, many methods of surgical treatment of cholelithiasis have been developed. With any type of surgical treatment, stones are completely removed along with the gallbladder - the main pathogenetic substrate of the disease! This completely eliminates the return of the disease.
The absolute indications for surgical treatment of gallstone disease are:
- history of severe attacks of hepatic colic;
- the presence of large stones that can cause a pressure sore of the bladder wall;
- the risk of developing gallbladder cancer, which occurs in 5% of patients suffering from gallstone disease for a long time;
- small bladder stones that can block the cystic duct, penetrate the common bile duct and cause obstructive jaundice, cholangitis, biliary acute or chronic pancreatitis.
A relative indication for surgical treatment is the presence of latent and dyspeptic forms of cholelithiasis.
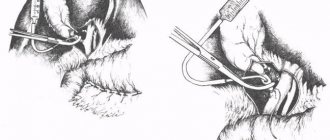
The main type of surgery for gallstone disease is traditional (open) cholecystectomy (removal of the gallbladder). In this case, various types of accesses (incisions) are performed through the anterior abdominal wall and penetrate into the abdominal cavity. After intraoperative inspection of the gallbladder, extrahepatic bile ducts, duodenum and pancreas, and assessment of the nature of pathological changes, its complete removal is performed. The classical approach provides wide access to the hepatobiliary zone and a good overview of all interested organs, however, it is associated with significant tissue trauma (especially the anterior abdominal wall), which leads to a rather long period of postoperative rehabilitation and a higher risk of complications in the operating room compared to minimally invasive techniques wounds.
Currently, the most popular are minimally invasive surgical interventions in the treatment of cholelithiasis, such as mini-access cholecystectomy and laparoscopic cholecystectomy.
Advantages of laparoscopic surgery
Pain in the postoperative period is minor and, as a rule, is observed only on the first day.
Immediately after recovery from anesthesia (several hours after the operation), the patient can walk and care for himself.
The length of hospital stay is much reduced (up to 1–4 days), as is the time required to restore working capacity.
The number of postoperative hernias is reduced several times.
Laparoscopic surgery is a cosmetic operation; after a few months, scars after punctures become almost invisible in most patients.
Cholecystitis - inflammation of the gallbladder
Often develops with cholelithiasis (so-called stone cholecystitis, up to 80–90% of the total number of diseases [1]), after viral hepatitis and other infectious diseases, in the presence of chronic focal infection (for example, tonsillitis) or parasitic diseases (for example, opisthorchiasis). The development of cholecystitis is facilitated by stagnation and changes in the composition of bile, which may be associated with dietary habits. Often cholecystitis is combined with cholangitis.
There are calculous (presence of gallstones in the bladder) and acalculous, acute and chronic cholecystitis.
Diagnosis of cholecystitis
- Ultrasound of the abdominal organs with examination of the gallbladder, bile ducts, and pancreas.
- General and biochemical blood test.
- X-ray examination (if obstructive jaundice develops and the presence of stones in the bile ducts is suspected).
Acute cholecystitis
The main signs of acute cholecystitis: paroxysmal pain in the right half of the abdomen, radiating to the right shoulder and shoulder blade; nausea and vomiting; chills and increased body temperature; Jaundice and itching of the skin are possible. A dangerous complication of acute cholecystitis is peritonitis. Cholecystostomy (Greek chole bile + kystis bladder + stoma opening, passage) is indicated - external drainage of the gallbladder when other interventions are impossible.
The presence of stones in the gall bladder is an indication for surgery.
This is due to the fact that the presence of stones in the gallbladder can at any time lead to acute cholecystitis, its necrosis with the development of complications:
- empyema of the gallbladder - infection of the contents of the gallbladder;
- hydrocele of the gallbladder - a violation of the outflow of bile, but without its infection, while the elements of bile are absorbed, and the bladder remains filled with transparent contents;
- phlegmon of the gallbladder - purulent inflammation of the wall of the gallbladder;
- subhepatic abscess;
- biliary fistulas;
- peritonitis, sepsis are deadly complications that can develop with the progression of the complications described above.
If complications develop, the operation is performed on an emergency basis and is associated with a high risk of complications, and the rehabilitation period ranges from several weeks to several months!!!
Chronic cholecystitis
Chronic cholecystitis can be acalculous and calculous, from the Latin word “calculus”, which means “stone”. Calculous cholecystitis is one of the results of cholelithiasis. Chronic cholecystitis is manifested by nausea, dull pain in the right hypochondrium and other unpleasant sensations that occur after eating. In recognizing cholecystitis, laboratory data and cholecystocholangiography play an important role.
The most serious complication of calculous cholecystitis is hepatic colic. If a small stone (less than 1 cm) does not pass through the bile ducts, blocking the flow of bile, then bile pigments enter the blood and subhepatic jaundice develops.
The symptoms of colic are very similar to the onset of acute cholecystitis. However, colic hurts much more severely and usually begins at night or early in the morning.
After some time, the symptoms of jaundice appear: yellowing of the sclera and skin occurs - a peculiar lemon-yellow color appears, urine darkens and becomes like beer, and feces noticeably lighten, even white.
Patients in this condition are subject to emergency hospitalization.
Chronic cholecystitis can be a consequence of acute cholecystitis, but it can also occur independently. In Russian medical literature, it is customary to distinguish typical and atypical types of symptoms of gallbladder diseases (cholelithiasis-K 80.2 and chronic cholecystitis).
The presence of stones in the gall bladder significantly complicates the task of treatment and worsens the prognosis of the disease.
Share this page:
How does it manifest?
While the stones are not in the duct, but lie quietly in the gallbladder, a person may not even be aware of his illness. The first warning signs that indicate cholelithiasis are: heaviness in the right hypochondrium, bitterness in the mouth, nausea and belching.
Sometimes the stone passes out of the gallbladder into the bile ducts. In this case, an attack of so-called biliary colic : a sharp pain occurs in the right hypochondrium or in the upper abdomen. It can “give” to the right collarbone, right arm or back. In this case, bitterness appears in the mouth, nausea and vomiting, which does not bring relief.
If the stone (with a relatively small size) was able to bypass the ducts and fall into the duodenum, the attack stops on its own, and the stone is passed out with feces. Otherwise, blockage of the bile ducts occurs and there is a danger of developing acute cholecystitis and mechanical (subhepatic) jaundice.
The most important thing for the patient
In the modern world, cholelithiasis is a well-studied pathology, and laparoscopic surgery is the “gold standard of treatment.”
Unfortunately, many people do not pay attention to the initial manifestations of the disease and do not undergo medical examination or preventive examination to detect stones in the gallbladder. As a result, the disease is detected at late stages, when drug treatment is not only ineffective, but also contraindicated, and the success of minimally invasive surgery also becomes questionable. If you have the complaints described above, as well as the risk factors listed above, you must contact a surgeon or gastroenterologist to receive recommendations for examination and selection of optimal treatment or preventive measures.
Our Clinic performs a full range of diagnostics, surgical and endoscopic treatment of cholelithiasis and its complications. Surgical operations in most cases are performed minimally invasively using laparoscopic and endoscopic technologies.
Diagnostics
Diagnosis and treatment of uncomplicated cholelithiasis (GSD) is carried out by a gastroenterologist. The diagnosis can be made based on the patient's complaints and a number of additional studies.
First of all, the patient will undergo an ultrasound of the abdominal organs. In more complex cases, an X-ray examination may be required with preliminary administration of a contrast agent (orally or intravenously) - cholecystocholangiography. Contrast material may also be injected directly into the bile ducts with a special thin needle (percutaneous transhepatic cholangiography) or through an endoscope (endoscopic retrograde cholangiopancreatography or ERCP). During ERCP it is possible to remove small stones from the bile ducts.
Cost in a paid clinic
| Service name | Price, rub |
| allergology | From 440 rub. |
| tests | From 153 RUR |
| andrology | from 15,180 rub. |
| anesthesia | from 690 rub. |
| ANESTHESIA IN DENTISTRY | from 3,150 rub. |
| VACCINATION | from 450 rub. |
| HOME CALL | from 3460 rub. |
| GASTROENTEROLOGY | from 605 rub. |
| GYNECOLOGY | from 2250 rub. |
| DERMATOVENEROLOGY | from 200 rub. |
| CHILDREN'S DENTISTRY | from 75 rub. |
| CHILDREN'S TRAUMATOLOGY | from 4890 rub. |
| CHILDREN'S MASSAGE | from 550 rub. |
| REMOTE AND CONTACT LITHOTRIPSY | from 37,950 rub. |
| IMMUNOLOGY | from 440 rub. |
| CT SCAN | from 650 rub. |
| COSMETOLOGY | from 60 rub. |
| LAPAROSCOPY | from 27,500 rub. |
| TREATMENT WITH LEECHES (HIRUDOTHERAPY) | from 220 rub. |
| MAMMALOGY | from 1,820 rub. |
| MANUAL THERAPY | from 2,250 rub. |
| MASSAGE ROOMS | from 550 rub. |
| NEUROLOGY | from 424 rub. |
| OZONE THERAPY | from 610 rub. |
| ONCOLOGY | from 2,250 rub. |
| EMERGENCY GYNECOLOGY | from 600 rub. |
| ORTHOPEDICS | from 310 rub. |
| OTOLARYNGOLOGY | from 250 rub. |
| OPHTHALMOLOGY | from 100 rub. |
| PEDIATRICS | from 1,150 rub. |
| PROCTOLOGY | from 12,100 rub. |
| X-RAY | from 1,200 rub. |
| CERTIFICATES FOR A CHILD | from 1,000 rub. |
| HOSPITAL | from 770 rub. |
| DENTISTRY | from 1,060 rub. |
| THERAPY | from 2,390 rub. |
| TRAUMATOLOGY | from 1,573 rub. |
| SHOCK WAVE THERAPY | from 1,595 rub. |
| Ultrasound | from 1,350 rub. |
| UROLOGY | from 2,750 rub. |
| PHLEBOLOGY | from 4,240 rub. |
| FUNCTIONAL DIAGNOSTICS | from 3,650 rub. |
| SURGERY | from 2,250 rub. |
| EXPRESS DIAGNOSTICS | from 198 rub. |
| ENDOCRINOLOGY | from 2,250 rub. |
| ENDOSCOPY | from 4,290 rub. |
see all prices
Treatment
Gallstone disease can be treated therapeutically (without surgery) and surgically. As a rule, treatment begins with therapeutic methods.
- Diet. It is recommended to eat 4-6 meals a day, excluding fatty, fried, spicy, chocolate, and carbonated drinks. Smoked meats, fatty meats (lamb, pork), irritating seasonings, and alcoholic drinks are prohibited. Plant foods and dairy products are recommended. It is useful to add wheat bran to food.
- Dissolution of gallstones using special preparations (ursodeoxycholic and chenodeoxycholic acids). The method is used only in the case of single small (up to 2 cm) cholesterol (X-ray negative) stones, in the absence of contraindications. The course of treatment lasts 1-1.5 years. After a few years, more than half of patients develop stones again.
- Extracorporeal shock wave lithotripsy is the destruction of stones by a shock wave created by special devices. Indicated in the case of cholesterol stones with a diameter of up to 3 cm, no more than 3 in number, with sufficient contractility of the gallbladder. The stones are crushed into small pieces (up to 1-2 mm in size) and pass out of the body in the feces on their own. The procedure is painless, well tolerated and can be performed on an outpatient basis.
Surgical treatment is prescribed in most cases. It consists of removing the gallbladder, which can be done in two ways:
- Classic cholecystectomy: during the operation, a fairly wide incision is made in the abdomen. After the operation, a 10-12 cm long suture remains.
- Laparoscopic cholecystectomy: performed using special instruments that are inserted into the abdominal cavity through small holes (up to one centimeter). After the operation, there are practically no traces left on the skin. This method has advantages compared to classical cholecystectomy: it is less traumatic, requires a shorter (up to 4-5 days) period of hospitalization, after which there is a faster recovery and return to the usual rhythm of life.
The surgeon chooses the type of operation depending on the severity of the patient’s condition, the presence of concomitant diseases and other criteria.
Consequences of chronic cholecystitis
People who suffer from chronic cholecystitis for a long time end up risking their health and even their lives. The inflammatory process from the gallbladder spreads to neighboring organs, primarily the pancreas and liver. Almost all such patients have a chronic form of pancreatitis and changes in the liver. In this case, irreversible changes occur in the gallbladder, which leads to three options for the development of the disease.
- 1. The process of formation of gallstones does not stop. The addition of infection and inflammation creates favorable conditions for the growth and formation of new stones. The bladder fills with stones and ceases to be a reservoir for the accumulation of bile. It cannot perform its basic functions in the digestive process. Food is poorly digested.
- 2. Frequent inflammation of the gallbladder due to attacks of hepatic colic lead to changes in the wall of the gallbladder: it becomes overgrown with adhesions, and the muscles are replaced with dense scar tissue. The cavity of the bladder sharply decreases in size, a “scar-wrinkled bladder” is formed, which also does not participate in the digestion process.
- 3. When the cystic duct is blocked by a stone, the bladder becomes large and overstretched. Overflowing with bile, which does not find an outlet, the bladder loses its ability to contract, and even after the stone leaves the duct it remains stretched, while it is no longer able to push out the bile. Gradually the contents become colorless - “white bile”. Hydrocele of the gallbladder develops. Sometimes it is asymptomatic (apparently, the patient simply forgets about the attack). However, if dropsy appears after an attack of hepatic colic, the enlarged gallbladder remains painful for quite a long time. Such a gallbladder also turns out to be excluded from the digestion process. In addition, bile, which remains in the gallbladder and is not renewed, easily suppurates when an infection occurs, and empyema of the gallbladder develops.
It is necessary to carry out a differential diagnosis of biliary (hepatic) colic from an attack of acute calculous cholecystitis. This is an inflammation of the gallbladder, provoked by the presence of stones in it, which is manifested not only by severe pain, but also by the presence of fever, signs of intoxication, sometimes positive peritoneal symptoms and requires emergency hospital treatment. The appearance of fever, jaundice, and decreased blood pressure in a patient with cholelithiasis requires the exclusion of such possible complications as acute cholecystitis, pancreatitis, cholangitis, etc.
Basic methods for diagnosing gallstones
Laboratory research
- With an exacerbation of cholelithiasis, changes in the clinical blood test are observed: the number of leukocytes increases with the appearance of their young forms, the ESR increases, which indicates the presence of an inflammatory process. Changes in biochemical blood parameters may occur: increased levels of liver transaminases, amylase, lipase, total bilirubin. In most cases of asymptomatic stone-carrying, the blood test may not be changed. Also, short-term attacks of biliary colic may occur without changes in laboratory parameters.
Instrumental diagnostics
- 1. The most accessible and effective method of screening diagnosis of all stages of cholelithiasis is ultrasound examination of the abdominal organs (ultrasound).
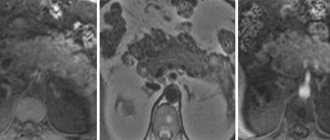
Ultrasound of the liver and gallbladder allows you to see stones in the cavity of the bladder, determine their size and mobility, assess the size of the residual cavity of the gallbladder, and identify signs of inflammation or deformation of its wall. Also, with ultrasound, the intra- and extrahepatic bile ducts are clearly visible; their deformation, expansion and the presence of additional inclusions (calculi) can be assessed. - 2. A more accurate diagnosis of the condition of the biliary tract is shown by magnetic resonance imaging - MR cholangiography.
When performing MR cholangiography, images of the gallbladder, cystic duct, segmental, lobar ducts, common hepatic duct, common bile duct and main pancreatic duct are obtained. It is possible to assess their deformation and identify the expansion or narrowing of their lumen in certain areas. It becomes possible to accurately visualize stones not only in the gallbladder, but also in the lumen of the bile ducts. Additional examination methods for cholelithiasis include computed tomography (CT) and video duodenoscopy. - 3. Computed tomography (CT)
of the abdominal cavity is performed if pathology of neighboring organs (liver, pancreas) is suspected, or if there is a suspicion of oncological pathology in the biliary system. - 4. Videogastroduodenoscopy
is an endoscopic study that resembles videogastroscopy, but is performed using a special endoscope with lateral optics, which allows you to clearly view the area of the large duodenal papilla or “papilla of Vater” (the place where the bile ducts flow into the duodenum).
Treatment of cholelithiasis and chronic calculous cholecystitis
Conservative treatment of gallstones
Doctors have ursodeoxycholic acid preparations in their arsenal, which changes the chemical composition of bile. These are the drugs henofalk and ursofalk, they are prescribed for the purpose of drug lithosis (dissolution of stones). Treatment should be carried out against the background of strict adherence to diet and nutrition, as well as anti-inflammatory therapy. The duration of treatment is up to 2.5-3 years and does not always achieve the desired result. It should be remembered that true “stones”, consisting mainly of calcium, do not dissolve. Therefore, drug treatment can only be used in the initial stages of the disease, when the sediment in the bile is mainly represented by cholesterol stones.
Surgery to remove gallbladder with stones
Cholecystectomy
– removal of the gallbladder is the main method of surgical treatment. The operation is performed either openly through an incision in the abdominal wall, or laparoscopically - endovideosurgical cholecystectomy. The purpose of the operation: removal of the gallbladder with stones. The only difference is in what instruments the surgeon uses and in what way the gallbladder with stones is removed.
In open surgery, the incision through which the bladder is removed can be made from the xiphoid process to the navel, or the second access is in the right hypochondrium. The laparoscopic method is less traumatic - special instruments and optics are inserted through 4 small incisions on the skin. With the help of these instruments, the gallbladder is removed. After such an operation, the scars are hardly noticeable. The duration of stay in a hospital bed is 2-3 days. A week later the patient is healthy.
Sources
- Nambapana MN., Wickramasuriya SS., Macelline SP., Samarasinghe K., Vidanarachchi JK. Algae-based antioxidant containing selenium yeast (Economase®) enhanced the growth performance, oxidative stability, and meat quality of broiler chickens. // Anim Biosci - 2021 - Vol - NNULL - p.; PMID:33902180
- Wu H., Sun H., Ma C., Lian L., Lu L., Xu L., Xu L. Effects of maternal dietary energy restriction on breast muscle fiber development in the offspring of broiler breeders. // Anim Biosci - 2021 - Vol - NNULL - p.; PMID:33902177
- Taniguchi S., Zhu Z., Matsuzaki M., Tsudzuki M., Maeda T. 5-aminolevulinic acid improves chicken sperm motility. // Anim Biosci - 2021 - Vol - NNULL - p.; PMID:33902172
- Li W., Geng Z., Zhou XH. Causal mediation analysis with sure outcomes of random events model. // Stat Med - 2021 - Vol - NNULL - p.; PMID:33902164
- Junqueira FMD., Nadal JAH., Brandão MB., Nogueira RJN., de Souza TH. High-frequency oscillatory ventilation in children: A systematic review and meta-analysis. // Pediatr Pulmonol - 2021 - Vol - NNULL - p.; PMID:33902159
- Webb C., Chang YH., Pockaj BA., Gray RJ., Stucky CC., Wasif N. Lymph node positivity and association with long-term survival for different histologies of appendiceal cancer. // J Surg Oncol - 2021 - Vol - NNULL - p.; PMID:33902156
- Fontao M., Schorer L., Ross T. . // Fortschr Neurol Psychiatr - 2021 - Vol - NNULL - p.; PMID:33902150
- Eddicks M., Eddicks L., Stadler J., Hermanns W., Ritzmann M. // Tierarztl Prax Ausg G Grosstiere Nutztiere - 2021 - Vol49 - N2 - p.120-132; PMID:33902142