Ligation of the esophageal veins is a minimally invasive endoscopic procedure, which is an important component of the complex treatment of portal hypertension - increased pressure in the portal vein, through which blood flows from the intestines to the liver. Ligation of the esophageal veins helps prevent bleeding, which can be fatal for the patient.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
Dilatation of the veins of the esophagus. ICD I85.0 (I85.9)
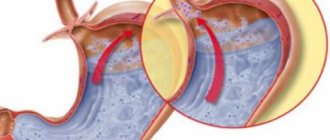
The walls of the esophageal veins are thin and easily stretchable, so an increase in pressure in them quickly leads to dilatation, deformation and bag-like bulging of part of the vessel. This is also facilitated by the fact that the veins of the esophagus are surrounded by loose, pliable connective tissue.
The anatomy of the venous system of the esophagus is quite complex. Blood from this organ flows to the three most important veins of the body. Impairment of blood flow in any of them can cause the appearance of phlebectasis in the esophagus. Most often, phlebectasis occurs in the lower parts of the tubular organ, as a result of disturbances in the v. system. portae (portal vein).
Various liver diseases (hepatitis, thrombosis, sclerosis, cirrhosis) lead to blood flow slowing down and pressure in the vein increasing (portal hypertension). The outflow of venous blood from internal organs, including the esophagus, slows down sharply, resulting in stagnation in the venous system.
The venous vessels of the esophagus, not adapted to such a volume of blood and pressure, stretch, their walls become thinner, the lumen of the veins becomes uneven, the veins lose their elasticity and bulge in a bag-like manner. Varicose nodes appear. The mucous membrane of the esophagus above the affected vessels becomes thinner and inflamed. All this creates conditions for damage to the integrity of the venous wall and the occurrence of bleeding - the most dangerous complication of varicose veins, threatening the life of the patient.
Complications and prognosis
The most severe and dangerous complication that pathology of the esophageal veins can lead to is bleeding. It leads to rapid and massive blood loss, hemorrhagic shock and, ultimately, death. In this case, even the presence of nearby medical workers and special equipment cannot always save the patient’s life.
According to statistical data, in patients who have suffered hemorrhage due to varicose veins, in 75% of cases a relapse occurs within a short period of time (1-2 years).
About 50% of patients die from blood loss. Moreover. the prognosis for life is extremely unfavorable: even if a person manages to control the veins of the esophageal gastrointestinal tract, complications from the liver may occur.
VRVP classification
All phlebectasias of the esophagus are divided into congenital and acquired.
- Congenital phlebectasis of the esophagus is a rare pathology, accompanied by many other severe abnormalities. The disease is associated with genetic predisposition and disorders that occur during pregnancy at the time of organ formation.
- Acquired are the result of impaired blood flow in large veins and, as a consequence, phlebectasis in the veins of the esophagus. Esophageal varices are common in liver cirrhosis.
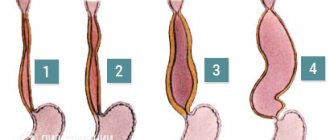
Depending on the size of varicose veins (varicose nodes) and the severity of the disease, four degrees of varicose veins are distinguished.
| Degree of disease development | Condition of veins and location of phlebectasias | X-ray characteristics | Condition of the esophagus | Clinical manifestations of pathology |
| 1st degree | Single dilated veins | Not defined | Satisfactory | Doesn't appear |
| 2nd degree | The veins of the esophagus dilate, become tortuous, and moderately enlarged varicose nodes appear. | An unclear venous contour is revealed. You can often see areas of stretched or tortuous veins. | The esophageal mucosa is not changed, its integrity is not compromised. | The clinic is not specific. Some patients experience discomfort when swallowing food. |
| 3rd degree | The lumen of the vessel narrows, the veins take on a serpentine shape, and the first angioectasia (dilation) appears. | In the middle of the esophagus and above, bulging vessels are detected. Distinct protrusion of venous nodes into the esophageal cavity. | The mucous membrane is thinned, erosions and foci of inflammation are detected on it. The mucous membrane is easily injured. | Belching and pain in the epigastrium and retrosternal space appear. Signs of micro- and sometimes macro-hemorrhage appear. |
| 4th degree | Veins are twisted, collected in nodes with numerous angioectasia | The esophagus is narrowed. Polypoid and cluster-shaped phlebectasias are identified. | The esophageal mucosa is thinned, with many erosions and inflammatory foci. | The patient has a clinical picture of severe esophagitis. A characteristic salty taste of blood appears in the mouth. The development of massive bleeding is very likely. |
Symptoms of the disease
At the first stage of the disease there is no pronounced discomfort; it is usually attributed to a violation of the diet and its errors, or to the symptoms of a gastrointestinal disease.
Heartburn appears, a mild indigestion, for which people often do not consult a doctor. When the disease progresses to the second stage, symptoms appear : belching, heartburn. Difficulty swallowing. Enlarged abdomen - ascites, accumulation of fluid in the abdominal cavity. Heaviness and burning in the chest
Complications of the disease are accompanied by: impaired swallowing reflex, bleeding, vomiting with blood, dark feces. In this case, urgent assistance is needed. Symptoms are different for everyone; diagnostics, a thorough medical history, and collection of all necessary tests are required.
Survey
Pathanatomy offers the study of micropreparations, tissue sections, and their laboratory study to identify the pathogen. The macroscopic specimen shows how the vessels are damaged and the esophageal mucosa is changed; specialists need this data to perform operations.
If a disease is suspected, the patient is prescribed tests and medical procedures. In differential diagnosis, other diseases that give similar symptoms are excluded. Qualitative research contributes to successful diagnosis. They include:
- General blood analysis . Shows the number of leukocytes and platelets in the blood
- Blood chemistry . Cholesterol content, liver enzymes, bilirubin level, protein amount, blood type and Rh.
- Endoscopy . The most detailed and reliable diagnosis is fibroesophagoscopy. Internal examination of the walls of the esophagus using an endoscope. The procedure allows you to find out the condition of the veins, the esophageal mucosa, the cause of bleeding, and identifies signs of other diseases with similar symptoms: cancer, ulcers.
- X-ray . Contrast radiography is used. To do this, the patient uses a radiopaque agent barium sulfate internally. When filling the esophagus, barium has a white light in the image and clearly highlights all the structures of the esophagus. Damaged vessels are clearly visible, in the form of oval filling defects.
- Duplex scanning of blood vessels . This is a dual ultrasound examination consisting of B-mode and Doppler. In modern medicine, the method of color Doppler mapping has appeared. The color determines the direction and intensity of blood flow. The use of these two methods allows you to examine the anatomy of blood vessels and veins, find out the degree of their expansion, see the presence of nodes and ectasia
Causes of VRVP
The cause of VRVP is congestion in the esophageal veins and increased pressure in them. The main factor for this is disruption of blood flow and increased pressure in one of the three main veins.
Pathologies most often occur in the v. system. portae. This is due to the fact that almost any disturbance of blood flow in the system of this vein leads to portal hypertension. Moreover, an obstacle to blood flow can occur in any area v. portae:
- the lower ones are thrombosis of the splenic vein, congenital narrowing of the portal vein;
- hepatic – liver cirrhosis, active hepatitis, hepatocellular carcinoma, schistosomiasis;
- upper – constrictive pericarditis, right ventricular failure.
With portal hypertension at the initial stages of development of varicose veins, phlebectasias are localized in the distal part of the organ, and only as the disease progresses, the veins of the stomach and the veins of the middle part of the esophagus are involved in the process.
VRVP can form when compressed by the superior vena cava (hypertrophied organ, enlarged lymph nodes, tumor). In this case, varicose veins of the esophagus will develop in the upper part of the organ.
In rare cases, VRVP occurs as a result of disturbances in the entire circulatory system (severe degrees of heart failure). In this case, blood circulation in all organs is disrupted. As a result of a violation of the outflow of blood from the esophagus, deformation of the veins is observed along the entire length of the organ, although the size of the nodes will be significantly smaller than with portal hypertension.
Dilated veins of the esophagus: symptoms
For a long time, the pathology does not manifest itself in any way. The first symptom of varicose veins is often bleeding. Sometimes hemorrhagic manifestations are preceded by unpleasant sensations in the retrosternal region (behind the sternum). More often, symptoms of esophagitis appear within a few days (sour belching, heartburn, difficulty swallowing solid food).
More often, hemorrhage is immediately preceded by overeating and sudden physical exertion. Although sometimes bleeding occurs during sleep.
The severity of hemorrhagic syndrome can be very different, from minor bleeding to massive blood loss that threatens the patient’s life. But even minor, constant bleeding can lead to serious consequences. Patients are constantly worried about:
- weakness;
- nausea;
- vomiting streaked with blood;
- melena.
The result of this is exhaustion, sudden weight loss, and iron deficiency anemia.
With massive blood loss, when blood flows out in a stream from damaged vessels, the condition immediately becomes critical, with rapidly increasing symptoms:
- suddenly the patient feels severe weakness, accompanied by a faint or faint state;
- severe sweating;
- nausea followed by vomiting large amounts of blood with clots;
- Blood pressure drops sharply, tachycardia appears, often accompanied by various kinds of arrhythmias, and the patient loses consciousness.
Signs of varicose veins of the esophagus
Grade 1 esophageal varicose veins, which can develop over years, do not have obvious symptoms. Sometimes the patient may feel heartburn, heaviness in the chest, and belching. Periodically, the patient complains of discomfort when swallowing food. Sometimes VRVP is accompanied by a venous pattern on the anterior wall of the abdominal cavity.
Reference! The first symptoms, as a rule, appear several days before the onset of bleeding. It consists of significant heaviness in the chest area and a deterioration in the general condition of the patient. Ascites is sometimes observed.
Immediately after a vein rupture, the patient experiences the following symptoms of esophageal varicose veins:
- A sharp decrease in blood pressure.
- Vomiting with blood.
- Bloody stool.
- Tachycardia.
- Light bleeding is accompanied by weakness and symptoms of anemia.
Diagnostics
Diagnostic measures are aimed at identifying the cause that caused varicose veins, as well as determining the stage of varicose veins, which determines the treatment strategy for the patient.
Mandatory diagnostic measures.
Laboratory research:
- study of peripheral blood (hemoglobin, red blood cells, hematocrit);
- study of venous blood (blood sugar, bilirubin and its fractions, AST and ALT, amylase, creatinine, total protein);
- coagulogram.
- Ultrasound examination of the liver
- X-ray examination with contrast of the esophagus (allows you to determine the nature of the dilation of veins and varicose nodes).
- fibroesophagoscopy (the main diagnostic method that allows you to determine how much the veins are changed, the presence of damage and hemorrhages, the condition of the venous nodes).
Treatment
If a diagnosis of varicose veins is established, then, depending on the degree of phlebectasis in the organ, appropriate treatment is immediately prescribed.
Basic principles of management of patients with esophageal varicose veins:
- treatment of the disease that caused varicose veins;
- delay the progression of varicose veins as long as possible;
- slow down the occurrence of hemorrhagic complications as much as possible;
- quickly stop the bleeding that has begun and rehabilitate the victim as fully as possible;
- use all means to prevent the recurrence of hemorrhages.
Varicose veins of the esophagus I degree
There are no clinical manifestations suggesting esophageal varicose veins at this stage of the disease. The veins are slightly dilated, their lumen is free. Nodes are just beginning to form, there may be 1-2 of them. The only method to detect the disease at this stage is esophagoscopy.
At this stage, the main method is conservative treatment, the patient is supervised by a gastroenterologist, therapy is mainly aimed at treating the disease that caused varicose veins. In addition, the patient is prescribed:
- diet therapy with strict adherence to the diet;
- develop a work and rest regime with the exception of heavy physical activity;
- warn about the need to eliminate bad habits;
- prevention of esophagitis: antacids (Gaviscon, phosphalugel), PPIs (omeprazole, rabeprazole), IGRs (famotidine, nizatidine), prokinetics (domeperidol, itopride).
Esophageal varicose veins, grade 2
In the second degree of pathology, the veins are dilated and tortuous, but their lumen is free. The mucous membrane is slightly changed or completely intact (not affected). At this stage, the disease can be detected not only by endoscopy, but also by contrast radiography of the esophagus. Clinical manifestations are determined mainly by the clinical picture of esophagitis:
- belching with a bitter or sour aftertaste, heartburn;
- discomfort in the retrosternal area;
- symptoms of dysphagia to varying degrees.
There are no bleedings with stage 2 VRVP.
A patient at this stage of the disease is usually prescribed:
- drugs that increase the pH of gastric juice;
- hemostatic drugs;
- vitamin complexes containing rutin and tocopherol to strengthen the vascular wall;
- iron-containing and vasoconstrictor drugs.
Grade 3 varicose veins of the esophagus
At this stage of phlebectasis, the veins are changed, serpentine in shape, their lumen is narrowed, the tone of the walls of the venous vessels is reduced, multiple nodes are clearly visible, and angioectasias are detected. The mucous membrane is changed, its integrity is damaged, multiple foci of inflammation and erosion appear on the surface. Gastroesophageal reflux is pronounced. With grade 3 VRVP, the risk of bleeding is very high. Hemorrhage can be caused by a variety of reasons:
- lifting weights;
- straining;
- feverish conditions;
- sudden rise in blood pressure.
The main goal of drug treatment is to prevent bleeding by:
- drug therapy for reflux esophagitis (diet, antacids, PPIs, IGRs, vitamins);
- transfusions of plasma, red blood cells, blood;
- administration of vasoconstrictor drugs.
If bleeding begins, it is necessary to stop it as soon as possible and carry out restorative therapy:
- tamponade of bleeding esophageal veins using a double-balloon Blackmore probe is a temporary measure, more often used in case of massive bleeding; inflated balloons press against the bleeding vessel, as a result the bleeding stops;
- ligation of varicose veins of the esophagus is ligation of bleeding veins (sometimes electrocoagulation of bleeding vessels is performed);
- restoration of blood volume, patients are immediately prescribed a transfusion of blood substitutes, and, if necessary, blood;
- measures are taken to prevent infection of the damaged mucosa and blood vessels.
After the bleeding has stopped and hemodynamic parameters have become stable, surgical treatment is prescribed to prevent relapses.
There are many methods of surgical treatment of varicose veins of the esophagus:
- anastomosis to reduce pressure in the affected vessel;
- prosthetics of venous vessels;
- suturing and removal of affected veins of the esophagus.
The method of surgical treatment and the extent of the operation are individually selected for each patient.
Stopping massive bleeding, and even more so preventing recurrent bleeding, is a very difficult task. Everything becomes more complicated if the cause of varicose veins is cirrhosis of the liver, a severe, constantly progressive disease. It is impossible to stop its progression with the current level of medical knowledge, which means it is impossible to reduce the level of constantly progressing portal hypertension. Even such a radical method as a liver transplant does not always lead to the desired results. And with the progression of portal hypertension, varicose veins progress, which is why patients with cirrhosis of the liver often die from bleeding from the esophagus.
Drug therapy
Drug therapy for varicose veins of the esophagus is primarily aimed at strengthening the vessels and reducing the load on them. The patient may be prescribed drugs to eliminate acidity in the stomach, vitamin complexes and drugs to treat the underlying disease. It is very important to monitor your blood pressure, as sudden increases can cause serious bleeding. The list of medications for each patient is compiled individually, taking into account the severity of the disease, the presence of concomitant diseases and the patient’s age.
Prognosis of VRVP in liver cirrhosis
The prognosis for VRVP is very serious, however, if the disease is detected in the early stages (stage I, and in some cases stage II), then it becomes possible not only to prolong the patient’s life, but, provided the patient follows all medical recommendations and proper treatment, for a long time maintain ability to work. In cases where the pathology is detected at stages III-IV, the prognosis is disappointing, especially in cases where hemorrhagic complications have begun. The main reason for this is that the diseases that cause varicose veins of the esophagus, especially liver pathology, are currently poorly treated, which means that varicose veins of the esophagus will progress all the time.
Useful tips
If, after diagnosis, the doctor reveals a grade 1 pathology, then you can initially try to eliminate varicose veins with preventive measures. This will prevent bleeding. Nutrition, physical activity, normalization of the psycho-emotional state - all measures are taken comprehensively.
The best option is to undergo regular examinations, especially for diseases of the liver, heart and blood vessels. The following recommendations should be kept in mind by a person at risk of esophageal varices:
- do not overwork physically beyond measure;
- exclude unhealthy foods from the menu, eat according to the diet prescribed by your doctor;
- take medications that constrict blood vessels.
It is recommended to divide the daily amount of food into 4-6 approaches and eat small portions. 3 hours before bedtime you need to finish snacking. Very hot food can damage the esophagus, so you need to choose dishes at a comfortable temperature. It is advisable that the cooking method excludes frying; steaming is preferable. Fatty and spicy foods should be excluded; you can learn about healthy foods and a therapeutic diet from another article in full detail.
Timely diagnosis of varicose veins will allow treatment to begin in the early stages, eliminate pathology and prevent serious complications.