What is pancreatitis
Pancreatitis is an acute or chronic inflammation of one of the main organs of the endocrine system of our body - the pancreas.
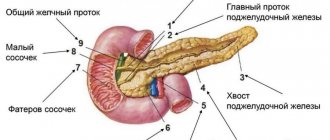
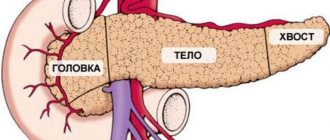
The functioning of the entire gastrointestinal tract and the process of food digestion depend on the normal functioning of this organ. The pancreas is located in close proximity to the liver, right behind the stomach. It performs many functions, the main one of which is the synthesis of hormones, in particular insulin. It also produces digestive enzymes that ensure the breakdown and absorption of fats, proteins and carbohydrates. Digestion of food occurs under the influence of pancreatic juice, which enters directly into the duodenum.
Enzymes and pancreatic juice begin to be produced immediately after any food or drink enters the stomach. Enzymes perform different tasks:
- lipase - breaks down fats;
- lactase, amylase, maltase and invertase convert carbohydrates into monosaccharides - glucose, galactose and fructose;
- trypsin - ensures the body's absorption of proteins.
In essence, pancreatitis is self-poisoning of pancreatic tissue by the enzymes it produces. Inflammation begins with excessive production of certain enzymes in combination with increased pressure in the ducts of the gland. Excess enzymes enter the general bloodstream, negatively affecting the functioning of the brain, kidneys and other internal organs.
Causes of inflammation of the pancreas:
- Alcohol abuse. More than half of the observations (p. 36-47) of pancreatitis are associated with regular consumption of large doses of alcohol.
- Pancreatitis often develops with cholelithiasis, abdominal trauma, the formation of cysts in the bile ducts, and malignant tumors in the gland.
- The disease can be a side effect of taking certain medications, such as diuretics.
The risk group includes diabetics, people with other endocrine pathologies and hepatitis B or C. Sometimes pancreatitis develops during pregnancy or after a kidney transplant.
How does alcohol affect the functioning of the pancreas?
Alcohol breaks down in the body to form acetaldehydes, which are toxic to humans. Pancreatic cells are especially susceptible to their harmful effects. In addition, drinking alcohol can cause spasms and narrowing of the pancreatic ducts, which leads to the accumulation of pancreatic juice in it. As a result, digestive enzymes begin to process the gland itself, causing inflammation. Over time, if the disease is not treated, the cells of the gland die (pancreatic necrosis) and are replaced by scar tissue, the organ loses the ability to function as before.
It is important to understand that the type of drink and its quality do not matter in this case. If a drink contains alcohol, it is harmful. Drinking alcohol together with fatty foods or foods with a high glycemic index can have a particularly negative effect on the functioning of the pancreas, since these products create additional stress on the organ.
Reasons for the development of pancreatitis
The disease develops due to damage to pancreatic tissue. This happens for the following reasons:
- alcohol and tobacco abuse
- abdominal trauma, surgery
- uncontrolled and long-term use of medications: antibiotics, hormonal drugs, corticosteroids, some diuretics
- intoxication with food products, chemicals
- genetic predisposition
- improper diet with a predominance of spicy and fatty foods and long breaks between meals
Types of pancreatitis
The most general classification of pancreatitis is based on the nature of the disease: acute attack or prolonged chronic pancreatitis with periodic relapses. The two forms differ in the severity of symptoms and require different treatment approaches.
Acute pancreatitis
The inflammatory process in acute pancreatitis develops very quickly and is always accompanied by severe pain. In most cases, the disease occurs due to alcohol abuse or after eating large amounts of fatty foods. Sometimes an exacerbation is preceded by an attack of acute hepatic colic.
Symptoms of acute pancreatitis:
- Severe pain in the left hypochondrium, radiating to other organs. The painful attack lasts about half an hour to an hour. The pain is felt especially strongly when lying on your back. The attack intensifies after eating food, especially fried and spicy food, and any alcoholic beverages.
- Vomiting, often uncontrollable with an admixture of bile and a bitter taste. Constant nausea that does not go away after vomiting.
- Low-grade or high fever.
- Sometimes, due to a violation of the outflow of bile, yellowing of the eye whites is observed, very rarely - a yellow tint to the skin.
- In some cases, the pain syndrome is accompanied by heartburn and bloating.
An attack of acute pancreatitis requires immediate medical attention. Painkillers provide only temporary relief, but do not affect the cause of inflammation. In the absence of qualified assistance, the risk of severe complications quickly increases: infection in inflamed tissue, necrosis and abscesses.
Severe acute pancreatitis can lead to shock and multiple organ failure.
Chronic pancreatitis
If, after an attack of acute pancreatitis, a person does not follow doctors’ recommendations and continues to drink alcohol and eat poorly, the disease is highly likely to enter the chronic stage. Chronic pancreatitis develops when there is significant damage to the pancreas during the first episode of the disease.
The disease is characterized by gradual pathological changes in the structure of pancreatic cells. Over time, it begins to lose its main function - the production of enzymes necessary for digesting food. Exocrine insufficiency manifests itself:
- diarrhea,
- bloating,
- a change in the nature of feces - they acquire a sticky consistency due to the large amount of fat in them and are poorly washed off the walls of the toilet.
Chronic pancreatitis can be asymptomatic for a long time: acute pain appears when significant pathological changes have already occurred in the pancreas. During an attack, chronic pancreatitis manifests itself with the same symptoms as acute:
- severe girdle pain,
- nausea,
- vomit,
- disturbances in intestinal function.
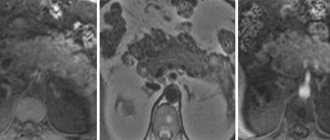
The diagnosis is made on the basis of ultrasound, computed tomography or magnetic resonance imaging. The examination usually reveals narrowed pancreatic ducts due to the formation of stones in them - calcifications. Hardware techniques also make it possible to detect cysts in place of atrophied tissue. Laboratory blood tests for chronic pancreatitis are not very informative.
Pancreatic insufficiency is determined by analyzing stool. If they contain a specific enzyme, pancreatic elastase, a diagnosis of chronic pancreatitis is made.
Pancreatitis - classification of the disease
Now let's talk about what pancreatitis is, symptoms and treatment in adult men and women. But first, let’s figure out why the pancreas is so important for the smooth functioning of the body.
There is an organ in the human body called the pancreas. The pancreas is located at the bottom of the stomach, communicating with the duodenum.
The organ is of great importance for the functioning of the entire human biosystem, as it performs a number of important functions:
- exocrine: synthesis of digestive juice, which contains many enzymes and promotes digestion;
- intrasecretory: synthesis of a number of hormones that affect carbohydrate, fat and protein metabolism.
For example, the pancreas produces hormones such as glucagon and insulin, which regulate blood sugar levels. When this system is destabilized, a person may develop diabetes.
You should not use folk remedies to treat pancreatitis.
With pancreatitis, inflammation of the pancreas occurs. The activity of the organ is disrupted, which leads to many other disorders. Pancreatitis happens:
- Acute
. Active inflammation, in which a sick man constantly suffers from vivid symptoms of pancreatitis. - Chronic
(most often a consequence of acute pancreatitis). In the chronic form, inflammation “sleeps.” The pancreas works, but with malfunctions. Chronic pancreatitis is characterized by a wave-like course with periods of rest and exacerbation.
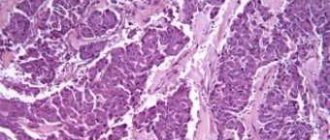
Chronic pancreatitis is more dangerous because it is characterized by constant progression of the pathological process. With this form of the disease, irreversible structural and functional damage to the gland occurs, which is why it is gradually destroyed.
Causes of inflammation of the pancreas
Pancreatitis is a multifactorial disease. The main reasons for the development are as follows:
- excessive and frequent consumption of alcohol;
- systematic smoking;
- intoxication;
- abdominal trauma;
- viral, fungal or infectious disease;
- disease caused by parasites;
- obstruction of patency in the pancreatic ducts.
Inflammation of the pancreas often develops as a postoperative complication or complication of cholelithiasis. There is also a hereditary predisposition to pancreatitis.
Importance of enzymes in digestion
The functioning of the human body is ensured by a complex system of interconnected and interdependent biochemical reactions. Thanks to special protein compounds - enzymes or enzymes - all these reactions are accelerated, ensuring rapid metabolism. The action of enzymes is very selective: each of them is capable of initiating, accelerating or slowing down only one reaction.
The digestive process is based on the work of digestive enzymes. Their main task is to make the process of energy absorption fast and efficient. Enzymes break down food components (proteins, fats and carbohydrates) into substances suitable for absorption. Moreover, the amount of enzymes produced depends on the quantity and quality of what is eaten.
Digestion of food begins in the oral cavity. The food, crushed into small pieces by the teeth, is mixed with saliva, which contains the enzyme alpha-amylase. The better we chew food, the easier it is for the enzyme in the salivary glands to convert starch molecules into soluble sugars and facilitate further processing.
After initial processing, food enters the stomach through the esophagus, where the gastric enzyme pepsin and hydrochloric acid begin to work. These substances create gastric juice, which:
- provides antibacterial protection for the body;
- stimulates the production of pancreatic hormones;
- regulates gastric motility;
- breaks down fats and performs a number of other functions.
In addition to pepsin, which is responsible for the breakdown of large protein molecules, other enzymes are produced in the stomach, for example:
- gelatinase is a solvent for collagen, gelatin and other connective tissue proteins;
- lipase is an enzyme that breaks down some fat molecules into fatty acids and monoglycerides;
- chymosin - starts the process of digesting milk protein.
Bile plays a significant role in the digestion process. It contains bile acids that stimulate the production of pancreatic secretions.
From the stomach, the food bolus is evacuated into the duodenum, where the main process of food digestion occurs. It is provided by more than 20 pancreatic enzymes. Enzymes are contained in pancreatic juice, which is produced by the gland in a volume of about two liters per day.
Functions of pancreatic enzymes:
- proteases - breakdown of proteins into amino acids;
- nucleases - act on DNA nucleic acids;
- amylase - breaks down starch into simple sugars;
- lipases - break down fats into higher fatty acids and glycerol.
The digestion process is completed under the action of enzymes of the small intestine and beneficial bacteria living in the intestines. The intestines absorb processed food into the body (Fig. 1).
Figure 1. Some important digestive enzymes. Source: Jason Northwest
When the function of enzyme production by the organs of the digestive system, especially the pancreas, is disrupted, the entire body becomes unbalanced. Such an imbalance entails nausea, diarrhea, flatulence, followed by anemia and exhaustion.
What to take with meals if you have a deficiency of pancreatic enzymes
With pancreatitis, the process of production of digestive enzymes by the pancreas is disrupted, as a result of which a person suffers from discomfort and pain in the stomach. In this case, after a complete examination, replacement therapy may be prescribed.
The goal of treatment with enzyme preparations is to compensate for their deficiency in the body, while reducing the load on the damaged organ. In some cases, such therapy is prescribed for life.
Important! The effect of all enzyme preparations begins 20-30 minutes after eating, so you need to drink them strictly before meals in the dosage prescribed by your doctor!
Modern pharmacology offers a large number of different enzyme preparations of animal and plant origin. Some of them are aimed only at replenishing the deficiency of a single enzyme, for example, one that breaks down lactose or fats. There are also complex agents prescribed for the deficiency of several enzymes in various organs of the digestive system.
Pancreatic enzymes are obtained from the organs of cows or pigs. The composition of the medicines includes the main pancreatic enzymes - amylase, lipase and trypsin. Polyenzyme preparations, in addition to pure pancreatin, may include bile acids, adsorbents or other enzymes. All drugs are selected strictly individually, taking into account the nature of the disease and the severity of symptoms.
Why do you need a diet for pancreatitis?
In the treatment of pancreatitis, nutrition plays no less a role than medications. The main goal of the prescribed diet is to restore the functions of the pancreas and normalize the production of digestive enzymes.
Products that are difficult to process increase the load on the inflamed organ. After a rich feast with fatty fried foods, the pancreas begins to intensively produce enzymes for its digestion. If the ducts of the gland are narrowed, pancreatic juice produced in extreme mode accumulates in the gland, aggravating the development of the disease - the affected pancreas begins to digest itself.
Signals that the gland is working overtime include:
- heaviness in the stomach after eating,
- heartburn,
- burping,
- attacks of pain in the stomach.
Of course, sticking to a strict diet all the time is not easy, especially at home. People with strict dietary restrictions are forced to cook for themselves separately and resist the temptation to eat anything fried or spicy.
It is important to understand that one violation of the diet can cause an acute attack of pancreatitis with all the ensuing consequences: severe pain, nausea, vomiting and diarrhea. A single failure can negate all efforts to maintain long-term remission.
What herbs can you drink?
To alleviate the condition, after consulting a doctor, you can drink decoctions of medicinal herbs.
Yelan
“Elan” is a ready-made collection of Altai herbs, sold in pharmacies. Has an anti-inflammatory effect. The decoction should be prepared according to the recommendations on the package.
Parsley
Parsley has a pronounced anti-inflammatory and antioxidant effect, stimulates gastric secretion. For chronic pancreatitis, an infusion of fresh chopped parsley is taken 2-3 times a day, half an hour before meals.
Herbal mixture No. 213
The collection includes a number of plants useful for inflammation: chamomile, wormwood, horsetail and other herbs. Decoctions based on the collection are prepared according to the recommendations on the packaging.
Surgery
Often, with chronic pancreatitis, patients develop stones that block the channels and ducts of the pancreas. They can worsen the condition of the organ or become a source of pain, so they are removed surgically.
When dilatation of the pancreatic duct is present, a bypass is performed from the organ to the small intestine. When there are structural changes in the gland or a large amount of inflamed mass, partial excision of the organ is performed.
Diet for pregnant women
Pregnant women often face problems related to the functioning of the gastrointestinal tract. Pancreatitis can develop due to abuse of vitamin complexes or due to excessive pressure on the pancreas from the uterus.
The principles of the diet for pregnant women do not differ from the general diet for pancreatitis. However, during pregnancy it is extremely important to provide a nutritious diet necessary for the development of the fetus. The following must be present in the food in sufficient quantities:
- proteins (lean meat and fish, dairy products, eggs, legumes),
- complex carbohydrates (cereals, pasta, fruits and vegetables),
- fats (vegetable oils),
- vitamins and minerals.