Metastases are secondary foci in various organs, the result of the spread of a malignant tumor in the body. According to statistics, about 53% of patients with pancreatic cancer already have distant metastases at the time of diagnosis.
- Features of metastasis in pancreatic cancer
- Where do pancreatic malignant tumors most often metastasize?
- What are the dangers of metastases in pancreatic cancer? Possible complications
- Modern diagnostic methods
- Treatment of pancreatic cancer with metastases
- Forecast
It is difficult to fight such an advanced disease. Remission (complete “cleansing” of the body from tumor foci - in a sense, this term can be considered synonymous with recovery) is impossible. But there are treatments that help to slow down the progression of the disease to some extent, cope with painful symptoms and improve the patient's condition.
The goal of treating metastatic pancreatic cancer is to prolong the patient's life and control pain and other symptoms.
Stages of pancreatic cancer
Unfortunately, stage 1 cancer of this location is detected very rarely. The disease is known for its high aggressiveness, rapid spread of metastases, and even the simultaneous formation of metastases and a node in the gland.
It is believed that at the stage of intraepithelial neoplasia, benign cells have the opportunity to leave the organ and disperse throughout the body so that, having received a genetic signal for malignancy, they begin to form metastases even before clinically detectable primary cancer. This theory arose from the identification of a significant number of patients with advanced disease and a small primary tumor or no tumor at all.
- Stage 1 is a formation up to 2 cm or more, but without exiting the glandular tissue and without damage to the lymph nodes.
- Stage 2 - the node may extend beyond the gland, but there are no cancer cells in the lymph nodes, or the second option is a primary formation of any size when the lymph nodes are affected.
- Stage 3 - the cancer has spread to large vessels of the abdominal cavity and lymph nodes.
- Stage 4 - there are distant metastases, the size of the primary formation and lymph nodes are not important.
Symptoms of pancreatic cancer are often mistaken for an exacerbation of chronic pancreatitis, which has either been troubling the patient for a long time, or is considered to have occurred latently and suddenly become more active. But this is not the only reason why the disease is detected in an advanced stage in most people; there are biological reasons for this.
Acinus cell carcinoma of the pancreas
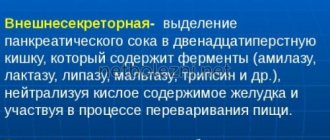
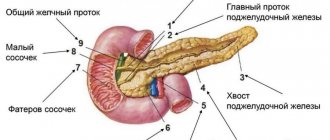
The acini is the structural and functional unit of an organ. In the case of the pancreas, the acini is a small round-shaped formation, not exceeding 0.15 mm in size. The acini consists of a secretory section and an intercalary duct, from which the ductal system of the pancreas begins.
The acini consists of ductal and secretory cells. When secretory cells are affected by a tumor, excessive production of lipase begins, which is involved in the digestion of fatty acids, fats, and acid-soluble vitamins. The presence of lipase in large quantities causes necrosis of adipose tissue and inflammation of the joints in the arms and legs.
Acinus cell carcinomas grow rapidly, increasing to 5-6 cm. At the stage when there is no metastatic liver damage, the tumor is amenable to surgical removal. Men at risk are in the age group from 55 to 65 years. Approximately at the same age there is a peak in the development of prostate cancer tumors, so men from this age group often turn to foreign specialists to undergo treatment for prostate cancer abroad.
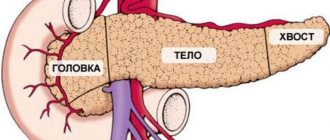
Where is the neoplasm located?
95% of pancreatic cancer is adenocarcinoma, but this is not the only cellular variant; the remaining seven malignant neoplasms account for only 5%.
It occurs in any part of the organ, in two thirds - in the head, in every sixth patient - in the body and in every 20th patient - in the tail. In some cases, it is not possible to know where the tumor grew from because of its large size, but the average diameter of a cancer tumor at initial diagnosis rarely exceeds 3 centimeters, and there are almost always metastases to the lymph nodes and often to other organs.
Prognosis of the disease: psychological aspects
The diagnosis of pancreatic cancer usually comes as a surprise to the patient, because... it is most often placed in the case of any acute disorder. The patient either suffers from discomfort in the abdominal area for weeks or suddenly discovers that the whites of his eyes have turned yellow. In this case, the diagnosis, as a rule, is made only a few days - or even a week - after the examination. The patient first simply understands that he is sick with something, and then suddenly hears that he has cancer, and it is difficult to treat: it ranks 4th in the list of the deadliest cancers in adults.
A person needs time to come to his senses. Usually he is not yet ready to listen to the oncologist’s answers to his relatives’ questions. Here are some tips that oncologists give to the patient’s loved ones:
- Family members need to get together before the medical consultation and discuss all its nuances.
- The patient should not go to the doctor alone - he should have at least one accompanying person, and this accompanying person should have a pen and paper with him.
- Before visiting the clinic, you need to discuss all the questions with the patient and make sure that he is ready to listen to the doctor’s possible answers.
Symptoms of pancreatic cancer
Symptoms caused by pancreatic cancer
These are the initial manifestations of the disease, their intensity depends on the size of the node and the involvement of other nearby organs and vessels.
Pain is the most common symptom and is caused by the spread of cancer along the nerve trunks in the form of a sleeve - perineural invasion. As the formation grows, pain appears in the epigastric region and hypochondrium. When cancer invades the retroperitoneal nerve plexuses, the pain radiates to the back and intensifies when bending forward. The intensity of pain increases in the evening and at night; it is aggravated by concomitant inflammation of the gland parenchyma, compression of the bile ducts and spasm of the vessels involved in the pathological process.
When the body and tail of the pancreas are damaged, the function of the glandular tissue is disrupted and symptoms of diabetes mellitus may develop, blood clots form in abundance, including against the background of inflammation of the venous trunks, and immune deficiency develops.
The patient loses weight, weakness increases, and fatigue increases due to “poisoning” by the growing tumor mass.
Symptoms from other organs
The gland is intimately adjacent to the liver, stomach and duodenum; with the growth of a cancerous node, they are involved in the process, which is manifested by symptoms of their inflammation and compression. This is pain and dysfunction of the gastrointestinal tract in the form of belching and anorexia. Loose stools and constipation are likely, all against the background of flatulence. Compression of the outlet of the stomach leads to nausea and vomiting of the food eaten; the formation of the tail part can partially block the lumen of the small intestine.
Compression of the bile ducts is accompanied by inflammation, hence the fever. A temperature reaction can be caused by gland tissue disintegrating due to enzymes in the cells.
A characteristic symptom of the disease is a sharp weight loss due to digestive disorders and lack of enzyme synthesis. Anemia develops.
Consult your doctor now!
Where do pancreatic malignant tumors most often metastasize?
Pancreatic cancer has a high tendency to metastasize. Even with small, less than 2 cm, malignant tumors, secondary lesions can often be detected. This partly explains why many patients already have metastases at the time of diagnosis.
Most often, secondary lesions are found in the following organs:
- Liver - in almost 80% of cases.
- In 40–50% of cases, carcinomatosis (damage by cancer cells) of the peritoneum develops.
- Lungs - in about 40% of cases.
- Lymph nodes in the abdominal cavity - 20%.
- Bones - 10%.
- Adrenal glands - 5–7%.
- Lymph nodes in the chest - 3%.
In less than 10% of cases, metastases from pancreatic cancer are found elsewhere. They can be found in almost any organ, including the diaphragm, brain, heart, gallbladder, kidneys, small and large intestine, pericardium, ovaries, testicles, stomach, skin, thyroid gland, spleen, uterus, bladder.
Even in cases where pancreatic cancer is operable and seemingly at an early stage, there are often already micrometastases in the abdominal organs and bone marrow. is most prone to hematogenous (through the bloodstream) spread, and to a lesser extent - malignant tumors of the head.
Pancreatic cancer can recur as distant metastases after treatment. For example, according to statistics, in 2/3 of operated patients with stages I and II of a malignant tumor, secondary lesions are subsequently discovered.
Undoubted causes of pancreatic cancer
The causes of pancreatic cancer will help reveal ways to prevent a disease in which the incidence rate is slightly higher than the mortality rate. This is a male tumor; women are affected three times less often and at a much older age. Diagnostics in Europe is better, and therefore the incidence is higher.
To date, no single root cause of the disease has been identified, but certain pathological conditions significantly increase the risk of malignant pathology of the pancreas.
Smoking tobacco doubles the risk of malignant tumors of the gland; for every fourth smoker, tobacco becomes the main cause of the disease. The likelihood of pancreatic cancer is directly dependent on the duration of the bad habit and the volume of daily cigarette portions.
The second proven cause of morbidity is type 2 diabetes, which is not congenital, but acquired. A diabetic's risk of developing a malignant tumor increases by 60%, and after the age of 50, every hundred diabetics are diagnosed with pancreatic cancer.
The third reason is chronic pancreatitis of any etiology; it increases the likelihood of tumor pathology by 20 times. Inflammation leads to intraepithelial neoplasia, which for most patients is a direct path to cancer. With neoplasia, cells divide too quickly, losing the ability to recover when damaged, and the slender architecture of glandular tissue is lost. The same proliferative processes in an aggravated form also occur in malignant neoplasms.
Heredity as a cause of cancer
Every 50th patient with chronic pancreatitis has a hereditary form of inflammation of the pancreas, with it the likelihood of malignant degeneration of the pancreas increases 50 times, and the disease is diagnosed in four out of ten patients suffering from pancreatitis. If you also smoke with such a genetic background, then a malignant neoplasm will appear at a younger age. And the culprit is a gene that is unable to stop the synthesis of the enzyme trypsin, which is produced in excess and causes the digestion of pancreatic cells, which leads to the formation of neoplasia.
Every 20th patient with pancreatic cancer has a hereditary tumor. When a parent has cancer, the likelihood of his offspring getting sick doubles; when both parents are sick, it increases sixfold; if three first-degree relatives are sick, it increases 30 times. But which genes regulate family transmission have not yet been precisely determined.
In the United States, the incidence of pancreatic cancer in African Americans is half that of whites, which may be related to genes.
Suspicious but not proven risk factors
A diet rich in animal proteins and poor in plant components has long been suspected as the cause of the pathology, but clinical studies have not yielded convincing evidence. It is believed that the effect of meat is aggravated by coffee, but no scientific basis has been found for this hypothesis.
However, immigrants who come from regions with low incidence and live long enough in a country with high incidence have a comparable risk of getting sick to the local population. And the reason is the inevitable change in diet.
A connection between the pathology and obesity is assumed, but this is also an unconvincing hypothesis.
Infectious diseases have also contributed to the causes of pancreatic neoplasms, similar to the fundamental role of the hepatitis virus in the initiation of liver cancer. But the role of Helicobacter pylori infection has not yet been proven for the development of pancreatic tumors.
There is an assumption that the removal of the stomach or gallbladder does not leave a permanent mark on the pancreas.
Diagnosis of pancreatic cancer should confirm or reject the malignant nature of the disease, determine its prevalence and exact localization in the gland. In case of an unconditionally resectable tumor, verification - morphological confirmation of cancer can be carried out during surgery.
Reviews from our patients
- Review of the treatment of obstructive jaundice
Review of the treatment of obstructive jaundice April 9, 2021The patient was admitted with severe signs of jaundice. During hospitalization, his condition stabilized. For this purpose, drainage of the bile ducts was carried out, as well as exposure to medications. After receiving the results of the histochemical study, further treatment tactics will be determined.
read more
- “They have golden hands”...
“They have golden hands”... April 7, 2021
Patients are being treated at the Medicine 24/7 clinic. During the treatment, they managed to become friends and this time decided to record a joint review. They thank all the clinic staff for the high organization of all processes and the effectiveness of the procedures.
read more
- Chemotherapy - review by Olga Stepanovna
Chemotherapy - review by Olga Stepanovna April 6, 2021
The patient is hospitalized for the third time. During a comprehensive examination, a puncture of the tumor was performed. Histological analysis made it possible to verify the diagnosis and determine treatment tactics. At the first stage of treatment, surgery was performed. The tumor was radically removed. Drug treatment is now being carried out to prevent the possibility of relapses. To date, the first course of chemotherapy has been completed. The patient was discharged home in satisfactory condition.
read more
- “You are the only clinical organization that brings benefits to people”...
“You are the only clinical organization that brings value to people”... April 6, 2021
The patient was admitted for treatment of cancer. The hospitalization lasted a week. The patient notes that they immediately responded to all his problems and provided assistance in a timely manner. He compares the Medicine 24/7 clinic with other medical institutions. Patient o...
read more
- Review of the attending physician M.Kh. Mustafaeva
Review of the attending physician M.Kh. Mustafaeva April 2, 2021
The patient was hospitalized in serious condition. Complex treatment was carried out. A positive effect has been achieved. The patient’s wife thanks her husband’s attending physician Milana Khanlarovna Mustafaeva. She says: “From the first day, from the first minute, as soon as we came to you, we immediately felt and understood each other. You understood the patient, you understood me. You have defined to the depth of the volume that we need. Although I couldn't explain how...
read more
- Feedback on the treatment of breast disease
Feedback on the treatment of breast disease April 1, 2021
The patient was hospitalized with breast disease. By decision of the council, surgery was performed at the first stage of treatment. It was successful. On the third day the patient was discharged home. After histological examination, further treatment tactics will be determined.
read more
- Feedback on the treatment of ascites
Review of the treatment of ascites March 30, 2021
The patient contacted the Medicine 24/7 clinic for treatment of ascites and pleurisy. These conditions are characterized by abnormal accumulation of fluid in the abdominal and pleural cavities, respectively. This happens with cancer. A laparocentesis procedure was performed, during which the fluid was evacuated. The patient's condition improved markedly.
read more
Diagnosis of pancreatic cancer
What diagnosis of pancreatic cancer is necessary?
The pancreas can be examined by ultrasound; tumors in the tail are not very visible, since they are covered by other hollow organs of the gastrointestinal tract. Large fatty tissue of the abdominal wall and cavity, which is typical for men, as well as intestinal gas formation interfere with the examination. Ultrasound diagnostics reveals formations of more than a centimeter.
Neoplasms smaller than a centimeter are detected by a combined diagnostic method - endoscopic ultrasound, when an optical examination from the inside and an ultrasound scan are simultaneously performed. Moreover, the gland can be examined both from the stomach with the duodenum, and from the bile duct or pancreatic duct and the abdominal cavity during laparoscopy. Endosonography allows you to take material for microscopy from a suspicious formation with a thin needle.
There are good prospects for diagnosing pancreatic pathology with MRI with contrast and X-ray (X-ray CT), and spiral CT with angiography will clearly reveal the relationship of cancer with nearby large vessels.
When is diagnosis with biopsy necessary?
A biopsy allows you to take a piece of tumor tissue for examination to eliminate all doubts about the nature of the tumor. If an operation is planned, then a preoperative biopsy can be abandoned and material for microscopy can be taken during the intervention. When the tumor cannot be removed for chemotherapy or radiation, it is necessary to accurately diagnose the malignant process, so a biopsy is required.
In addition, in 5% of cases, a malignant tumor in the pancreas has a structure other than cancer and requires different treatment. Unfortunately, none of the diagnostic methods can give an accurate answer to “what it is”, except for examination under a microscope. A pancreatic biopsy is performed under ultrasound or CT guidance and does not pose any danger to the patient.
Additional and clarifying diagnostics
Esophagogastroduodenoscopy (EGD) is always performed, since it will accurately indicate the involvement of the duodenum in the tumor process, which is very likely, because the pancreas is located in close proximity.
A complex diagnostic study under the abbreviation ERCP means the introduction of contrast into the ducts during endoscopy, useful in the absence of morphological confirmation, since it allows one to distinguish cancer from pancreatitis, but is not at all free from complications.
If there are ambiguities in the interpretation of RCT, angiography - X-ray with contrasting of blood vessels - can resolve the situation.
Laparoscopy may be required if metastatic lesions of the peritoneum and ascites are suspected - the formation of pathological fluid in the abdominal cavity.
Pancreatic cancer markers
With pancreatic cancer, CA 19–9, CEA, CA 50, CA 72.4 and CA 242 may increase; only the first two are of practical importance. True, these markers also increase in other diseases, so their level can be used to assess the results of treatment and the course of the process with an initial increase in concentration. If during the initial diagnosis the patient’s marker level was normal, then monitoring is questionable.
The normal value of CA 19–9 is below 37 U/l. It has been noted that when the tumor is widespread, its concentration is higher than when the cancer is small.
Carcinoembryonic antigen (CEA) normally does not exceed 2.5 ng/ml in non-smokers; in smokers it is slightly higher, but not more than 5 ng/ml. With advanced cancer, a directly proportional relationship is observed - the concentration of CEA is higher.
Diagnostic methods
Since there are no effective routine screening tests that can diagnose pancreatic cancer in asymptomatic stages, screening usually begins when a doctor detects symptoms in a patient that may indicate the disease. They start with the simplest and most accessible diagnostic methods that help detect a tumor. Once it is detected, additional studies are prescribed to clarify the diagnosis.
Often the examination begins with an ultrasound . Along with classical ultrasound, endoscopic ultrasound is used, when the sensor is located at the end of a catheter inserted into the duodenum. If a tumor is found, a needle can be passed through the catheter and a biopsy performed.
MSCT - multiphase spiral computed tomography - is performed after intravenous administration of a special contrast solution. The study helps to identify pancreatic cancer and its spread to neighboring organs, and to correctly guide the needle during a biopsy.
MRI - magnetic resonance imaging - is used less frequently than CT, since it is a more complex study that requires special equipment, which is not available in every clinic. If a pancreatic tumor is suspected, various modifications of MRI are used:
- MRI cholangiopancreatography allows you to study the pancreas and surrounding tissues.
- MRI angiography is a study of blood vessels.
PET - positron emission tomography - is an ideal tool for searching for metastases. A safe radioactive compound is injected into the patient's body, which accumulates in cancer cells. Because of this, they become visible in special photographs. Sometimes a PET scan is performed in conjunction with a CT scan to better understand where the metastases are located.
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that helps examine the bile ducts and pancreatic duct and detect narrowing in them. A radiopaque contrast agent is injected into the duct using an endoscope inserted through the mouth, after which radiography is performed. During the procedure, you can perform some manipulations:
- Take a piece of tissue for biopsy.
- Install a stent to restore bile flow.
Percutaneous transhepatic cholangiography is performed if ERCP cannot be performed. In this case, a radiopaque substance is injected through a needle inserted through the skin. During the procedure, a biopsy can also be performed and a stent installed.
A blood test for bilirubin is used to diagnose the causes of jaundice. It helps to find out what is causing the symptom: liver damage or blockage of the biliary tract.
A blood test for tumor markers - substances whose levels increase in the blood with pancreatic tumors. Most often, the level of the marker CA 19-9 , less often - CEA ( carcinoembryonic antigen ). For diagnosis, such tests are unreliable. Sometimes with stage 4 pancreatic cancer, the levels of tumor markers are normal, but in healthy people they are elevated. However, this is a useful diagnostic method for tracking the patient's condition over time and monitoring the effectiveness of treatment.
A biopsy is the most accurate method for diagnosing cancer. It can be performed with a needle through the skin, endoscopically, during ERCP or percutaneous transhepatic cholangiography.
Jaundice due to pancreatic cancer
A tumor that has reached a significant size causes jaundice due to compression of the liver ducts, itching of the skin appears, urine darkens, and feces become light.
Nausea increases, appetite completely disappears, vomiting, dry mouth, and diarrhea appear. Ulcers may appear on the skin, and pustular lesions are more common. The patient quickly becomes exhausted and loses strength.
Treatment for obstructive jaundice
Jaundice is evidence of severe liver dysfunction, which significantly worsens the patient’s condition and leads to death, therefore, in the presence of such a complication of pancreatic cancer, the outflow of bile is first restored. How this will be done is determined by the extent of the narrowing of the bile duct, the possibility of removing the cancer-affected gland, and the patient’s condition.
To remove bile, one of three manipulations is performed:
- The least complicated and with fewer complications is puncture through the skin of the bile ducts and installation of a drainage tube that drains the resulting bile.
- Drainage of the bile duct during endoscopy with stent installation often causes serious complications and after some time is dangerous for relapse of jaundice, so it is performed before radical surgery on the pancreas.
- The most complex surgical method involving the formation of anastomoses—connections of the bile ducts with the gastrointestinal tract—is also not free from complications.
Pancreatic cancer treatment
Treatment of operable cancer
Treatment tactics for pancreatic cancer depend on the stage and shape of the tumor. Complete removal of a part of the gland or an entire organ affected by the tumor is considered radical. There are various types of pancreatic resections, but when there is a tumor in the head of the pancreas, they often resort to complete removal - pancreatectomy.
After the surgical stage, multi-course prophylactic adjuvant chemotherapy is required. It is preferable to use gemcitabine, as it is the least toxic in comparison with other effective drugs. To determine sensitivity to it, an analysis is performed for the hENT1 protein; if there is no protein, then the drug will not be delivered to the tumor cell, so chemotherapy is performed with other drugs.
Learn about modern approaches to cancer therapy
Tactics for large pancreatic cancer
If the prospects for removal are questionable or there is uncertainty about the complete radicality of the future intervention, chemotherapy is performed at the first stage, the same gemcitabine is used. It is possible to join drug treatment and irradiate the gland. After 2–3 months of therapy, a follow-up examination is carried out; if the tumor has decreased, organ resection is performed. After the operation, chemotherapy continues, but its nature is preventive.
Forecast
To assess prognosis in oncology, the five-year survival rate is used - the percentage of patients who remain alive within five years from the date of diagnosis. For pancreatic cancer with metastases, this figure is about 3%. This is the worst prognosis among all tumors of the digestive system.
But even such a terrible diagnosis is not a reason to give up. There are effective treatments that help prolong the patient's life. Literally every year the possibilities of oncology are growing. Even if the patient managed to give an extra week of life without pain and other painful symptoms, it was worth fighting for. For us there are no hopeless patients. Contact us to find out more about treatment options at the European Clinic.
Book a consultation 24 hours a day
+7+7+78