The location of the pancreas is such that it is not very accessible for palpation, so diagnosing its diseases requires instrumental and laboratory research methods.
Of the instrumental methods, one of the fastest, most informative and safest, allowing one to determine the density and size of the pancreas in normal and pathological conditions, to detect inflammation, developmental abnormalities, tumors, the presence of stones, cysts, fistulas, is ultrasound examination (ultrasound).
Other methods either do not provide the necessary information or are less accessible, such as MRI. It is more accurate and visual, but is not available everywhere and is much more expensive than ultrasound.
Laboratory indicators are important for diagnosing pancreatic diseases - determination of enzymes in the blood and urine. Normally they shouldn't be there. Therefore, if their appearance is detected, the patient is almost always prescribed an ultrasound.
Pancreatic diseases
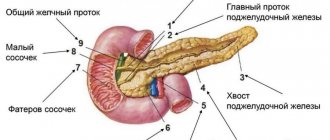
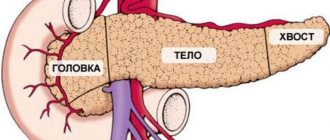
The pancreas is an organ of the digestive and endocrine system. The main functions are the production of pancreatic juice, which contains enzymes, and the production of several important hormones, including insulin. Located posterior to the stomach, closely connected with the duodenum. The pancreas consists of a head, body and tail; blood supply occurs through the pancreaticoduodenal arteries and veins. Most often diagnosed:
- Pancreatitis.
Magnetic resonance imaging for acute organ pathology
Acute inflammation of the pancreas is accompanied by severe pain in the upper abdomen. Other symptoms include nausea, vomiting, diarrhea, flatulence and fever. The cause of acute pancreatitis is gallstones, chronic alcohol consumption, hereditary diseases, injuries, medications, infections, electrolyte and hormonal disorders, high lipid levels, etc. If it is impossible to detect an internal factor, they speak of idiopathic (i.e., self-occurring) form. In the absence of adequate diagnosis and treatment, tissue necrosis occurs.
In acute pancreatitis, MRI shows the presence and degree of necrotization of the pancreas and the area of edema. Magnetic resonance imaging has advantages over CT in diagnosing subtle (initial) changes.
A standard MR scanning protocol of the pancreas, including T2WI, T1WI fat-suppressed and a series of T1WI, GRE sequences before and after gadolinium administration, is a reliable way to determine the stage of acute pancreatitis and the prognosis of the disease.
In severe acute pancreatitis, MRI of the pancreas with contrast is performed to assess parenchymal perfusion and the presence of necrosis. Organ enlargement is clearly visualized on any sequence, and parenchymal edema is better demonstrated on native T1 imaging.
MRI of the pancreas in chronic pancreatitis shows uneven expansion of the main duct with the formation of lateral branches, filling defects
Chronic pancreatitis is a progressive disease associated with the gradual destruction of the pancreas against the background of fibrosis and cellular infiltration, with the development of duct pathology and loss of exocrine and endocrine functions. Clinical manifestations are similar to the acute form. The advanced stage is characterized by underweight, anemia, and the development of type 2 diabetes. With a long-term ongoing process, MRI shows atrophy of the pancreas and pseudocysts. Changes are differentiated from tumor pathology.
- Pancreatic tumors.
Double duct sign on MRI indicates pancreatic cancer of the head of the organ
The majority of cases (85%) of malignant lesions are adenocarcinoma of ductal origin with typical localization in the head of the organ. Pancreatic cancer is difficult to detect at an early stage because there are no clinical manifestations. As the pathology progresses, abdominal pain, back pain, weakness, yellowing of the skin and sclera appear. Ultrasonography for tumors smaller than 3 cm shows ambiguous data. Multiparametric MRI with diffusion-weighted imaging and magnetic resonance cholangiopancreatography allow the analysis of morphological changes in the pancreatic parenchyma and duct.
- Cystic and pseudocystic neoplasms.
Multicystic lesion of the pancreas on MRI
Cysts and pseudocysts are detected during ultrasound scanning of the abdominal organs; often, when they are small in size, symptoms are nonspecific or absent. It is important to undergo an in-depth study to determine the malignant potential of the tumor. To make a diagnosis, gender, age, and medical history (trauma, alcohol intoxication, chronic diseases of the biliary system, etc.) are important. Final verification is possible after morphological examination.
Signs of cystic neoplasms of the pancreas:
- irregular contour, thickening of the walls;
- presence of partitions;
- visualization of solid components;
- dilated pancreatic duct more than 3 mm;
- calcifications, etc.
Exocrine pancreatic insufficiency: diagnostic possibilities and methods of correction
Pancreatic insufficiency can occur both with a general decrease in the production of all pancreatic enzymes, and with an isolated decrease in the production of one of them. Clinically, exocrine pancreatic insufficiency can manifest itself as diarrhea, flatulence, abdominal pain, nausea, repeated vomiting, decreased appetite, as well as such nonspecific symptoms as general weakness, decreased physical activity, weight loss, stunted growth (in severe forms of maldigestion). An important diagnostic sign of exocrine pancreatic insufficiency is a change in the nature of the stool, because manifestations of lipase deficiency develop before the decrease in amylase and protease activity. The stool becomes bulky, polyfecal matter is noted, the stool is grayish in color and has a “greasy” appearance, and steatorrhea appears. Diagnosis of pancreatic pathology is one of the most difficult problems of pediatric gastroenterology and is based on the analysis of the results of both laboratory and instrumental research methods. Determination of the content of pancreatic enzymes in the blood (a-amylase, lipase, trypsin and its inhibitor) makes it possible to judge the organic damage to the organ, the presence of damage to acinar cells, however, it reflects the exocrine function of the pancreas to a lesser extent. Normally, 60% of serum amylase is amylase from the salivary glands, the remaining 40% is from the pancreas [1]. An increase in the enzyme content in the blood serum is a fairly early marker of acute pancreatitis: an increase in amylase activity is observed within 2–12 hours from the onset of the disease. It should be noted that the sensitivity and specificity of this marker for pancreatitis in children is somewhat lower than in adults and amounts to no more than 80–90% [1], while up to 40% of pancreatitis in childhood can occur with normal serum amylase activity [2 ]. When assessing the results of a laboratory test, it should be remembered that hyperamylasemia is a nonspecific symptom and can be caused by another pathology: appendicitis, acute cholecystitis, diseases of the salivary glands, renal failure (due to decreased amylase clearance) (Table 2). For the differential diagnosis of hyperamylasemia, determination of the level of amylase isoenzymes can be used (Table 3). Serum lipase levels also tend to be elevated in acute pancreatitis and remain elevated longer than amylase levels. An increase in the activity of this enzyme in the blood is a more sensitive and specific marker of pancreatic damage, and when the level of both enzymes is simultaneously determined, the sensitivity of the method reaches 94% [3,4]. Important for the diagnosis of acute pancreatitis is the determination of the activity of other pancreatic enzymes in the blood serum, in particular elastase-1, trypsin and its inhibitor with the determination of the inhibitor/trypsin ratio, which decreases with organ pathology. Significant in the diagnosis of pancreatitis is the determination of the concentration in the blood and urine of phospholipase A2, a marker of the destructive process in the pancreas. According to N.B. Gubergrits (2001), the sensitivity of various pancreatic enzymes in the blood depends on the duration of the disease (Table 4) [5]. For the diagnosis of acute and exacerbation of chronic pancreatitis, determining the level of pancreatic enzymes in the urine is of great importance. In acute pancreatitis, the level of urine amylase (diastase) can be increased by 5–10 times. It should be recognized that scatological research has not lost its relevance to this day and is the most accessible method that can confirm the presence of exocrine pancreatic insufficiency; however, in contrast to determining the level of pancreatic enzymes in the blood, indicating direct damage to the organ, based on the results of scatology, carry out a differential diagnosing absolute and relative pancreatic insufficiency is reliably impossible. A stool examination should be performed before administering pancreatic enzymes. The accuracy of this method is also influenced by: the state of intestinal motility, the volume of bile secreted into the intestinal lumen, its qualitative composition, the presence of inflammatory processes in the intestines, etc. Analysis of the results of a scatological study allows us to identify the following symptoms: • steatorrhea - an increase in the content of neutral fat in the feces (steatorrhea type 1), fatty acids/soaps (type 2 steatorrhea) or a combination thereof (type 3 steatorrhea); • creativeorrhea – increased content of muscle fibers in the stool (++ or +++); • amilorrhea – the presence of starch grains in the stool. Persistent persistence of steatorrhea and creatorrhoea may most likely indicate the presence of exocrine pancreatic insufficiency in the patient, while amylorhea is detected in patients with pancreatic insufficiency quite rarely, since starch hydrolysis is often not impaired due to the high activity of intestinal amylase. A fecal lipidogram allows you to clarify the nature of steatorrhea and is of certain importance in assessing the effectiveness of enzyme therapy. The fat content in stool is assessed qualitatively (adding Sudan dye to the stool) or quantitatively. The latter is the most informative [6], allowing a total determination of the total amount of fat in feces, taking into account fat of exogenous (food) origin. Normally, the amount of fat excreted in feces should not exceed 10% of the fat introduced with food. In diseases of the pancreas, the amount of fat excreted in feces sometimes increases to 60% [7]. Determination of elastase-1 in feces allows one to assess the degree of exocrine pancreatic insufficiency and make a differential diagnosis between absolute and relative exocrine insufficiency. Elastase-1 is a proteolytic enzyme of the pancreas with a molecular weight of about 28 mDa. It is known that the enzyme does not change its structure as it passes through the gastrointestinal tract, which allows it to be considered a sensitive marker of exocrine pancreatic insufficiency. This technique has qualitative advantages over the methods used today for determining exocrine pancreatic insufficiency (stool lipid profile, coprogram) due to the greater specificity of the method and the lack of influence of enzymatic therapy on the results of the elastase test. The elastase content in feces should be above 200 μg/g. The level of fecal elastase from 200 to 100 µg/l indicates moderate exocrine pancreatic insufficiency, a decrease in the level of the enzyme in feces less than 100 µg/l indicates the presence of severe pancreatic insufficiency. This test has found wide use in patients suffering from cystic fibrosis and Shwachman's syndrome, since determining their level of fecal elastase makes it possible to monitor the condition of the pancreas without canceling enzyme therapy. Table 5 and Figure 1 present an algorithm for diagnosing exocrine pancreatic insufficiency based on the results of studying the level of elastase-1 in feces [8]. The previously widely used secretin-pancreozymine test (SPT) is a probe method for studying the exocrine function of the pancreas and is based on determining the content of bicarbonates and enzymes in the duodenal contents using a probe after direct stimulation of acinar and ductal cells of the pancreas. When conducting the study, the basal secretion is first determined by administering secretin (1 U/kg), which stimulates an increase in the volume of pancreatic secretion and the production of bicarbonates. Then cholecystokinin-pancreozymin (1 U/kg) is administered, which stimulates the production of enzymes and causes contraction of the gallbladder (stimulated secretion). Normal indicators of the secretin-pancreozymine test: bicarbonates - not less than 70 mmol/l, amylase - not less than 12,000 U/30 min., trypsin - not less than 3 U/30 min., lipase - not less than 65,000 U/30 min., steatorrhea – no more than 7 g/day. Based on the results obtained, it is possible to determine the types of pancreatic secretion to stimuli: • normosecretory response - increased enzyme activity, secretion volume and bicarbonate level; • hypersecretory type of secretion - an excessive increase in the concentration of enzymes with a normal or increased volume of secretion and bicarbonate levels, characteristic of mild inflammatory-dystrophic changes in the pancreas associated with hyperfunction of acinar tissue; • hyposecretory type of secretion – normal or reduced volume of juice and bicarbonate level with reduced enzyme activity, indicates a qualitative insufficiency of pancreatic secretion, characteristic of the development of pancreatic fibrosis; • obstructive type of secretion – a decrease in the volume of juice with a normal content of enzymes and bicarbonates, characteristic of duct obstruction (papillitis, duodenitis, spasm of the sphincter of Oddi, choledocholithiasis). It should be noted that in children the enzyme-synthesizing function of the pancreas is more often impaired; only with severe pancreatic insufficiency does the level of bicarbonates and secretion decrease. This test is currently not widely used due to the availability of modern sensitive and minimally invasive methods for assessing the structural and functional state of the pancreas. Instrumental research methods in the diagnosis of exocrine pancreatic insufficiency are of auxiliary value, allowing the assessment of the anatomical structure of the organ. Ultrasound examination of the pancreas is one of the leading methods of radiation diagnostics, which allows you to quickly, quite informatively, regardless of the severity of the patient’s condition, assess the condition of the pancreas: an increase in its size, changes in echo density (edema, compaction), the presence of echo-dense inclusions, the condition of the Wirsung duct. The acoustic characteristics of the unchanged pancreas include determination of the shape, contour, size, echogenicity of the internal structure and the state of the main pancreatic duct. Traditionally, in clinical practice, age standards for ultrasound sizes of the pancreas are used (Table 6). One of the main criteria for damage to the pancreas is a change in the size of the organ. Based on an analysis of more than 3,000 examined children, M.I. Pykov (1997) showed that an increase in the size of the pancreas, especially its tail part, and visualization of the dilated duct in children are evidence of increased pressure in the lumen of the duodenum. A number of authors consider a moderate increase in the size of the pancreas (or its parts) with unchanged echogenicity and homogeneous echostructure as a manifestation of functional changes in the organ of a compensated nature. At the same time, organic lesions of the pancreas are characterized by changes in size, contours, shape, echostructure and expansion of the main pancreatic duct [9]. Signs of chronic pancreatitis on ultrasound include: dilation of the pancreatic duct, detection of stones in the pancreatic duct, uneven edges of the pancreas/changes in the echostructure, the presence of pseudocysts [10,11]. Ultrasound scanners using the Doppler effect can provide data on blood flow in arterial and venous vessels. Taking into account that the earliest changes in the pancreas occur at the level of the microvascular bed, the importance of visualizing parenchymal blood flow in the pancreas for assessing its condition cannot be overestimated. The defeat of this organ is often accompanied by changes in hemodynamics in large vessels supplying blood to the upper parts of the digestive system. In the domestic literature there are only isolated reports on Doppler ultrasonography indices in normal and pathological conditions. According to V.V. Mitkova (1998), the frequency of visualization of small vessels of the pancreas using color Doppler scanning (CDS) and power Doppler (PD) ranges from 60 to 90%, with the largest number of vessels determined in the area of the head of the pancreas [12]. According to pulse-wave Doppler, the maximum systolic velocity in the small arteries of the pancreas is 30±1 cm/s, in the veins - 15 cm/s, the resistance index in the small arteries of the pancreas is 0.61±0.05. In acute pancreatitis, an increase in intraorgan blood flow is observed; as parenchymal edema increases, according to pulsed Doppler (PD), an increase in peripheral resistance indices in small arteries may be observed. As destructive processes develop in the pancreatic parenchyma, deformation of the vascular pattern in the destruction zone is recorded, and with ID - a decrease in peripheral resistance and identification of signs of arteriovenous shunting. In chronic pancreatitis, when performing CDK, a weakening of blood flow is observed, and in ID, a decrease in the speed of blood flow in the small vessels of the pancreas is observed. Endoscopic retrograde cholangiopancreatography (ERCP) is the “gold standard” for diagnosing pancreatic pathology. Using this technique, it is possible to detect expansion and deformation of the main pancreatic duct, detect duct strictures, calcium deposits on the walls of the duct, and calcification of the pancreatic parenchyma. The study also reveals changes in the biliary system: stenosing papillitis, choledocholithiasis, anomalies in the development of the bile ducts and gallbladder, etc. Indications for ERCP are: • recurrent chronic pancreatitis; • blunt abdominal trauma with severe pain; • duodenostasis; • jaundice of unknown etiology; • chronic calculous cholecystitis; • preoperative examination of patients. The main indications for computed tomography and magnetic resonance cholangiopancreatography in children: • complicated course of acute and chronic pancreatitis; • suspicion of a mass process in the pancreas and adjacent organs. Correction of pancreatic insufficiency is aimed at eliminating disturbances in the breakdown of fats, proteins and carbohydrates and involves prescribing a special high-calorie diet and enzyme replacement therapy, which can reduce the manifestations of maldigestion and malabsorption. Many enzyme preparations traditionally used by pediatricians have significant technological and pharmacological disadvantages, as well as low activity in the duodenum. When prescribing a particular drug, the doctor must first of all know its composition and have information about the activity of its components. Drugs for replacement therapy of exocrine pancreatic insufficiency in children should [13,14]: • contain lipase and be resistant to hydrochloric acid; • have a maximum effect at pH 5–7; • quickly and homogeneously mix with chyme and transport to the duodenum; • have a microtablet (microspherical) shape with a diameter of no more than 2 mm, providing a large surface of contact with the chyme. This promotes the simultaneous entry of the drug into the duodenum and the rapid release of lipase in the intestine; • be well tolerated; • not toxic. To ensure rapid and homogeneous mixing of enzymes with food chyme, to prevent intragastric inactivation and adequate passage from the stomach to the duodenum, new generation pancreatin enzyme preparations were created - Creon 10000, Creon 25000 and Creon 40000 in the form of mini-microspheres, the diameter of which does not exceed 1.4 mm. Creon 40000 mini-microspheres are coated with an enteric coating and enclosed in a gelatin capsule. When it enters the stomach, the capsule quickly dissolves, mini-microspheres are mixed with food and gradually enter the duodenum. When the pH of the duodenal contents is above 5.5, the membranes dissolve and the enzymes begin to act on a large surface. The mechanism of action of Creon 40000 allows you to reproduce the physiological process of digestion, in which pancreatic juice is secreted in portions in response to the periodic intake of food from the stomach. The drug is characterized by an optimal ratio of lipase and protease activity, as well as a high content of carboxylesterolipase and phospholipase A2 for the most effective breakdown of fats. The success of therapy for exocrine pancreatic insufficiency depends on many reasons. The most convenient and physiological way for the patient is to take enzyme preparations with meals. In the case of an adequately selected dose and form of the enzyme preparation, a significant improvement in the patient’s condition occurs. The criteria for the effectiveness of treatment are the disappearance of polyfecal matter, reduction or elimination of diarrhea, increase in body weight, disappearance of steatorrhea, amilorrhea and creatorrhoea. The dose of the enzyme preparation is selected individually within 1 week. treatment depending on the severity of exocrine pancreatic insufficiency. It is advisable to calculate the dose of the enzyme preparation based on lipase and start with a small one (1000 IU of lipase per kg of weight). If there is no effect, the dose of the drug is gradually increased under the control of scatological studies. For severe exocrine pancreatic insufficiency, we use 4000–5000 IU of lipase per kg of body weight. The duration of therapy is determined individually. Enzyme intake is stopped if clinical and scatological signs of maldigestion and malabsorption disappear.
Literature 1. Lerner A., Branski D., Lebenthal E. Pancreatic diseases in children // Pediatr. Clin. North Am. 1996. Vol. 43. R. 125–156. 2. Cox KL, Ament ME, Sample WF, Sarti DA, O'Donnell M., Byrne WJ The ultrasonic and biochemical diagnosis of pancreatitis in children // J. Pediatr. 1980. Vol. 96 (3 Part 1). R. 407–411. 3. Frank B., Gottlieb K. Amylase normal, lipase elevated: is it pancreatitis? A case series and review of the literature // Am. J. Gastroenterol. 1999. Vol. 94. R. 463–469. 4. Russell MK Acute pancreatitis: a review of pathophysiology and nutrition management // Nutr. Clin. Pract. 2004. Vol. 19. R. 16–24. 5. Gubergrits N.B., Golubova O.A. Laboratory diagnosis of pancreatic diseases / Medical laboratory diagnostics (programs and algorithms) / ed. A.I. Karpishchenko. St. Petersburg, 2001. 6. Henderson D.M. Pathophysiology of the digestive organs. M.: Binom, 1997. P. 288. 7. Korovina N.A., Levitskaya S.V., Budakova L.V., Kameneva O.P. Diagnosis of pancreatitis in children. M., 1989. 24 p. 8. Belmer S.V., Gasilina T.V. Digestive pancreatic insufficiency in children. Differentiated approach // Russian Medical Journal. 2007. No. 1. P. 57–60. 9. Pykov M.I. Doppler examination of pancreatic vessels in children // Ultrasound and functional. diagnostics. 2001. No. 2. P. 53–57. 10. Zagorenko Yu.A. Clinical and pathogenetic assessment of information content and modern possibilities for optimizing ultrasound diagnostics of chronic recurrent pancreatitis // Med. visual 2002. No. 1. P. 48–58. 11. Zubarev A.V. Ultrasound monitoring of the treatment of acute pancreatitis // Med. visual 2000. No. 4. P. 21–24. 12. Mitkov V.V., Bryukhovetsky Yu.A., Kondratova G.M. Color Dopplerography and eneogetic Doppler in ultrasound examinations of the pancreas. Clinical physiology. Diagnostics - new methods. M., 1998. pp. 177–180. 13. Yakovenko E.P. Enzyme preparations in clinical practice // Clinical pharmacology and therapy. 1998. No. 7. P.17–20. 14. Graham DY Treatment of exocrine pancreatic insufficiency // Pract.Gastroenterol. 1980. Vol. 4. R. 18–23.
Is MRI performed for diseases of the pancreas?
The reason to sign up for a magnetic resonance examination of the abdominal cavity and retroperitoneal space is the detection in laboratory parameters of changes characteristic of damage to the organs of the biliary system
MRI for diseases of the pancreas is done to identify pathology, determine the stage of the disease and detect complications. The images provide the doctor with valuable information for making a diagnosis. The doctor analyzes:
- location, size and internal structure of the gland;
- zonation of the organ - features of visualization of the body, head and tail;
- involvement of parapancreatic tissue in the pathological process, spread of the tumor to nearby tissues, connection of the neoplasm with the pancreas, damage to the lymph nodes;
- configuration, tumor density, blood supply characteristics, presence of areas of necrosis, calcification (allows to differentiate benign and malignant processes);
- consistency of anastomoses after liver transplantation;
- changes in the parenchyma, the severity of inflammation;
- parasitic lesions;
- developmental anomalies;
- modification of the ducts of the pancreatic and biliary tract as a whole, the presence of strictures, localization, stone formation;
- changes in the retroperitoneal space etc.
Taking into account the absence of long-term consequences after the diagnostic procedure, the study is suitable for dynamic monitoring of cystic neoplasms and monitoring the effectiveness of therapy.
Final diagnosis
It is important not to miss any ailment associated with pancreatic disease. The availability of ultrasound in this situation cannot be overestimated. The sooner changes in the organ are detected and appropriate measures are taken, the greater the chance of cure.
The diagnosis is made only by a doctor based on a combination of clinical manifestations, laboratory parameters and instrumental studies. In the future, dynamic monitoring of changes in the condition of the gland is needed.
The main contribution from the patient is not only strict adherence to treatment recommendations, but also maintaining a healthy lifestyle, giving up bad habits, overeating, abuse of alcohol, sweets, fatty and fried foods.
Important for the health of the pancreas is maintaining immunity, protecting against stress, and eliminating household and professional intoxications.
MRI of the pancreas: indications
What is better, to do a magnetic resonance or computed tomography, the doctor decides, taking into account the clinical situation and restrictions on the use of the method
There are many indications for MRI of the pancreas. It is recommended to sign up for the procedure if:
- pain in the epigastric region, abdomen, indigestion, inexplicable by tests and ultrasound, appeared, indigestion - foul-smelling stool, unusual color of stool, nausea, vomiting, flatulence, jaundice, etc.;
- family history is burdened - several first-degree relatives have been diagnosed with pancreatic cancer;
- preoperative diagnostics are necessary to study the anatomical features and plan the intervention;
- ultrasound results are ambiguous/suspicious for pancreatic pathology, which implies advanced diagnostics;
- differentiation between cancer and chronic pancreatitis is required;
- deviations from the norm in laboratory parameters indicate disease of the pancreas, gallbladder, ducts, liver;
- there is a suspicion of a tumor in the biliary system, it is necessary to determine the stage of the oncological process, relapse after treatment;
- there are contraindications to computed tomography, including enhanced CT (pregnancy, childhood, allergy to iodine-containing contrast, renal failure, hyperfunction of the thyroid gland);
- There is no effect of therapy for pancreatitis / frequent exacerbations are observed when following a diet (MRI of the pancreas shows choledocholithiasis, intraluminal stones, stage of inflammation);
- it is necessary to exclude postoperative complications, etc.
Where to do an ultrasound of the pancreas
You can undergo an ultrasound scan of the pancreas at the MedCenterService clinic network. Our patients receive many benefits:
- High-quality diagnostic result. The examination is carried out using the latest generation equipment.
- Competent approach, politeness and courtesy. The appointments are conducted by doctors with extensive experience and a high level of qualifications.
- Convenient location and comfortable environment. The clinics are equipped taking into account modern medical standards and the wishes of patients.
How is an MRI of the pancreas done?
The greatest diagnostic value is for images obtained on high-field units with a closed contour
Before scanning, you must leave items containing metal in the storage compartment. A cell phone or payment card forgotten in a pocket when exposed to a magnetic field causes distortion in the photo.
After completing the documentation, the x-ray technician escorts the patient to the diagnostic room and places him on the scanner table. The limbs are fixed with soft belts and bolsters, and an intensifying coil is placed above the abdomen.
If an MRI of the pancreas with contrast is planned, a catheter is inserted into the vein. During certain phases of the study, a chelated gadolinium enhancer will be automatically delivered through the drain (using an injector) to improve visualization.
Medical staff monitors the progress of the diagnosis through glass from an adjacent room. Communication takes place via speakerphone; in case of an unforeseen event (an attack of claustrophobia, deterioration in health), the patient has a special signal button at hand. Technical noise produced by equipment can be leveled out using headphones.
After the native series of images, there is a wait for the dye to spread through the bloodstream to the organs of the biliary tract. The duration of MRI with contrast is 30-45 minutes. The results will be ready within an hour. There are no obstacles to daily activities.
How does the ultrasound protocol describe a normal pancreas?
The human pancreas at birth has a length of up to 5.5 cm and increases during the first year of life to 7 cm. The size of the head initially does not exceed 1 cm. Then growth continues until approximately 18 years.
Therefore, the norm in children varies depending on age and weight; to determine the pathology, calculations are made using special tables. The experience of the doctor conducting the study is also important.
In addition to the length, which reaches from 16 to 23 cm in adulthood, the pancreas has a width of up to 9 cm and a thickness of up to 3 cm, which smoothly decrease from head to tail.
The structure of the gland is normally homogeneous, consisting of small lobules that produce digestive juice and islets of cells that secrete hormones that regulate carbohydrate metabolism.
A duct called the Wirsung duct is visible in it; its width normally should not exceed 2 mm.
During the ultrasound examination, a comparison is made with normal values. How is the pancreas described in the protocol? Dimensions, standard:
- pancreatic head size – up to 32 mm;
- body – up to 25 mm;
- tail - about 30 mm;
- contours are smooth and clear;
- the diameter of the Wirsung duct is 1.5 - 2 mm and its expansion to 2.5 - 5 mm in response to intravenous administration of secretin;
- additional education – no;
- echostructure – homogeneous, similar to the echostructure of the liver;
- echogenicity – neither increased nor decreased.
An increase in the echogenicity of pancreatic tissue with age is not always associated with pathology.
This is what the norm looks like in adults.
Changes in size, contours and echostructure indicate the presence of congenital or acquired pathology of the organ.
MRI of the pancreas, how to prepare?
Ask your doctor if you have any questions about MRI scans.
Magnetic resonance imaging is often performed routinely; in urgent situations with an acute abdomen, it is preferable to do a CT scan. Preparation for an MRI of the pancreas implies:
- Obtaining a referral for research. The document must indicate the intended diagnosis, area/s of interest, type - with or without contrast;
- Dieting. A few days before the procedure, products containing starch, yeast, sugar - baked goods, confectionery - are excluded from the diet. Excessive flatulence and fermentation processes in the intestines are caused by fresh vegetables (cabbage, peas, beans), fruits, herbs, mushrooms, milk, brown bread, etc. Alcohol, kvass and drinks with gas can cause the movement of small stones and accompanying inflammation, which will provoke swelling of the gland and gallstone colic. You should avoid fatty meats, fish, smoked meats, marinades, and spices. A 6-hour fast is required before the test. The paramagnetic gadolinium and prolonged lying on the back can cause autonomic reactions in the form of dizziness, nausea, and drooling. You can prevent such phenomena by having a light snack 30 minutes before leaving the house.
- Taking medications. Medicines for routine therapy are taken as usual. Antispasmodics, enzymes, adsorbents, laxatives are used exclusively on the recommendation of a doctor. An enema is needed for chronic constipation (if it is planned to examine all organs of the gastrointestinal tract).
Don’t forget to take with you the results of ultrasound, FGDS, images and descriptions of previously performed MRI/CT, epicrisis from the hospital, conclusion of the oncoconsilium. If the study is paid for by an insurance company, a compulsory medical insurance or voluntary health insurance policy will be required.
How to prepare for an ultrasound examination?
A routine ultrasound examination of the abdominal organs must be carried out on an empty stomach, the stomach must be empty. Otherwise, the reliability of the study is significantly reduced.
Imaging accuracy may be affected by increased gas production in the intestines. It needs to be minimized and intestinal motility improved.
Therefore, on the eve of a scheduled ultrasound, a gentle diet is recommended for 2-3 days, avoiding legumes, black bread, cabbage, carbonated drinks, and sweets. The last meal should be no later than 19 hours before the test day.
Preparation for an ultrasound of the pancreas and neighboring organs may include taking activated charcoal, laxatives, enzymes and drugs that reduce gas formation.
In emergency cases, ultrasound can be performed without preparation.
What can you eat before an MRI of the pancreas?
It is preferable to prepare dishes using gentle heat treatment - boiling, baking, stewing
To ensure that food is fully digested, the following are allowed on the eve of the procedure:
- lean meat, dietary fish, skinned chicken breast;
- baked vegetables and fruits;
- porridge with water;
- omelettes;
- unrich broths;
- crackers, dry cookies;
- vegetable oil in small quantities;
- unsweetened compotes, still water, herbal teas, diluted juices without pulp.
Normal size of the pancreas on MRI
Organ parameters are variable:
| Department | Dimensions (mm) |
| Head | 11- 35 |
| Body | 4- 30 |
| Tail | 7- 30 |
The concept of normal on magnetic resonance images is relative. Sizes depend on gender, height, age, food load. A slight deviation from generally accepted indicators, provided the structure of the organ parenchyma is normal and functions are intact, is not considered a pathology. The length of the pancreas is 15-23 cm, width 4.5-6 cm, weight about 70-80 grams.
Normally, the organ is not enlarged, the contours are clear, even, and the dimensions correspond to the person’s build. The pancreatic duct is not dilated, the surrounding tissue is without any features. No changes in the MR signal were detected.
Indications and contraindications
Ultrasound of the pancreas is prescribed in the following cases:
- after abdominal trauma;
- in the presence of diabetes mellitus;
- if the results of laboratory tests are negative and indicate pathology of the gland;
- the presence of pathology from the stomach, liver, intestines, spleen;
- if you suspect cancer;
- with jaundice of non-infectious origin;
- after chemical poisoning.
It is recommended to undergo an ultrasound examination of the pancreas if the following symptoms appear:
- pain in the upper abdomen and projection of the pancreas of a girdle, aching or acute nature;
- sudden weight loss for no reason;
- flatulence, constipation and diarrhea;
- the presence of undigested food in the stool;
- nausea and vomiting accompanied by severe pain in the upper abdomen.
Regular ultrasound scanning of the pancreas is recommended for patients at risk:
- people who abuse alcoholic beverages;
- those who consume large amounts of junk food with artificial flavors and other chemical additives, as well as fatty and fried foods;
- in the presence of a genetic predisposition to pathologies of the abdominal organs;
- if there are episodes of acute pancreatitis in the anamnesis;
- with long-term drug therapy for any chronic diseases.
The study can also be carried out for prophylactic purposes at the request of the patient.
There are no contraindications to the procedure; ultrasound diagnostics is considered completely safe and is therefore prescribed to patients of all ages. The exception is severe skin damage from ulcers or wounds, in which it is impossible to use an external sensor. It is not advisable to conduct the study on the same day as FGDS or colonoscopy, since excess air, which is pumped during endoscopic procedures, can interfere with the propagation of ultrasonic waves.
The use of radiopaque diagnostic methods with the introduction of barium within 24 hours before performing ultrasound diagnostics is also not indicated.