Often, an ultrasound diagnostic specialist, during a routine examination, has to diagnose pyloric stenosis, or pyloric stenosis, in young children.
This is a congenital or acquired pathology consisting in a narrowing of the pylorus (Pylorus) of the outlet of the stomach, i.e., the opening leading from the stomach to the duodenum. The disease, which occurs in an acute form, causes a lot of suffering for both the child and his parents. It occurs more often in boys than in girls.
Causes of the disease
Pyloric stenosis in a child in most cases manifests itself in the first weeks of life. It occurs as a result of congenital defects, organic damage to muscles, their cicatricial deformities or a chemical burn, the so-called pyloric region. The disease is severe, and if timely assistance is not provided, it can even lead to the death of the child.
All the causes of pyloric stenosis in children are currently unknown. But some of them are:
- severe pregnancy with toxicosis in the first trimester;
- infectious diseases;
- the expectant mother taking certain types of medications;
- maternal endocrine disorders during pregnancy.
Pyloric stenosis
Hypertrophic pyloric stenosis is a disease of children in the first month of life, caused by thickening and compaction of the circular muscle layer of the pyloric part of the stomach, which causes gastric obstruction. The incidence of this disease is 2-3 cases per 1000 newborns (P.Puri, M.Hollwarth 2009). Boys get sick 4 times more often than girls. There is a genetic predisposition to this disease. This pathology is more common in children whose parents suffered from pyloric stenosis.
Clinical symptoms of pyloric stenosis appear from the 2nd to 5th week of life. At first it may just be regurgitation, which over the course of several days turns into “fountain” vomiting soon after feeding or after some time. The child progressively loses weight and becomes dehydrated. Parents report decreased urination and constipation.
Diagnosis of pyloric stenosis is based on clinical manifestations and examination data.
Currently, a safe method for diagnosing pyloric stenosis is ultrasound of the stomach, which detects thickening of the muscular wall of the pylorus.
For additional diagnostics, if there is a discrepancy between the clinical manifestations and the echographic picture during ultrasound examination, fibrogastroscopy is performed, which makes it possible to see the narrowed whitish lumen of the pyloric part of the stomach, impassable for the instrument.
Treatment of this pathology is carried out surgically. Surgery for pyloric stenosis is not an emergency and is not performed until hypovolemic and electrolyte abnormalities have been corrected. In case of significant weight loss with late diagnosis of pyloric stenosis and low weight of the child, a probe is inserted into the small intestine beyond the pyloric area of the stomach to feed the child. This procedure allows you to fully feed the child in the preoperative and early postoperative period, avoiding large volumes of intravenous fluid.
A universal surgical intervention for pyloric stenosis is pyloromyotomy according to Frede-Ramstedt. In the avascular zone, a longitudinal dissection of the seromuscular layer of the pyloric part of the stomach is performed, followed by dilation of the muscles in a direction perpendicular to the cut line until the gastric mucosa bulges.
Currently, preference is given to performing pyloromyotomy laparoscopically. This technique is less traumatic, promotes rapid recovery in the postoperative period and provides a good cosmetic result.
Laryngeal stenosis in children
In treatment, one of the most important factors is the timely detection and correct assessment of respiratory disorders. The choice of therapy and the prognosis for curing the disease depend on this. But the main task of treatment is to eliminate suffocation and respiratory failure.
In stage I (compensation), the root cause (the primary disease that led to laryngeal stenosis) is identified and can be treated.
In stage II (incomplete compensation), therapy is repeated as in stage I.
Stages I and II are subject to drug therapy, during which the patient is in the hospital under the supervision of doctors. Treatment uses antibiotics, anti-inflammatory drugs, antihistamines, corticosteroids, and dehydration therapy.
In the case of stage III (decompensation), an urgent tracheotomy is performed, during which adequate gas exchange in the lungs is restored and cardiac activity is normalized.
In stage IV (terminal (asphyxia)), children undergo conicotomy with further resuscitation measures (artificial ventilation, intracardiac administration of adrenaline, cardiac massage, intravenous infusion of a glucose solution with insulin, potassium chloride, etc.).
At any stage, the patient is prohibited from physical activity and emotional stress. For this purpose, sedatives and psychotropic drugs are prescribed.
Children in serious condition with laryngeal stenosis are prescribed operations to restore breathing and the activity of the cardiovascular center. The type of operation is prescribed depending on the severity of suffocation, its location, and accompanying symptoms.
Tracheotomy is used to eliminate severe hypoxia and restore breathing. This surgical intervention quickly restores respiratory functions and eliminates the appearance of the glottis. Indications for this operation are acute and chronic stenosis of an infectious, traumatic and neurological nature, as well as respiratory failure in stages III and IV of the disease.
Along with tracheotomy, other types of surgical intervention (throat section) are used:
Thyrotomy – dissection of the thyroid cartilage.
Conicotomy – dissection of the conical fold.
Cricotomy – dissection of the cricoid cartilage arch.
Intubation is indicated for short-term stenosis of the larynx (from several hours to several days), as well as in case of urgent connection to a ventilator. This helps normalize breathing and eliminate complications of tracheotomy. The reasons for prescribing intubation are: inflammatory diseases and trauma to the larynx and trachea, convulsive syndrome, respiratory failure, breathing pathologies.
The incubation tube can remain in the larynx of a young child for 3-4 days, and for an older child - 7-10 days. Longer stays lead to permanent stenosis.
With laryngeal stenosis, when the child is in serious condition, or during (or after) surgery, complications may develop:
- Early complications - formed at the time of surgery, these include: bleeding, emphysema of the subcutaneous tissue (typical of children aged 1-4 years, develops within 12 hours from the moment of surgery) and mediastinum, pneumothorax.
- Injury to the esophagus, isthmus of the thyroid gland, innominate vein. The cause of these violations is incorrect insertion of the tracheotomy tube, which can lead to bleeding.
- Aspiration pneumonia occurs when blood enters the bronchi.
- Asphyxia with respiratory and cardiac arrest develops after insertion of a tube under the detached diphtheria film or non-viable flaps left in the trachea.
- Injury to the posterior wall of the trachea appears in the case of a deep or hasty incision.
- Postoperative aerophagia.
The treatment of this disease is the timely prevention of bleeding during surgery, which will help avoid consequences.
In addition to early complications, there are also late ones: difficulties that arose in the postoperative period and are associated with the removal of medical equipment used during the operation, as well as with inflammatory processes.
What are the complications of uncorrectable pyloric stenosis?
If this condition is left untreated, pyloric stenosis can lead to the following complications:
- Because a baby is always vomiting, his body never gets enough nutrients from the food he eats. This leads to slow growth and sudden weight loss.
- Nutritional deficiency leads to delayed mental and physical development. The baby may be developmentally behind children of its own age.
- Repeated vomiting irritates the stomach lining and causes tiny erosions that bleed. As a result, the child may have blood in his vomit.
- Rarely, pyloric stenosis can lead to increased levels of bilirubin in the blood - which ultimately causes jaundice.
Complications can be avoided if the child is immediately sent for diagnostics.
What are the symptoms of pyloric stenosis in infants?
Thickening of the pyloric muscle creates several pathophysiological problems at once, which lead to the following symptoms:
- Vomiting like a fountain . This is a specific symptom, one of the early signs of pyloric stenosis, which directly indicates an anomaly of the pylorus. The child will vomit violently, the contents of the stomach will be released like a fountain, almost the entire volume of food eaten. Vomiting occurs a few minutes (within an hour) after eating. Before this, the baby does not experience any visible discomfort and looks quite calm.
- Constant hunger . Because of vomiting, the child is always hungry and requires food. He eats again, starts vomiting, gets hungry again, and the cycle continues.
- Waves or ripples around the abdomen . You may notice a pulsation or wave-like movement going from the left to the right end of the baby's abdomen immediately after eating. The movement, called peristalsis, is produced by the smooth muscles of the stomach to transfer food to the small intestine. Because the pylorus does not open, additional muscle forces are used to push food through. These active tremors and muscle contractions are externally visible as ripples or waves on the surface of the abdominal cavity.
- Lean chair . There will be fewer soiled diapers, and the excrement will be only mucus or bile, with virtually no leftover food leaving the intestines.
- Abdominal pain . The baby will have constant abdominal pain, which will cause him to cry with his legs pressed against his stomach.
- Lethargy and dehydration . As the condition progresses, the child becomes lethargic and weak. This indicates dehydration due to nutritional deficiencies and metabolic alkalosis, where blood pH levels rise. Alkalosis occurs due to the loss of hydrochloric acid from the stomach through vomiting. This also leads to loss of electrolytes (especially potassium).
Attention! Vomiting in a fountain, in itself, should be a cause for concern. But, if any other symptoms are detected, you should immediately show the child to the doctor, as this condition can lead to serious complications!
What causes pyloric stenosis?
The exact cause of muscle thickening is unknown, but it is believed that sudden thickening may occur, either in utero or immediately after birth.
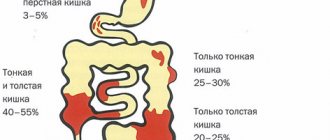
These conditions create two types of pyloric stenosis in infants:
- Congenital pyloric stenosis , also called congenital hypertrophic pyloric stenosis. It occurs when a baby develops a thickened pyloric muscle in utero.
- Acquired pyloric stenosis , or acquired hypertrophic pyloric stenosis; often observed a couple of weeks after birth, when the baby begins to receive an increasing amount of nutrition.
Experts believe that pyloric stenosis is more often acquired than congenital.
Video: Pyloric stenosis - symptoms and treatment
Specific factors increase the risk of a child developing acquired or congenital pyloric stenosis.
What are the risk factors for pyloric stenosis in infants?
The following conditions and scenarios increase a child's chances of developing the disorder:
- Age . Pyloric stenosis mainly affects children between a few weeks and six months of age. The peak incidence occurs among children three to five weeks old.
- Heredity . If the parents had pyloric stenosis, the child is 20% more likely to develop the disease. The hereditary line is not always traced, and abnormal genes are passed on through generations.
- Floor . Boys are four times more likely to develop pyloric stenosis than girls. However, it is unknown exactly how the sex of the baby influences pyloric anomaly.
- Firstborn . They have a higher incidence of pyloric stenosis, although the exact cause is unknown.
- Premature babies . Babies born prematurely are susceptible to many complications, one of which is pyloric stenosis.
- Smoking during pregnancy . Women who smoke during pregnancy are more likely to give birth to a baby with pyloric stenosis.
- Exposure to erythromycin . Children who are given the antibiotic erythromycin during the first two weeks of life are at increased risk of developing infantile pyloric stenosis. Other cases in infants occur when mothers consume erythromycin during the last two weeks of pregnancy or during the first month of lactation.
- Ethnicity . According to statistics, pyloric stenosis is common among Europeans, and less common among Latin Americans and Africans. It is rare among infants of Asian descent.
Keep in mind! These factors only increase the risk of pyloric stenosis, but their presence does not always mean the presence of the disease. If a child has any of the above factors, then parents should be careful.
You can identify pyloric stenosis by its symptoms.
What is pyloric stenosis?
Pyloric stenosis is an abnormal thickening and narrowing of the pyloric muscle (pylorus), located at the border of the stomach and small intestine. The pylorus plays a crucial role in regulating the flow of stomach contents into the duodenum, which is the initial part of the small intestine.
The pylorus (Pylorus) is a circular band of muscle that forms a sphincter that opens and closes like a valve, allowing food to move down the digestive tube. When a muscle thickens and becomes deformed, it cannot work fully and prevents the normal passage of food from the stomach to the small intestine.
The thickened sphincter and obstructed movement of food eventually cause the condition of pyloric stenosis.
The pathology is also known under other names - childhood hypertrophic pyloric stenosis, congenital pyloric stenosis and pyloric stenosis of newborns.
As mentioned, pyloric stenosis is caused by thickening of the sphincter muscles. But why does the muscle thicken?