INDICATIONS. This resection is usually an emergency operation used for sudden obstruction, such as gangrenous bowel in a strangulated hernia or volvulus. Less commonly, it is used for thrombosis of mesenteric vessels and obstruction due to a tumor. Because end-to-end anastomosis more accurately restores the natural integrity of the intestine, it is usually preferred to lateral anastomosis; however, the surgeon should also be familiar with side-to-side anastomosis, which is recommended if there is a noticeable difference between the sizes of the anastomosed intestines.
PREOPERATIVE PREPARATION. Preoperative measures are limited accordingly. However, before proceeding with the operation, the stomach is emptied and constant gastric suction is established.
ANESTHESIA. General anesthesia.
POSITION. On the back.
OPERATIONAL PREPARATION. The skin is prepared as usual.
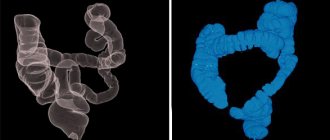
CUT AND EXPOSURE. An incision is made over the area where damage is suspected. If the location of the small bowel obstruction is unknown, a lower middle or right rectal incision is often used because the lesion often involves the lower ileum. It is best to make the incision on one side of the old abdominal scar, if there is one, because the obstruction is likely to be near this point, especially if the scar was painful before surgery. A culture of peritoneal fluid is obtained, noting its quantity, color, and consistency. Bloody fluid indicates vascular obstruction. The dilated loops of intestine are carefully pulled or removed from the abdominal cavity and placed on a warm, moist surface, covered with gauze swabs soaked in warm saline. If there is an incarceration, the surgeon must determine the viability of the affected bowel by considering the following factors: (1) cadaverous odor; (2) the presence of bloody fluid indicating venous thrombosis; (3) that peristalsis does not pass through the affected intestine; (4) that the serosa has lost its usual luster and color; and most importantly (5) the absence of arterial pulsation. Bowel that at first appears nonviable and requires resection often regains viability once the cause of the obstruction is removed and the bowel is wrapped in warm, moist gauze for a period of time. There is also a dramatic change in color of the viable intestine when 100% oxygen is inhaled. In doubtful cases, infiltration of the mesentery with a 1% solution of procaine hydrochloride can also relieve vascular spasm and restore arterial pulsations. To assess regional perfusion, intra-arterial fluorescein injection followed by ultraviolet illumination can be used. Doppler can also be useful in checking the arterial blood supply. If a tumor is present, the mesentery should be examined for metastatic nodes. If there is any doubt as to the location of the obstruction, the surgeon should without hesitation eviscerate the patient until the pathological lesion is exposed and pass the colon between the fingers, segment by segment, from the ligament of Treitz to the cecum. The surgeon must be sure that there is no secondary injury or distal cause of the obstruction.
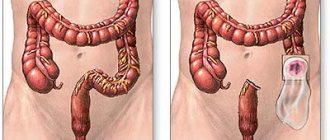
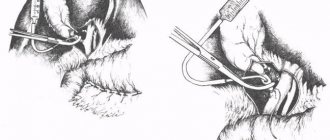
PROGRESS OF THE OPERATION. The bowel wall should be removed within 5 to 10 cm of the seriously affected area, even at the expense of several feet of small bowel (Figure 1). The intestine and mesentery are cut, and it is better to start with the mesentery (Fig. 2). The surgeon must be sure that the clamps are not applied too low at the base of the mesentery, since the blood supply to a long segment of the bowel may be accidentally interrupted; (2) that resection extends to the base of the mesentery only in the presence of malignant disease; and (3) that a large pulsatile vessel is preserved to supply the bowel adjacent to the point of resection. The intestine must be cleared of the mesentery at least 1 cm beyond the intended resection line (Fig. 2). A pair of narrow straight clamps with atraumatic teeth are applied to the intestine. The clamp on the viable part of the intestine is applied obliquely, this not only improves the blood supply to the antimesenteric border, but also provides a larger lumen for anastomosis (Fig. 3). The intestine is cut on both sides of the lesion, and the remaining intestine is covered with warm, moist swabs. The color of the bowel is again inspected to ensure that there is adequate blood supply to the bowel adjacent to the clamp and that enough serosa is exposed at the mesenteric border for suturing. If the bowel appears bluish or there is no pulsation in the mesenteric vessels, the bowel is excised until there is sufficient circulation. After the ends of the intestine are prepared for anastomosis and mobilized distally and proximally for a residual distance so that there is no tension on the anastomotic suture line, the clamps are rotated to provide access to the posterior serosal surfaces for their approximation. Enestrostomy clamps are placed along the intestine 5-10 cm from the pressure clamps to prevent leakage of intestinal contents after removal of the pressure clamps. Silk mattress sutures are placed in the serous layer at the mesenteric and antimesenteric borders. The mesenteric border had to be cleared at a residual distance so that only the serous layer and not the mesenteric fat entered the sutures. A series of interrupted 00 silk Halsted sutures are placed in the serosa using curved or straight needles (Fig. 4). Then the posterior layer of the mucosa is closed (Fig. 5). The antimesenteric angle and anterior mucosal layer are closed using an everting Connell suture (Figs. 5 and 6). The anterior serosa is then closed with interrupted Halstead sutures made of 00 silk (Fig. 7). The mesentery is brought together with interrupted 0000 silk sutures, placed so as not to injure the vessels. By invaginating the intestine using the thumb and index finger, the patency of the anastomosis is checked (Fig. 8). Silver staples can be used to mark the site of the anastomosis for further x-ray studies.
Modification of the method The lateral anastomosis method can be used. After dividing the intestine according to the operation described above, the cut ends are closed with a continuous everting suture of thin catgut through a clamp (Fig. 9). The intestinal wall is everted, and the smooth serous layer is brought together by removing the clamp (Fig. 10). Once the clamp is removed, the suture is pulled tight enough to control bleeding and occlude the lumen, and tied at the mesenteric border. The end of the bowel is closed with a serosal row of interrupted mattress sutures made of 00 silk, which should not involve fat or mesentery (Fig. 11). To avoid interrupting the blood supply, the final suture may draw the edge of the mesentery towards the point of closure, but should not evert or trap it. Straight intestinal non-crushing forceps are placed on the intestine near the mesenteric border and close to the closed ends to bypass the blind segment outside the anastomosis. While the clamps are applied, the bowel is held in place with Allis, Babcock, or surgical forceps (Fig. 12). The clamps are tied together, and the field is covered with fresh towels. Extension sutures are applied to both corners of the anastomosis (Fig. 13). Place a series of interrupted 00 silk sutures in the serezal layer. The intestinal wall is cut with a knife on both sides, close to the suture line (Fig. 13). The incision is extended with straight scissors until a stoma is two to three fingers wide. The posterior layer of the mucosa is closed with a continuous locking suture of fine catgut or interrupted sutures of fine 0000 silk (Fig. 14). The anterior mucosal layer is closed with an everting Connell suture, and the anterior serous layer is closed with interrupted 00 silk mattress sutures (Fig. 15). The corners can be reinforced with several interrupted 00 silk sutures until the closed ends of the bowel are securely attached to the adjacent bowel (Fig. 16). The mesentery is approximated using interrupted 0000 silk sutures placed to bypass major blood vessels (Fig. 16). If easy access to the stomach is available, temporary gastrostomy should be considered.
CLOSING. You can add relief seams.
POSTOPERATIVE CARE. Fluid balance is established and maintained using intravenous administration of lactated Ringer's solution. Antibiotic therapy is used. Continuous decompression is maintained through continuous gastric suction until normal bowel movements begin.