Causes of splenic rupture
The spleen is located inside the human body, that is, it is protected by the musculoskeletal frame from the influence of environmental factors. But by itself it does not have any particular strength, and it does not take extra effort to damage it. The internal “filling” of the spleen is the so-called pulp (translated as “pulp”), which is a delicate structure. Over its entire surface, the spleen is covered with a kind of connective tissue cover. If it weren’t for him, the spleen could easily be injured even with not too intense physical impacts on it - during falls during regular physical education, in ordinary situations at home and at work.
But even the presence of a protective case is not able to protect the spleen from damage. Under the influence of a traumatic factor, the pulp ruptures subcapsularly. This means that the connective tissue membrane remains intact, but the soft tissue of the spleen is damaged.
A rupture of the spleen is a violation of the integrity of its sections, which occurred due to a traumatic effect on the area of the abdomen in which the spleen is projected - the lower part of the chest on the left or the left hypochondrium. The most common causes of splenic rupture in patients who were brought to the clinic are :
a fall from a height, when the impact on the ground or other hard surface fell on the left hypochondrium and the left half of the abdomen;- various disasters - road, railway, industrial (impacts from bulky production equipment, mine collapses), natural (collapses as a result of an earthquake, impacts from tree trunks during hurricanes);
- deliberate infliction of physical injury (both with sharp and blunt objects; even clinical cases have been described in which a ruptured spleen was diagnosed after being punched in the side);
- sports injuries (a boxer's blow to the opponent's left hypochondrium, a fall on a gymnastic apparatus); Often, rupture of the spleen in such cases is observed in beginners who are trying to set some records, but in the absence of general sports training, they overestimated their capabilities and set the bar for achievements too high.
Causes
High-energy injuries are the immediate cause of splenic rupture. The organ is damaged by a fall, injury or blow to the stomach, as a result of a car, household or industrial accident. Injuries to the spleen can be professional or criminal in nature. In children, it is damaged during fights or outdoor games. The child falls or is hit in the left chest and abdomen.
Factors contributing to organ rupture:
- Thinned capsule, full-blooded and loose parenchyma,
- Immobility of the spleen
- Dysfunction of the hematopoietic system,
- Increased load on the spleen during prolonged and severe infectious processes,
- Excessive physical stress
- Difficult birth
- Colonoscopy and other invasive diagnostic and treatment procedures,
- Weakness of the abdominal muscles.
Diseases in which splenomegaly develops often lead to organ rupture. Non-traumatic causes of injury include:
- Infectious mononucleosis,
- Enlarged spleen of toxic, autoimmune or infectious origin,
- Hematological diseases,
- Oncological pathologies,
- Abscess of the spleen,
- Malarial infection
- Metabolic disorders
- Congenital anomalies of the spleen,
- Inflammation of nearby organs - liver, kidneys.
If a patient has the listed diseases, the lining of the spleen gradually becomes thinner, and sensitivity increases. The spleen can rupture regardless of a person's general well-being. The ideal functioning of internal organs minimizes the risk of such an event occurring. If the functioning of the bone marrow, endocrine glands and immune system is impaired, the likelihood of rupture increases significantly.
There is also spontaneous splenic rupture, which occurs for no apparent reason. This name is considered conditional, since in most cases, organ damage is preceded by minor trauma. In the presence of normal parenchyma, it does not lead to a violation of integrity. For spontaneous rupture of a pathologically altered spleen to occur, it is enough to make an awkward movement or sneeze.
Risk factors
Most often, splenic rupture occurs in working age people from 30 to 55 years. It is diagnosed more often in men than in women. Categories of people most often at risk of splenic rupture:
- persons whose work activity is associated with severe physical activity or extreme conditions;
- living in a socially unfavorable environment in which assault is often practiced to sort out relationships;
- dysfunctional families in which beatings are not avoided for educational purposes;
- families built on the principles of patriarchy and authoritarianism, as a result of which a woman often suffers assault from her husband.
Why can some people endure trauma to the abdomen without the risk of the spleen being damaged, while others with the same physical fitness, with similar anatomical features of the chest and abdominal wall, experience splenic rupture even with a non-critical mechanical impact? There are a number of factors that contribute to the rupture of the tissues of this organ:
fragility of the connective tissue capsule-case (congenital or due to diseases of the spleen);- plethora of the organ due to the fact that it deposited a large amount of blood;
- diseases of the spleen, due to which splenomegaly develops (increase in size), as a result of which the spleen is projected below the edge of its protector - the costal arch;
- looseness of spleen tissue due to hereditary factors or acquired diseases;
- low location of the organ immediately at the time of injury;
- breathing phase - during exhalation it is easier to injure the spleen, since due to the excursion (movement) of the ribs it is closer to the anterior abdominal wall;
- slight filling of the intestine at the time of injury, due to which its loops cease to be a life-saving shock-absorbing pillow in case of injury to the abdomen on the left.
Splenic ruptures can be:
- isolated, without damage to other internal organs;
- in combination with injury to one or more internal organs (so-called polytrauma).
In case of polytrauma, splenic rupture is most often accompanied by:
rib fractures;- injuries from the chest - in particular, pneumo- and hemothorax (respectively, air and blood in the pleural cavity, which normally are not there);
- liver damage;
- ruptures of the mesentery (a thin connective tissue film with which the intestines are attached from the inside to the abdominal wall);
- spinal fractures in the thoracic and lumbar spine.
Diagnostics
It is probably simply impossible to ignore the signs of a splenic rupture, since the person feels extremely severe, acute pain. But it can be very difficult to correctly determine the diagnosis due to symptoms that are also characteristic of other pathologies of internal organs. The presence of the alleged damage can only be definitively confirmed during surgery. In all other cases, it is possible to establish a specific diagnosis with a probability of about 12-15%.
If you suspect an organ rupture, you should definitely go to the doctor. At the clinic, you will be prescribed a set of examinations that will help identify the cause of the pain:
- Ultrasonography. On the monitor, the tear does not reflect ultrasonic waves, that is, it is not possible to see the edges and tissues of the organ. This occurs due to excessive bleeding. Indicators of splenic rupture on the ultrasound screen are considered to be the complete absence or decreased mobility of the diaphragm in the area of the left dome. In addition, in this condition, there is a pronounced displacement of the abdominal organs to the left. Sometimes an ultrasound becomes impossible due to severe pain when pressing on the damaged area.
- Laparoscopy. This is a surgical examination that makes it possible to identify the presence of injury, its size and location. Laparoscopy involves puncture of the abdominal cavity and internal insertion of a special telescopic tube. If such an examination is impossible due to certain contraindications, the doctor may prescribe the patient an identical surgical diagnostic method - laparocentesis. During this procedure, soft tissues are carefully pierced with a special device and the liquid accumulated inside is removed.
- X-ray of the chest and abdomen. Often, it is not possible to examine the damage in detail on a plain X-ray, so doctors often recommend a contrast examination of the network of blood vessels—antiography. This procedure can detect vascular damage caused by the injury and determine the extent of bleeding.
Classification of spleen injuries
According to the degree of damage to the fragments of the spleen, there are ruptures (according to the degree of increasing severity):
- contusion – when a small section of the spleen parenchyma is torn, the capsule (case) remains intact;
- rupture of the sheath with minor damage (at the level of micro-tears) to the spleen parenchyma;
- instantaneous rupture - the capsule case and the internal contents of the spleen rupture at the same time;
- two-stage rupture - first the more delicate parenchyma ruptures, macroscopically the capsule remains intact, but has microscopic damage of a linear nature, due to which after some time a visible (macroscopic) violation of the integrity of the capsule occurs;
- imaginary two-stage rupture - the parenchyma ruptures, but the blood clot blocks the source of bleeding, it stops, but after some time the clot is washed away, bleeding resumes;
- imaginary three-moment rupture - a two-moment rupture occurs, during which the bleeding stops, since the clot again tampons (blocks) its source, after which it is washed out again, the bleeding continues.
According to domestic statistics, most often simultaneous ruptures of the spleen occur, accompanied by heavy bleeding into the abdominal cavity and rapidly developing blood loss, which is life-threatening. The countdown from the moment of injury to the critical level of blood loss due to bleeding is 4-6 hours.
But there are also atypical cases when, with a small rupture of a section of the spleen, it closes with a huge blood clot, the bleeding stops and can resume as soon as 7-20 days later, when the clot is displaced. Reasons for renewed bleeding:
- cough;
- loud savory sneezing;
- coughing;
- awkward turning of the body (for example, uncontrollable sleep in bed);
- the act of defecation - especially with constipation, when the patient, in order to recover, strains, like a woman in childbirth;
and a number of other circumstances that provoke an increase in pressure in the spleen.
Causes of damage
Anyone can experience a ruptured spleen, regardless of age or lifestyle. This pathology may well overtake an elderly person, a teenager, and even a very young child.
The first symptom of splenic rupture in adults is the appearance of an extensive hematoma, which is filled with blood clots. This condition is called a subcapsular formation. Gradually the capsule opens, provoking the development of bleeding. The most common cause of splenic rupture is serious abdominal trauma. In this case, all symptoms usually appear immediately. According to statistics, rupture of the spleen from a blow occurs in approximately 70% of all cases of pathology.
Much less often, an organ is damaged due to other conditions:
- clonal deviations in the functioning of the hematopoietic system;
- the occurrence of infectious processes in the body that increase the load on the spleen;
- too much physical activity due to pathologies in the spleen;
- abnormal changes in the organ, for example, its pathological enlargement;
- increased level of blood filling during the formation and development of the fetus in the last trimester of pregnancy;
- disruptions in metabolic processes;
- injury to the capsule during contractions during rapid or complicated labor;
- malignant and benign neoplasms in organ cells;
- vector-borne infectious diseases, for example, malaria;
- inflammation of nearby structures, for example, cirrhosis of the liver, tuberculosis or hepatitis C.
Symptoms of a splenic rupture
Clinical manifestations of splenic injuries accompanied by ruptures are, on the one hand, varied, and on the other hand, quite characteristic . Therefore, making a diagnosis purely based on symptoms without using additional examination methods is not difficult . An aid to diagnosis is the collection of anamnesis (information from the patient about the development of the condition) - the traumatic factor (fall, fight) is clearly visible in the anamnesis.
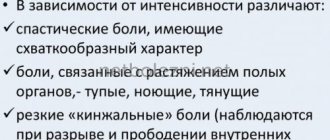
In the first hours after trauma to the spleen, a characteristic complaint is pain in the left upper part of the abdominal wall and in the lower part of the chest on the left (a symptom typical in the first hours after injury).
From the abdominal organs, after some time the following are observed:
- intestinal paresis (lack of peristalsis) – its internal contents “freeze” in place and do not move towards the anus, as happens normally;
- retention of gases, their accumulation in the intestines and because of this bloating (as surgeons say, “a mountain of a stomach”);
- inability to recover (although the final segment of the large intestine may be full).
must be observed:
- pronounced pallor;
- cold sweat, sticky in consistency;
- sharp deterioration in general condition;
- severe general weakness;
- drowsiness up to a state of prostration (lack of orientation in space, place and time);
- dizziness, accompanied by darkening of the eyes, sometimes with a subjective sensation of “sparks from the eyes”;
- in advanced cases with critical blood loss - twilight consciousness bordering on fainting;
- vomiting (even in the absence of any contents in the stomach);
- increased heart rate and decreased blood pressure;
- dyspnea;
- tinnitus, sometimes with variations - clicking, slight ringing.
With critical blood loss, general weakness and lethargy gives way to excitement, which at any moment can give way to fainting.
Signs of blood loss are valuable for diagnosis, since they make it clear that there has been a “leakage” of blood, that is, significant damage to the organ. But, on the other hand, they are nonspecific, since they can develop with any catastrophe in the abdomen, and not just with a rupture of the spleen.
Splenic rupture: what is it?
Tinnitus, dizziness, shortness of breath are some of the symptoms of a ruptured spleen, in which you should immediately seek medical help.
This injury is quite common in falls from great heights, road accidents, natural, industrial and railway accidents. A splenic rupture can provoke the development of internal bleeding. To prevent the development of this complication, it is necessary to perform the operation as soon as possible.
Damage to the spleen is most often observed in able-bodied middle-aged people, which is caused by their higher physical activity compared to children and the elderly. According to statistics, able-bodied people are more likely to find themselves in extreme situations, risking a similar injury.
Depending on the number of organs affected, such damage may be:
- Isolated, when only the spleen is affected.
- Multiple, when damage to several organs has occurred.
In most cases, the mesentery, liver and colon are damaged simultaneously with the spleen. Fractures of the ribs and spine, injuries to the chest, fractures of the bones and pelvis, and traumatic brain injuries are also possible. The elimination of such pathologies is carried out by abdominal surgeons and traumatologists.
The spleen is a parenchymal organ that is located in the left side of the abdominal cavity, behind the stomach. This organ is not one of the vital organs, although it performs a number of important functions. This is the main source of lymphocytes, producing antibodies and destroying old red blood cells and platelets. The spleen also functions as a blood depot.
Symptoms
Symptoms of a ruptured spleen can be very extensive. The manifestations in this case depend on how serious the damage is and how long ago it occurred.
If relatively little time has passed after the injury, then the following symptoms are possible when the spleen ruptures:
- the patient's condition gradually worsens, there are signs of acute blood loss;
- severe pain in the area of the left hypochondrium and upper abdomen;
- the left shoulder and part of the shoulder blade are painful.
Victims most often lie on their left side or back, tucking their legs. This pose is forced. The abdominal wall does not take part in the breathing process.
Palpation allows you to identify pain of varying intensity in the patient. The abdominal wall is tense to one degree or another. If we are talking about a state of shock or collapse, then the patient’s abdominal muscles may be relaxed. With severe internal bleeding, percussion of the abdomen shows dullness of sound.
A few hours after the injury, the victim develops intestinal paresis. This condition is accompanied by bloating, gas retention and lack of bowel movements.
In addition to local symptoms, the patient may have signs of acute increasing blood loss. These include:
- pallor;
- decreased blood pressure;
- cold clammy sweat;
- rapid pulse;
- nausea and vomiting;
- severe weakness that progresses;
- tinnitus and shortness of breath;
- dizziness.
After some time, motor agitation may develop, after which the patient may lose consciousness. The pulse increases to 120 beats per minute, and blood pressure does not reach 70 mm.
Most of the above symptoms of spleen damage do not directly indicate spleen rupture. They are characteristic of most traumatic injuries of the abdominal organs. Clinical signs will not be enough to establish the exact cause of bleeding. This requires professional diagnosis.
Causes
A careless fall from a height is one of the most common causes of splenic rupture in children.
The main cause of splenic rupture is a sudden and strong mechanical impact. Most often this happens in accidents and work-related injuries.
Subcapsular rupture of the spleen can occur in both adults and children. In children, the causes of this pathology are the following factors:
- fights during which the child receives strong blows to the chest area;
- traffic accidents;
- falling from a great height.
Predisposing factors to the development of splenic rupture in an adult are:
- practicing various types of martial arts, including boxing;
- lack of normal development of abdominal muscles;
- splenomegaly;
- increased physical activity;
- organ plethora;
- extreme sports;
- rib damage;
- thin capsule of the spleen;
- too loose parenchymal tissue;
- the spleen has low mobility.
A ruptured spleen can be caused by a difficult birth. Less commonly, the organ is damaged by a large neoplasm, such as a cyst or tumor.
Risk factors
The likelihood of splenic rupture increases significantly if the following predisposing factors are present:
- the thin capsule of the organ is not strong enough;
- the spleen has low mobility;
- organ plethora.
This organ is reliably protected from injury by the ribs. However, with significant mechanical impact, injury may occur. The strength of the spleen depends on the following factors:
- the position of the victim at the time of physical impact;
- degree of blood supply to the organ;
- respiratory phase;
- filling the stomach and intestines.
In some patients, splenic rupture did not occur even with a fracture of the lower ribs. Naturally, such cases can be considered a happy coincidence, but the strength of the organ can indeed vary depending on the factors described above.
Clinical examination data for splenic rupture
Upon examination, the following signs will be characteristic:
about 80-85% of victims take a characteristic position - they lie on their left side, bending over and pulling their knees to their stomach;- the patient’s breathing is shallow (gentle), the anterior abdominal wall does not take part in the act of breathing (only diaphragmatic breathing is preserved);
- Tension of the anterior abdominal wall may not be observed - in the case when collapse has already developed (a sharp drop in blood pressure) or a state of shock due to blood loss. Abdominal muscle tension is not a 100% sign of splenic rupture.
When percussing (tapping with fingers) of the anterior abdominal wall, dullness (dullness) of sound is observed due to the accumulation of fluid (blood) in the sloping areas of the abdomen.
During auscultation (listening with a phonendoscope or stethoscope), bowel peristaltic sounds will be weakened. Breathing in the left half of the chest will also be weakened reflexively.
Diagnosis of splenic rupture
In most cases, the diagnosis of splenic rupture can be made based on clinical signs, without resorting to additional examination methods - a history of trauma (history of the development of the condition), pain in the left half of the abdomen and rapidly increasing signs of blood loss primarily allow one to suspect a splenic rupture.
Of the additional examination methods, abdominal radiography is informative.
The main radiological signs of splenic rupture are:
- uniform blurry shadow in the projection of the spleen;
- high location (standing) of the left dome of the diaphragm;
- displacement of the intestine down and to the right.
Of the modern diagnostic methods, laparoscopy provides almost 100% results in making the correct diagnosis - inserting a tube with an optical system into the abdominal cavity through a small hole, through which you can observe the processes in the abdomen without making a traditional and traumatic laparotomy (an incision in the anterior abdominal wall). If the clinic does not have a device for performing laparoscopy, then laparocentesis can help out - piercing the anterior abdominal wall with a special surgical instrument with a trocar and determining whether there is blood inside.
The MRI method will help assess the degree of blood loss by the presence of blood in the abdominal cavity.
A blood test may not be informative : blood counts in the first hours of acute blood loss remain unchanged due to compensatory mechanisms (the body understands that there is little blood transporting nutrients and air, and releases some of it from the depot).
Diagnosis
A splenic rupture is accompanied by intense pain that cannot be ignored. It is this that forces a person to see a doctor. The specialist takes into account not only the victim’s complaints, but the physical examination data, the results of measuring pulse and pressure. When examining a patient, doctors pay attention to the abdominal wall that is swollen and hard to the touch, to the presence of abrasions, hematomas and other signs of injury. However, making a diagnosis based on symptoms alone is quite difficult. Similar manifestations occur when other internal organs are affected.
At the initial stages, the diagnosis of pathology is carried out taking into account clinical symptoms, the results of radiography, laparoscopy and other methods.
splenic rupture, subphrenic hematomaOn the radiograph on the left, under the diaphragm, a uniform darkening is visualized, displacing the dilated stomach, kidney and part of the intestine to the right and down. In the absence of obvious symptoms, X-ray data are considered nonspecific - not allowing a diagnosis.
- Angiography is a radiopaque study that can detect vascular damage and determine the extent of bleeding. This method requires a lot of time, expensive equipment and specially trained personnel. It is used extremely rarely.
- Ultrasonography - assessment of the condition of the damaged organ, detection of free fluid in the abdominal cavity and immobility of the diaphragm, determination of the symptom of “floating loops” and decreased echogenicity of the spleen.
- Laparoscopy is a diagnostically significant, informative and widely used method for detecting damage. It allows you to confirm the suspected diagnosis and accurately determine the location of the source of bleeding. Specialists on the surgical table puncture the abdominal cavity and insert an endoscope inside. It is used to determine the presence of injury.
- Laparocentesis is performed in the absence of endoscopes or if the patient has contraindications to laparoscopy. This is an alternative technique that consists of piercing the anterior abdominal wall with a trocar, inserting a catheter through it and removing contents from the abdominal cavity. Laparocentesis confirms the presence of bleeding, but does not determine its source.
- Blood tests may initially give normal results. Their lack of information is due to the compensatory restoration of the composition of peripheral blood. Subsequently, signs of anemia, hypovolemia, and endotoxemia increase.
Detecting a splenic rupture is not at all easy. Diagnosis requires a thorough examination of the victim, study of the clinical picture, and correct interpretation of the results of hardware studies. Only during surgery can specialists confirm with 100% certainty that the spleen has ruptured.
Medical tactics for splenic rupture
The biggest danger when the spleen ruptures is bleeding, which leads to blood loss, and this, in turn, is life-threatening. Bleeding from a damaged spleen can stop on its own thanks to a blood clot that plugs the damaged area. But in the vast majority of cases, emergency surgery is indicated to stop the bleeding.
Due to the fact that the internal contents of the spleen are a spongy substance, it is extremely problematic to apply sutures to it in case of damage, to the point that it is simply impossible to apply them and tighten a full-fledged surgical knot - they cut through the tissue. Therefore, even with minor damage to the spleen, surgeons are forced to remove it. Direct indications for removal of this organ without attempts at suturing:
- extensive ruptures;
- ruptures in the area of the so-called gate (the place where the artery enters the organ and where the vein exits);
- through and torn damage.
A victim who is diagnosed with a capsule rupture with intact parenchyma is lucky: in this case, the damage is sutured without problems. But after the operation, careful observation is carried out, since after the rupture of the capsule, parenchymal rupture may occur after some time.
The sooner the surgery is performed, the sooner the bleeding is stopped, the less blood loss will be. To compensate for this, blood products and blood substitutes are transfused. Reinfusion is also practiced: blood that has spilled into the abdominal cavity from the damaged spleen is collected, filtered and immediately, during surgery, injected into the patient’s bloodstream.
Surgery
Surgery is necessary to stop internal bleeding, which can be fatal. Immediately before surgery, doctors normalize hemodynamics through transfusion of blood substitutes or blood.
If the victim is in critical condition, doctors perform an urgent operation to remove and sew together the organ, without stopping the transfusion.
Just a few decades ago, when the spleen ruptured and hemorrhaged, doctors resorted to one method of eliminating the pathology - complete removal of the affected organ.
Today, such an operation is prescribed exclusively in the following cases:
- inability to suture the wound;
- departure of the organ from the pedicle;
- cutting seams;
- ruptures and cracks directed towards the hilum of the spleen;
- through and torn knife and gunshot wounds.
In all other cases, there is simply no reason to completely remove the damaged organ, so it remains partially or even entirely.
Damaged spleen: to be or not to be?
Until recently, surgical tactics for splenic ruptures were reduced to removing this organ. But disputes continue among practical surgeons about whether it is advisable to carry out reconstructive (restoring integrity) operations on the spleen if it is damaged.
The importance of the spleen for the human body cannot be overestimated, knowing its role. She begins to work actively even in the early stages of fetal development - she inserts a significant 5 kopecks into hematopoiesis: until the 9th month of intrauterine development of the fetus, this is one of the organs of the holistic hematopoietic system of the future human being, which produces red blood cells and leukocytes.
Before the birth of a child, the spleen transfers the mission of hematopoiesis to the bone marrow, but joins the work of the immune system - it begins to produce lymphocytes and monocytes. However, it does not forget its hematopoietic role: in the case of certain blood diseases, foci of hematopoiesis appear in it again.
The functions of the spleen after the child is born and grows up are as follows:
the organ is the main “factory” for the production of circulating lymphocytes (cells that fight bacteria, protozoa and foreign objects that have entered the body), as well as antibodies (structures that prevent the proliferation of bacteria and viruses and the formation of protein poisons);- the spleen serves as a “graveyard” for some blood cells - old, unusable, diseased and damaged red blood cells and platelets; without such a function, outdated blood cells would have wandered around the body for a long time, confusing it (the cells are present, but do not bring any benefit);
- the organ takes part in the metabolism of iron and the production of bile - after the destruction of red blood cells and platelets in it, their remains are sent to the liver, where they are utilized. Thus, red blood cells and platelets, having completed their “blood” life, thanks to the spleen, begin to exist as part of the biliary system;
- The parenchyma of the spleen is capable of depositing (accumulating) blood, and also accumulates “for a rainy day” platelets (about a third of all platelets in the human body) and releases them in case of need (for example, in case of acute or chronic blood loss, destruction of diseased platelets).
Even a brief overview of the functions of the spleen makes it clear that it is necessary to reconsider surgical tactics in case of ruptures, which now boils down to removing this organ . It should be taken into account that the role of the spleen has not yet been fully studied. If scientists prove that it performs endocrine (hormone-forming) functions, in particular, performs hormonal regulation of the bone marrow, its importance for the human body will increase significantly. This means that medical practitioners will need to immediately think about the development of surgical methods that ensure the preservation of the spleen in case of damage.
Prognosis after spleen removal
Since the functions performed by the spleen are performed not only by it, after removal of this organ a person, thanks to correct and complete rehabilitation measures, can return to a normal lifestyle. But possible consequences:
- weakened immunity;
- changes in the blood;
- signs of dyspepsia (digestive disorders);
- the formation of large and small blood clots in the vessels of the liver;
- atelectasis of the lungs - collapse of some of their areas.
For the rest of his life, a person who has had his spleen removed must adhere to certain recommendations:
- beware of infectious diseases - to do this, get vaccinated in a timely manner during epidemics, avoid crowded places (queues, festive events, public transport), get vaccinated before traveling to exotic countries, carefully follow the rules of sanitation and hygiene;
- If you have a cold, do not self-medicate at home, but immediately consult a doctor;
- avoid countries where you can become infected with malaria;
- for the first two years, do a control ultrasound of the abdominal organs once a year, then, if there are no changes due to splenectomy, once every two years;
- Use all medications only as prescribed by a doctor or after consultation with him;
- engage in physical exercise (but not sports - the difference with physical exercise is the severity of physical activity); observe the correct regime of rest, work, nutrition, sex, quit smoking, do not use drugs, do not abuse alcohol (but reduce its use to a minimum) - that is , lead a healthy lifestyle.
If these simple rules are carefully followed, the patient with the spleen removed will not feel any changes in his general condition.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
15, total, today
( 195 votes, average: 4.58 out of 5)
Esophageal obstruction: causes, symptoms, treatment
Relaxation of the diaphragm, its relaxation: what is it?