Choledocholithotomy is an operation to remove stones from the common bile duct through an incision. The main indication for surgery is choledocholithiasis .
The operation is performed if endoscopic treatment for choledocholithiasis is ineffective or impossible.
A necessary condition for performing this operation is intraoperative cholangiography through the cystic duct under x-ray control to exclude “silent” stones in the common bile duct.
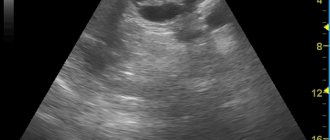
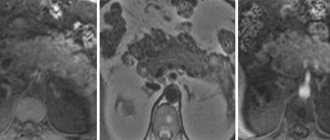
Intraoperative cholangiography Stone in the distal common bile duct
Why is endoscopy performed?
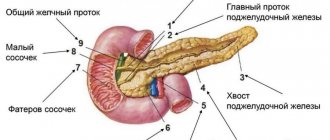
Endoscopic retrograde cholangiopancreatography is performed for differential diagnosis of patency of the biliary tract and pancreatic ducts (narrowing of the ducts, tumors, stones, etc.). In the treatment of diseases of the gallbladder and pancreas (cyst, tumor, polyps, etc.) and for hidden bleeding, anemia, Crohn's disease, etc. Endoscopic examination allows you to identify changes in the bile ducts and pancreatic ducts, indicate the exact location of the lesion, and take a biopsy or urgently operate.
Uncomplicated gallstone disease: how to get rid of stones without surgery
Uncomplicated cholelithiasis: biliary sludge; dissolution of cholesterol gallstones in the gallbladder, if it is impossible to remove them by surgical or endoscopic methods; prevention of recurrent stone formation after cholecystectomy.
Dissolving gallstones
If stones have been established in the gall bladder, this does not mean that it is necessary to immediately undergo surgery to remove it. First, it is worth trying other methods of getting rid of stones: crushing them using equipment or dissolving them with medication. Special equipment and doctors working on it cannot be found in every clinic, but drugs that dissolve gallstones are available in every pharmacy. Moreover, both methods do not provide a 100% guarantee of results. However, the cost of shock wave lithotripsy (hardware crushing method) is an order of magnitude higher in comparison with drugs that must be taken throughout the year.
Three types of stones can form in the gallbladder:
- pigmented (they consist of lime and bilirubin);
- cholesterol;
- mixed (from cholesterol, bilirubin and lime)
It is believed that in 90% of cases cholesterol stones are “born” in the gallbladder. But do not underestimate other stones. The origin of stones is associated with an imbalance between cholesterol produced by liver cells and bile acids. When their correct ratio is disturbed, a precipitate of bile begins to form. Subsequently, stones are formed from the sediment. The action of medications is aimed at dissolving such cholesterol stones. At the same time, pigmented or mixed stones cannot be dissolved and the gallbladder must be removed.
There are currently various drugs on the pharmaceutical market aimed at dissolving gallstones. Basically, these are drugs based on bile acids. They can only be used if there is confirmation that the stones are cholesterol. One of the best developments in this direction is considered to be a drug based on ursodeoxycholic acid - ursosan. When used, the reproduction of cholesterol in the liver and the absorption of cholesterol in the intestine are reduced. Once in the gallbladder, this acid creates certain conditions for the stones to dissolve on their own. On the one hand, cholesterol synthesis in the liver is suppressed, its concentration in bile is reduced, and on the other hand, the synthesis of bile acids is stimulated. Bile acid preparations have been used for liver diseases and cholestatic diseases for several decades and have proven success in this direction.
How is endoscopy performed?
An endoscopic examination is performed using an optical device - a duodenofiberscope. A flexible probe equipped with an optical system is inserted through the patient's mouth into the major duodenal papilla. Using an optical fiberscope, a contrast agent is injected into a special plastic tube, which helps to “see” the paths of the gallbladder and large ducts of the pancreas. During such a precise examination, if necessary, endoscopic mini-invasive surgery of the affected areas is simultaneously performed. This is important in situations of blockage of the bile ducts at the common mouth of the bile ducts, internal bleeding, etc. During endoscopy of the bile ducts and pancreatic ducts, tissue samples can be extracted to determine the cause of the blockage and determine the microflora of the stomach or if a tumor process is suspected. The tissue is used for cytological and other studies. Special instruments are used to remove stones from the bile ducts.
Activities after removal of gallstones
The duration of the postoperative period after such a procedure is determined by the method of stone extraction or cholecystectomy. To prevent the development of various complications, speedy tissue regeneration in the area of surgical intervention, speedy restoration of the functional activity of the liver, structures of the hepatobiliary system, the following measures are taken:
- The diet after removal of gallstones is aimed at reducing the functional load on the liver, hepatobiliary system, and excludes the consumption of fatty, fried, spicy foods, marinades, pickles, and alcohol. This diet must be followed for at least one month after the procedure.
- Limiting physical activity is necessary for high-quality healing of the postoperative wound and prevention of suture dehiscence.
- Medications – if necessary, antibiotics, anticoagulants, anti-inflammatory and painkillers are used.
Specialists from the surgical department of the SKZD hospital in Rostov-on-Don provide treatment for diseases of the hepatobiliary system, maximally aimed at preserving its anatomical integrity and functional activity.
How is anesthesia used during the procedure?
Endoscopic examination is performed using short-acting agents that are quickly eliminated from the body. They cause slight relaxation and drowsiness.
An injection of contrast agent is given intravenously immediately before endoscopy. The patient is asked to lie on his left side, the endoscope tube is inserted through the mouth and the examination begins. The study is carried out in a hospital setting. The endoscopy procedure is painless and comfortable. A sore throat goes away within 30 minutes.
During endoscopy of the bile ducts and pancreatic ducts, local anesthesia with a special aerosol is used to numb the mouth and pharynx, relieve discomfort and improve breathing when installing an optical device. The doctor directs the endoscope (the diameter of the endoscope is like a small piece of sugar) through the mouth and pharynx - into the esophagus, stomach, and into the duodenal papilla - the lumen of the duodenum. The monitor screen shows the real condition of the bile ducts and pancreatic duct: cysts, stones, inflammation, narrowing, cicatricial stenosis or neoplasm. Based on the examination, the endoscopist makes an accurate diagnosis. According to indications, successful treatment is carried out (95% success).
Endoscopic examinations can be performed while the patient is sleeping. A sleeping pill is administered intravenously under the supervision of an anesthesiologist. For invasive surgery (in certain cases), general anesthesia may be used.
30 minutes after endoscopy of the bile ducts and pancreatic ducts, patients return to normal life.
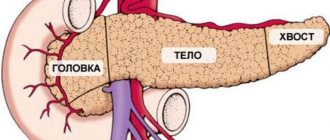
Operations on the gallbladder, biliary tract and pancreas
Who is indicated for gallbladder removal?
We remove the gallbladder if there are stones (calculi) in it and if there are gall bladder polyps.
The operation is indicated in all patients with stones with clinical manifestations (attacks of pain, dull pain and discomfort in the subcostal region, nausea and intolerance to fatty foods) and a complicated course of gallstone disease (attacks of acute cholecystitis, pancreatitis, previous obstructive jaundice, stones in the bile ducts and etc.).
In case of asymptomatic gallstone disease, a prophylactic cholecystectomy can currently be performed to prevent its complications of gallstones, especially in the presence of small stones in the gall bladder and in persons of certain professions and lifestyles (long business trips, expeditions, etc.). Prophylactic removal of the gallbladder is possible in the absence of a high risk of surgery through the use of laparoscopy.
Why is it better to perform the operation in?
Our center uses three laparoscopic techniques - classic laparoscopic cholecystectomy, minilaparoscopic cholecystectomy, cholecystectomy through a single laparoscopic approach (SILS - single incision laparoscopic surgery). Operations are performed at an expert level using equipment from the German company Karl Storz.
The laparoscopic cholecystectomy technique in our center is performed in accordance with the clinical recommendations of the European Society of Endoscopic Surgeons for the prevention of bile duct injuries.
Regardless of the method of removing the gallbladder during surgery, in real time in our center, if there are clinical indications, the bile ducts are examined by cholangiography using a C-arm, which allows, if necessary, one-stage elimination under anesthesia of pathological findings detected during cholangiography changes in the bile ducts (stones, narrowing) by using the antegrade endoscopic papillosphincterotomy technique.
Cholangiography is a mandatory method for intraoperative examination of the bile ducts in case of indications of jaundice, dilatation of the ducts, previous attacks of pancreatitis, girdle pain - especially in patients with small stones in the gall bladder. An alternative, highly informative, painless and safe method for examining the bile ducts is magnetic resonance imaging (MRI cholangiography), which is performed in our center before surgery and can be performed in most patients.
This method allows the surgeon to know before surgery about possible anomalies in the structure of the bile ducts and the presence of pathological changes. The MRI cholangiography method allows avoiding radiation exposure during surgery by eliminating cholangiography. The duration of a comfortable stay in the hospital after a low-traumatic method of removing the gallbladder is usually 2-3 days. Classic laparoscopic cholecystectomy is a generally accepted technique in the world, performed under general anesthesia through four accesses, length from 6 mm to 10 mm with the expansion of one of the accesses to 20-40 mm to remove the gallbladder.
Figure - Symbolic diagram of the location and size of punctures during classical laparoscopic removal of the gallbladder
Minilaparoscopic cholecystectomy
Minilaparoscopic cholecystectomy is performed with instruments with an external diameter of 3 to 5 millimeters; removal of the gallbladder is performed through an umbilical approach. This technique is exclusive in that it is least traumatic and leaves barely noticeable postoperative scars, as it is performed using ultra-small punctures (approaches).
Figure - Symbolic diagram of the location and size of punctures during minilaparoscopic cholecystectomy
Cholecystectomy through a single laparoscopic approach allows you to relieve the patient from cholelithiasis through an inconspicuous access in the area of the skin fold of the navel 2.5-3 cm long. The technique has the greatest cosmetic advantages over other methods of removing the gallbladder and is advisable in patients with large stones in the gallbladder with a diameter of more than 2 centimeters, as well as when combined with an umbilical hernia. 1-2 years after this technique, an inconspicuous postoperative scar forms along the skin fold of the navel in most patients.
Figure - Postoperative scar in the navel area after a single laparoscopic approach
Cholecystectomy through a mini-access is performed in patients with high anesthetic risk and concomitant diseases in which the use of laparoscopy is contraindicated. The length of the mini-access in most patients is from 4 to 8 cm. The course of the postoperative period during cholecystectomy through the mini-access differs little from the laparoscopic method of surgery.
Treatment options for cholelithiasis
Conservative treatment is possible in the initial stages of cholelithiasis in the absence of signs of severe cholecystitis and complications. It is aimed at eliminating the conditions for stone formation, normalizing metabolic processes, improving the mobility of the biliary tract, and reducing the activity of the inflammatory process in them.
In other cases, surgical treatment is indicated - cholecystectomy, during which the gallbladder with stones is removed. It can be carried out in two ways:
- laparotomy. An incision of 15-20 cm in length is made in the abdominal wall. Due to the traumatic nature, the indications for this technique have now significantly narrowed. It is necessary only in case of gallbladder rupture, bile peritonitis, or if there are contraindications to the laparoscopic method. However, surgeons who are not proficient in laparoscopy still actively practice laparotomy when performing cholecystectomy;
- laparoscopically. Removal of the gallbladder using video endoscopic equipment and endoscopic instruments through one access 1-2.4 cm long or several accesses 0.3-1 cm long is recognized today as the best method of surgical treatment of cholelithiasis. For example, what technique is used at the Swiss University Clinic in Moscow.