Hemangioma is a benign neoplasm, which is a tangle of dilated blood vessels. It is not associated with cancer and cannot transform into cancer, but sometimes causes complications.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
Most often, hemangiomas are found on the skin of the face, scalp, chest, and back. But there are also other localizations. On the skin, such formations in most cases are within the competence of pediatric surgeons, since they arise during the first months of life. Some children undergo surgical treatment; in some, “vascular tumors” disappear on their own by 5–10 years, and in some they persist until adulthood.
In addition, there are some special types of hemangiomas, which are usually diagnosed in adults.
The Medicine 24/7 clinic uses all modern types of treatment for hemangiomas of any location. We employ expert-level surgeons and use modern equipment. Our specialists remove tumors as carefully as possible, using minimally invasive, least traumatic methods. After the interventions, patients quickly recover and return to their normal lives.
Types of benign esophageal tumor
There are two types of benign tumors - epithelial (polyps, adenomas, epithelial cysts) and non-epithelial (leiomyomas, fibromas, neuromas, hemangiomas, etc.), which are much more common. Polyps and adenomas can be localized at any level of the esophagus, but more often they are located at the proximal end or in the abdominal region. These tumors may have a broad base or a long stalk.
In the latter case, they sometimes become pinched in the area of the cardia or fall out of the esophagus into the pharynx, causing corresponding symptoms. These are usually well-circumscribed, reddish, sometimes lobular tumors. When the vessels are located superficially, they bleed easily when touched. These formations should not be confused with the more common papillomatous growths on the mucous membrane of the esophagus, which occur in older people due to chronic inflammatory changes. Such papillomas do not reach large sizes. Cysts are not true tumors and arise due to blockage of the mucous glands of the gong esophagus due to improper embryonic development of the organ.
Rarer benign tumors of the esophagus include fibromas, neuromas, lipomas, hemangiomas, and lymphangiomas. These tumors have a characteristic structure. Fibromas and neuromas are more dense, are often located in the outer layers of the esophagus and originate from the membranes of the nerve trunks or the tissue surrounding the esophagus. They closely adhere to the wall of the esophagus and grow, pushing its muscle layer apart. Often such tumors have the histological structure of neurofibroma. Lipomas, lymphangiomas and hemangiomas are soft and do not always form clear boundaries of distribution along the esophagus and in surrounding tissues.
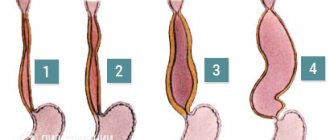
Among benign tumors of the esophagus, leiomyomas are the most common - up to 70 - 95%. Leiomyomas arise from the smooth muscle lining of the esophagus or from the muscular elements of the mucous membrane. They usually have the appearance of a single node with polycyclic contours, less often they consist of several nodes, sometimes interconnected and entwining the esophagus over a considerable length. Located in the thickness of the muscular wall of the esophagus, leiomyoma expands it, thins it, stretches the unchanged mucous membrane, prolapses into the lumen of the esophagus, causing narrowing and dysphagia. The tumor consists of bundles of smooth muscle alternating with areas of fibrous connective tissue. When connective tissue develops in a tumor, it is referred to as fibromyoma.
Cherry spots
Other names for this pathology are cherry angiomas, Campbell de Morgan spots, senile angiomas. They usually appear in middle age and old age and resemble red-purple “beads” on the skin, sometimes they are flat. Their color can also be purple, in rare cases dark brown or even black. At first they are no larger than the head of a pin, but over time their size and number can increase.
Cherry hemangiomas in adults are approximately equally common in people of different races and ethnicities, but are more noticeable on fair skin. Women and men get sick approximately equally often.
Campbell de Morgan spots are not dangerous; they do not transform into malignant tumors. There are two main indications for their removal:
- If the hemangioma is constantly injured and bleeds.
- For cosmetic reasons - if the formation is located in a noticeable place and spoils the appearance.
Classical excision of cutaneous hemangiomas with a scalpel is now rarely resorted to, as more convenient and safe techniques have appeared. Today, hemangiomas are often removed with a laser. There is a device for radio wave surgery called Surgitron. In it, instead of a laser, high-frequency radio waves play the role of a scalpel. You can remove formations on the skin using an electrocoagulator - an instrument that burns tissue with an electric current. Sometimes they resort to cryosurgery - the destruction of hemangiomas using low temperatures.
All these interventions can be performed without anesthesia, under local anesthesia. No hospitalization is required. On the same day, the patient can return home and do their usual activities. A scar on the skin may remain if the hemangioma was large.
You should not remove “cherry stains” yourself at home. If even a small hemangioma is damaged, it can bleed heavily and there is a risk of infection. Consult a medical specialist.
Take care of yourself, book a consultation now
Symptoms of a benign esophageal tumor
Small benign tumors of the esophagus are quite common. They do not cause clinical manifestations and are often unexpectedly discovered at autopsy. The disease manifests itself with the onset of dysphagia. Benign tumors rarely cause esophageal obstruction. Dysphagia was observed in only 50% of patients. With large tumors, in addition to dysphagia, patients experience a sensation of a foreign body in the esophagus, vomiting and nausea, and sometimes pain when eating. It happens that large tumors do not cause any symptoms and are accidentally detected during an X-ray examination.
Unlike esophageal cancer, dysphagia in benign tumors does not tend to steadily and rapidly increase and can remain unchanged for several months or even years. In the anamnesis of some patients, periods of improvement in the passage of food due to a decrease in spasms are noted. The course of benign tumors is long; with non-epithelial tumors of the esophagus, patients live a long time, and the tumor does not show a significant tendency to grow. The general condition of patients with an esophageal tumor does not suffer. Sometimes there is some weight loss due to eating disorders and natural anxiety in such cases.
Diagnosis of benign esophageal tumor
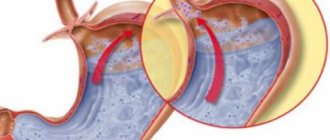
Clinical signs allow one to suspect a disease of the esophagus, but a final diagnosis of a benign tumor can only be made based on a comparison of the results of X-ray and endoscopic examinations. X-ray examination of intramural and intraluminal formations. X-ray signs of a benign intramural tumor: a sharply defined filling defect, displacement of the lumen of the esophagus at the level of the tumor, and in certain projections - expansion.
When the defect is located marginally, the angle between the edges of the tumor and the normal wall of the esophagus approaches an acute one. Folds of the mucous membrane are detected only on the wall opposite the tumor. According to the defect, against the background of the posterior mediastinum, a semi-oval shadow of the tumor is often found, forming, together with the defect, a semblance of a ball. When the tumor is lobular and its nodes are located at different levels, a contrast suspension filling the hollows between individual protrusions creates a picture of intersecting contours.
The described x-ray picture is typical for a benign intramural tumor of the esophagus, regardless of its histological characteristics (leiomyoma, fibroma, lipoma, neuroma, etc.), as well as for a cyst of the esophageal wall. X-ray signs of a benign intraluminal tumor (polyp): variegated single (less often multiple) filling defects with clear, smooth contours, which seem to flow around a contrast suspension and shift along with the wall of the esophagus. When the polyp has a stalk. the filling defect moves. The peristalsis of the esophageal wall in the area where the polyp is located is characteristic. With benign tumors, there is no circular damage to the esophagus and stretching of the opposite wall, so suprastenotic dilatation of the esophagus usually does not occur.
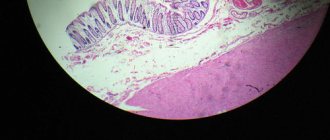
Confirmation of the diagnosis of a benign tumor of the esophagus can be obtained by esophagoscopy. For intraluminal tumors arising from the mucous membrane of the esophagus. a biopsy can be performed. With an intramural tumor, esophagoscopy reveals the preservation of the mucous membrane and the approximate localization of the formation. Biopsy for such tumors is contraindicated for two reasons. Firstly, it is most often impossible due to the deep location of the tumor in the wall of the esophagus. Secondly, injury to the mucous membrane is usually accompanied by infection and complicates subsequent surgical intervention.
Treatment.
The only treatment provided is surgical intervention, after which the patient must strictly adhere to the prescribed diet in order to avoid the risk of complications.
If possible, the tumor is removed with a special flexible tube. Depending on the size and type of tissue, not only the tumor, but also part of the esophageal wall may be removed. In cases where this method does not help, the chest and abdominal cavities are opened, through which the tumor is removed.
Also, an important part of the treatment is following a diet; “Table No. 1” will become very relevant; to get acquainted with the menu, just visit the website Menu of Table No. 1. This menu should be alternated with the menu of other tables recommended by the doctor.
Treatment of benign esophageal tumor
For benign tumors, treatment should only be surgical. Due to the slow growth of these tumors, surgical treatment is indicated only in cases of dysfunction of the esophagus and painful symptoms, provided there is no increased risk of surgery. Observation is permissible if regular endoscopic examination is possible in one medical institution, so that in case of deterioration, indications for surgery can be established in a timely manner. When planning treatment, it is necessary to take into account that the benignity and malignancy of a tumor can be judged only after a histological examination, which is possible only after a biopsy of the formation. Removing the tumor at an early age saves the patient from possibly more extensive and difficult surgery in the future.
Epithelial tumors located on a long and narrow stalk can be removed through an esophagoscope. In other cases, given the possibility of malignancy of the polyp, which often begins at the base, it is more advisable to perform esophagotomy, excision of the tumor under visual control with histological examination. In rare cases, with large polyps and it is impossible to exclude malignancy with urgent histological examination during surgery, resection of the esophagus is indicated. Resection of the esophagus for benign non-epithelial tumors is performed extremely rarely - with a very large tumor that cannot be removed endoscopically and when malignancy cannot be rejected.
Discussion on the forum
Liver hemangioma
According to various sources, 0.5–20% of people have hemangiomas in the liver; women are approximately 4–6 times more likely than men. Most often, such neoplasms are not dangerous and do not even cause symptoms; they are discovered by chance during an examination for another reason.
Typically, symptoms occur with hemangiomas of the liver, reaching a size of 4–10 cm. Pain under the right rib, nausea, vomiting, the patient quickly eats. Most patients are recommended to undergo dynamic observation with periodic monitoring of the size of the hemangioma. Indications for surgical treatment occur rarely in the following cases:
- severe symptoms;
- rapid growth of the tumor;
- if there is doubt about the diagnosis, suspicion of a malignant tumor;
- spontaneous rupture of liver hemangioma and other complications.
There are minimally invasive treatment methods, such as hepatic artery embolization, radiofrequency and microwave ablation of the tumor, and radiation therapy. In more serious cases, it is necessary to perform enucleation of the tumor or resection (removal of the affected part) of the liver, in very rare cases - liver transplantation (if it is impossible to remove the hemangioma, it is huge and causes serious complications).