Cancer of the papilla of Vater (cancer of the major duodenal papilla) is a malignant tumor located in the place where the common bile duct flows into the duodenum.
Causes of the disease
Causes and predisposing factors:
- Genetic predisposition. It is often detected in families with familial adenomatous polyposis. Also, in some patients, a cellular mutation of the K-ras gene is detected.
- BDS adenoma is a benign tumor of the papilla that can become malignant.
- Chronic diseases of the gallbladder and liver.
- Chronic pancreatitis.
Symptoms and course of the disease
Cancer of the papilla of Vater is detected in the early stages of development, due to narrowing of the final section of the biliary tract. This leads to wavy yellowing of varying intensity of the skin, which is accompanied by itching. And refusal to eat, indigestion, fever, vomiting leads to weight loss. Due to a violation of the outflow of bile, the liver becomes enlarged, and a full gallbladder can be palpated through the abdominal wall. Obstruction of the excretory ducts is also reflected in the state of the blood.
In blood plasma it is noted:
- increased activity of gamma-glutamyl and alkaline phosphatase;
- bilirubin increases significantly;
- increase in transaminase.
Treatment of the disease
The only radical treatment method is surgery . Most often, pancreatoduodenal resection is performed - removal of part of the duodenum, stomach and part of the pancreas with adjacent lymph nodes.
Radiation therapy and chemotherapy are of secondary importance . Chemotherapy is also used for metastases.
Palliative endoscopic intraductal interventions in case of severe narrowing of the common bile duct, if it is impossible to perform radical intervention. This type of operation includes papillotomy (dissection of the papilla of Vater) followed by stenting. This helps normalize the passage of bile.
For effective treatment of cancer of the major duodenal papilla, high-quality early diagnosis is important.
Vater's Nipple
Vater's Nipple
[
papilla duodeni major
(PNA);
named after the German anatomist Vater (A. Vater, 1684-1751); synonym: major duodenal papilla, major duodenal papilla, papilla Vateri
] - an elevation on the inner surface of the wall of the duodenum, corresponding to the place where the common bile duct and pancreatic duct enter the duodenum.
Rice.
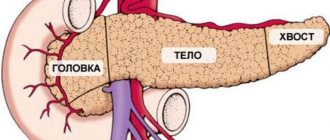
Macropreparation of a part of the duodenum (the intestinal lumen is opened): I - descending part of the duodenum, II - horizontal part of the duodenum; 1 - Santorini nipple (small); 2 - papilla of Vater (major duodenal papilla); 3 - probe inserted into the common bile duct. Vater first described this formation in 1720. The width of Vater's nipple is about 4 mm, height up to 7 mm; most often it is located approximately in the middle of the descending part of the duodenum (see). Its origin is associated with the passage of the common bile duct (ductus choledoehus) and the pancreatic duct, or Wirsung's duct (ductus pancreaticus, s. ductus wirsungi) in this section of the intestinal wall. The common bile duct lifts its mucous membrane in the form of a longitudinal fold, at the base of which the papilla of Vater is formed (Fig.) Most often, in the area of the papilla of Vater, the common bile duct expands, forming the hepatopancreatic ampulla (ampulla hepatopancreatica), into which the pancreatic duct flows (see .), and both ducts open on the nipple of Vater with one common opening. There are other options for the flow of these ducts into the duodenum (see Bile ducts). In the circumference of the hepatopancreatic ampulla, in the thickness of the papilla of Vater, there are ring oblique and longitudinal muscle bundles that intertwine with each other and form the sphincter of the hepatopancreatic ampulla, or the sphincter of Oddi (sphincter ampullae liepatopancreaticae, s. sphincter Oddi), functioning independently of the duodenal muscles intestines. The common bile duct and the pancreatic duct at their confluence have independent sphincters (sphincter ductus choledochi, sphincter ductus pancreatici).
The blood supply to the papilla of Vater is carried out by the ventral and dorsal branches of the retroduodenal arteries (aa. retrod uodenales). Venous outflow of blood occurs through the anterior and posterior pancreatoduodenal veins (vv. pancreaticoduo-denales), flowing into the superior mesenteric vein (v. mesenterica sup.). Lymphatic vessels are connected with the lymphatic vessels of the terminal part of the common bile duct, duodenum and head of the pancreas and communicate with the lymph nodes of the root of the mesentery of the colon. The vagus nerve and sympathetic fibers of the celiac plexus (plexus celiacus) are involved in the innervation of the nipple of Vater.
The nipple of Vater, in particular the sphincter of the hepatopancreatic ampulla, as well as the sphincters of the common bile duct and pancreatic duct play a major role in regulating the flow of bile (see) and pancreatic juice into the duodenum and preventing duodenobiliary and duodenopancreatic reflux (see). When these sphincters relax, bile and pancreatic juice enter the duodenum; when they contract, their flow into the intestine stops, and the bile is sent through the cystic duct into the gallbladder (see). Secretory pressure of the liver (see), motility of the gallbladder, tone of the walls of the bile ducts, peristalsis of the duodenum, etc. also play a role in the mechanism of movement of bile into the duodenum.
Methods for studying the papilla of Vater include: duodenal intubation (see), duodenography (see, Relaxation duodenography), duodenoscopy (see), endoscopic retrograde cholangiopancreatography (see, Retrograde pancreatocholangiography), cholangiography (see), intravenous choleography (see. ), choledochomanometry, choledochoscopy (see), ultrasound examination of the bile ducts and pancreas (see Ultrasound diagnostics), computed tomography (see Computer tomography).
Diseases of the Vater's nipple are clinically manifested by stenosis syndrome (see Stricture). According to V.V. Vinogradov (1962), stenosis of the papilla of Vater was observed in approximately 26% of patients who underwent surgery on the bile ducts for non-tumor diseases.
The causes of Vater's nipple stenosis are varied. In some cases, stenosis of the nipple of Vater is congenital. Some researchers point to the possibility of stenosis of the Vater's nipple, caused by functional disorders such as dyskinesia (see), in which there is a prolonged spasm of the sphincter of the hepatopancreatic ampulla, alternating with its atony. These disorders are usually combined with similar disorders of the bile ducts and gallbladder and can also be observed in diseases of the stomach (see), pancreas, and duodenum. Most often, Vater's nipple stenosis occurs with cholelithiasis (see) due to the frequent passage of sand and small stones, as well as with duodenitis (see), cholangitis (see), pancreatitis (see), as a result of Vater's inflammation that occurs with these diseases nipple - acute or chronic papillitis.
Morphologically, in the initial stage of stenosis of the papilla of Vater, swelling and leukocyte infiltration of its walls are observed. Later, an atrophic or hypertrophic process is found in the mucous membrane of the hepatopancreatic ampulla, often with hyperplasia of the glandular apparatus and the formation of adenomatous growths.
In the muscular apparatus of the sphincter of the ampulla, connective tissue develops, sclerotic and cicatricial changes occur, leading to a narrowing of the nipple of Vater. Sometimes these changes spread to the excretory sections of the common bile duct and pancreatic duct.
The clinical picture of Vater's papilla stenosis consists of symptoms of biliary hypertension, and in the most severe cases - cholangioedema and obstructive jaundice (see), and these phenomena are often temporary, and jaundice is remitting. Pain in the right hypochondrium is observed in the vast majority of patients. In approximately 30-40% of patients, stenosis of the papilla of Vater is accompanied by a picture of recurrent pancreatitis associated with congestion in the pancreas caused by blockage of the pancreatic ducts. The severity of the wedge, manifestations depends on the degree of stenosis of the Vater's nipple, which can be compensated, subcompensated and decompensated.
Diagnosis of Vater's nipple stenosis is difficult, since its main clinical symptoms are not specific; they are also observed in gallstone disease, cholangitis, duodenitis, pancreatitis and other diseases with which stenosis of the papilla of Vater is often combined. The diagnosis of Vater's papilla stenosis can sometimes be clarified by multi-stage duodenal intubation, intravenous cholegraphy, and duodenoscopy using fiber optics. The most effective way to diagnose stenosis of the papilla of Vater is to examine the common bile duct during surgery (probing, cholangiomanometry, cholangiography, choledochoscopy).
Treatment of functional stenosis of the nipple of Vater is conservative (antispasmodic and antihistamines, choleretic agents, and, if indicated, antibiotics and sulfonamides). Surgical treatment of organic stenosis of the nipple of Vater. In case of isolated stenosis of the papilla of Vater and the absence of inflammatory phenomena in it and the wall of the duodenum, operations are performed on the papilla of Vater - bougienage, transduodenal papillotomy (dissection of the mucous membrane of the papilla of Vater), transduodenal papillosphincterotomy (dissection of the mucous membrane of the papilla of Vater and the sphincter of the hepatic-pancreatic ampulla) and papillosphincteroplasty (stitching after papillosphincterotomy of the edges of the dissected mucous membrane of the duodenum and hepatic-pancreatic ampulla); A less traumatic method of endoscopic papillosphincterotomy has become widespread - dissection of the sphincter with a special instrument - a papillotome inserted through the biopsy channel of the endoscope (see Endoscopy). When stenosing cicatricial-sclerotic changes spread to the common bile duct, the presence of stenosing pancreatitis (blocking the flow of bile as it passes through the head of the pancreas) and inflammatory phenomena in the wall of the papilla of Vater and the duodenum, choledochotomy (see), choledochostomy (see. ) or bypass biliary anastomoses are applied (see Choledochoduodenostomy, Cholecystoenterostomy).
In some cases, papillosphincterotomy and supraduodenal choledochoduodenostomy are indicated. For example, when Vater's nipple stenosis is combined with stenosing pancreatitis, bypass choledochoduodeno-anastomosis eliminates obstruction of the common bile duct, and papillosphincterotomy restores the patency of the pancreatic duct.
The prognosis for isolated stenosis of the nipple of Vater in cases of restoration of bile outflow is favorable. When Vater's nipple stenosis is combined with other diseases, the prognosis depends on the nature of these diseases and the operations used.
Neoplasms of the papilla of Vater include benign and malignant (cancerous) tumors that arise in the mucous membrane of the duodenum covering the papilla of Vater, the hepatopancreatic ampulla and the mouth of the common bile duct or pancreatic duct.
Benign tumors of the papilla of Vater are quite rare. More often these are papillomas (see Papilloma, papillomatosis) or adenomas (see Adenoma), which form the hepatopancreatic ampulla and prolapse into the lumen of the duodenum. The tumor sizes range from a few millimeters to 3-4 cm in diameter. Most often, tumors consist of mature epithelial cells and have a glandular structure; Often they exhibit pronounced inflammation.
The main clinical manifestations of benign tumors of the nipple of Vater are associated with its obstruction (pain in the right hypochondrium, intermittent jaundice, symptoms of recurrent pancreatitis). Sometimes blood is found in the duodenal contents. The most effective diagnostic method is visual examination of the papilla of Vater during fibroduodenoscopy, during which a tumor biopsy can be performed (see Biopsy). Treatment of benign tumors of the Vater's nipple is surgical (papillectomy). The prognosis for timely removal of the tumor is favorable. In some cases, malignancy of the tumor is possible.
Cancer of the papilla of Vater (see Cancer), according to various researchers, occurs in approximately 5 - 10% of patients with malignant neoplasms of the hepatobiliary and pancreaticoduodenal zones.
Macroscopically, the cancerous tumor of the Vater's nipple looks like a solitary node, polyp or ulcer. The solitary node causes prolapse of the nipple of Vater and a gaping of its mouth, through which bleeding tumor masses are visible. Polypous forms resemble cauliflower. A cancerous ulcer is usually irregular in shape with dense, undermined edges, a bleeding bottom and purulent overlays. Sometimes the tumor infiltrates neighboring tissues, spreading to the duodenum, common bile duct and pancreas. Microscopically, adenocarcinoma is most often detected with a picture of solid or mucinous cancer. Cancer of the Vater's nipple is characterized by relatively slow growth, but obstruction of the Vater's nipple develops already at the beginning of the disease. Metastasis occurs to regional lymph nodes, and later to distant organs.
The disease usually occurs in middle and old age, more often in men. Sometimes at the onset of the disease, patients experience pain resembling biliary colic, weakness, general malaise, and increased body temperature. However, more often the early symptom of the disease is jaundice, which is often permanent, followed by dyspeptic symptoms (anorexia, nausea, feeling of heaviness in the epigastric region), weakness, weight loss; sometimes, due to concomitant cholangitis, body temperature rises. During a clinical examination of the patient, an enlarged liver is determined and an enlarged, painless gallbladder is palpated (Courvoisier's symptom). Data from laboratory clinical studies (blood, urine, feces, etc.) indicate the presence of obstructive jaundice; Blood and atypical cancer cells can be found in the duodenal contents.
The diagnosis of Vater's nipple cancer is made based on data from a clinical examination of the patient and results obtained using instrumental research methods (see above). Significant assistance is provided by x-ray examination of the duodenum and bile ducts. The most effective method for diagnosing cancer of the papilla of Vater is fibroduodenoscopy, in which you can directly see changes in the papilla of Vater and perform a biopsy of the tumor.
Treatment for Vater's nipple cancer is only surgical. For localized tumors, transduodenal excision of the papilla of Vater (papillectomy) is performed. In cases of tumor germination of the wall of the duodenum or its spread to the pancreatic duct and common bile duct, pancreaticoduodenectomy (removal of the head of the pancreas and duodenum) or total pancreaticoduodenectomy (see). If it is impossible to remove the tumor or there are distant metastases, bypass biliary anastomoses are performed.
The prognosis for cancer of the Vater's nipple depends on the timeliness of the radical operation and the nature of the operation. According to many surgeons, radical surgery for cancer of the Vater's nipple is possible in 50-70% of patients; it often gives encouraging results.
Bibliography:
Aripov U. A. et al. Operations on the large duodenal nipple and pancreas, Tashkent, 1978; Balalykin A. S., Kornilov Yu. M. and Revyakin V. I. Endoscopic sphincterotomy of the ampulla of the papilla of Vater for obstructive jaundice, Sov. med., no. 11, p. 45, 1979; In ii n o-gradov V.V. Diseases of the Vater's nipple, M., 1962, bibliogr.; G r i sh k e-v i h E. V. Clinic, diagnosis and surgical treatment of stenosis of the papilla of Vater, Klin, hir., No. 7, p. 12, 1965; N i-d e r l e B. et al. Surgery of the biliary tract, trans. from Czech, Prague, 1982; S a-v e l e v V. S., Buyanov V. M. and B a l a l y k i n A. S. Endoscopy of the abdominal organs, M., 1977; Shkrob O. S., Lopata Yu. M. and Safronov V. V. Diagnostic value of special research methods for obstructive jaundice, Surgery, No. 9, p. 48, 1973; Fodisch HJ Feingewebliche Studien zur Orthologie und. Pathologie der Papilla Vateri, Stuttgart, 1972; Mattig H. Papilla Vateri, Lpz., 1977; The papilla vateri and its diseases, ed. by M. Classen ao, Baden-Baden ao, 1979.
D. F. Blagovidov, A. S. Yakovlev.
Diagnosis of the disease
Diagnostic program:
- Consultation with a qualified specialist.
- Detailed blood tests, including general clinical, biochemical, electrolyte composition, lipid profile, determination of tumor markers, pancreatic enzymes, glycosylated hemoglobin.
- Ultrasound examination of the abdominal organs with Dopplerography of the abdominal vessels; Spiral computed tomography of the abdominal cavity.
- Combined positron emission computed tomography.
- Endoscopic and laparoscopic ultrasonography.
- Esophagogastroduodenoscopy with test for Helicobacter pylori (under anesthesia).
- Tumor biopsy.
- Urgent histopathology and histochemistry of biopsy material.
- Magnetic resonance cholangiopancreatography (as an option).
Advantages of treatment in Israel
- Qualified specialists who are fluent in the methods of treating this disease.
- Equipping clinics with high-tech equipment.
- Application of innovative therapeutic methods and drugs.
- Carrying out treatment according to an individual comprehensive program.
- Reasonable prices.
The earlier treatment is started, the higher your chances of recovery. Therefore, do not waste time, choose a clinic and restore your health under the guidance of experienced oncologists.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
Prices
| Disease | Approximate price, $ |
| Prices for thyroid cancer screening | 3 850 — 5 740 |
| Prices for examination and treatment for testicular cancer | 3 730 — 39 940 |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing esophageal cancer | 14 380 — 18 120 |
| Prices for diagnosis and treatment of ovarian cancer | 5 270 — 5 570 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for breast cancer diagnostics | 650 — 5 820 |
| Prices for diagnosis and treatment of myeloblastic leukemia | 9 600 — 173 000 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for treatment of colorectal cancer | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for liver cancer treatment | 55 960 — 114 060 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of myelodysplastic syndrome | 9 250 — 29 450 |
| Prices for leukemia treatment | 271 400 — 324 000 |
| Prices for thymoma treatment | 34 530 |
| Prices for lung cancer treatment | 35 600 — 39 700 |
| Prices for melanoma treatment | 32 620 — 57 620 |
| Prices for treatment of basal cell carcinoma | 7 700 — 8 800 |
| Prices for the treatment of malignant skin tumors | 4 420 — 5 420 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for craniotomy | 43 490 — 44 090 |
| Prices for thyroid cancer treatment | 64 020 — 72 770 |
| Prices for treatment of bone and soft tissue cancer | 61 340 — 72 590 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Testicular cancer treatment prices | 15 410 |
| Bladder cancer treatment prices | 21 280 — 59 930 |
| Prices for cervical cancer treatment | 12 650 — 26 610 |
| Prices for treatment of uterine cancer | 27 550 — 29 110 |
| Prices for treatment of ovarian cancer | 32 140 — 34 340 |
| Prices for treatment of colon cancer | 45 330 |
| Prices for lymphoma treatment | 11 650 — 135 860 |
| Prices for kidney cancer treatment | 28 720 — 32 720 |
| Prices for breast reconstruction after cancer treatment | 41 130 — 59 740 |
| Prices for breast cancer treatment | 26 860 — 28 900 |
| Prices for prostate cancer treatment | 23 490 — 66 010 |
Forecast
The success of treatment and further prognosis largely depend on the stage at which the disease is diagnosed. Inflammatory processes in the area of the nipple of Vater can be successfully treated with medication.
Usually, if the function and patency of the canal is preserved, then after a course of treatment the problem goes away.
In case of oncological diseases of the organ, the chances of a successful outcome largely depend on timely surgery, the stage of the disease and the body’s response to chemotherapy.