In recent decades, there has been significant progress in the treatment of bleeding from esophageal varices, but an acute episode of bleeding remains a severe complication of liver cirrhosis and often acts as a turning point in the development of the disease, leading to death. Mortality in such cases reaches 20% [1, 2]. One of the key technologies in the treatment and prevention of portal bleeding remains endoscopic ligation of esophageal varices [3, 4]. Endoscopic ligation is considered a fairly safe procedure with few complications [5]. As a rule, we are talking about transient dysphagia and slight chest pain in the first days after ligation [6]. Some authors report the formation of a cicatricial stricture of the esophagus in 1.9% of cases [7]. Isolated casuistic complications were also noted: dislocation of the distal cap from the endoscope into the lumen of the esophagus [8], complete obstruction of the esophagus by a varicose node formed by a ligature [9]. The stages of pathological changes in the ligation zone have been well studied [10]. After strangulation of a varicose node, thrombosis, ischemic necrosis occurs, followed by detachment of the ligature. Small superficial ulcers heal within 2-3 weeks with the development of fibrosis in the mucous and submucosal layers. If the rubber ring prematurely slips off the varix before thrombosis forms, defects with gaping vessels may be exposed [11]. It is in this situation that episodes of bleeding from the esophagus occur after endoscopic ligation [12]. There are few publications in the literature on postligature bleeding in patients with liver cirrhosis [13]. Risk factors for such a complication, independent of the surgical technique, include a low prothrombin index, reflux esophagitis, a history of bleeding from varicose veins, and a low level on the APRI scale [14]. Another study noted that patients with postligature bleeding had lower levels of hemoglobin, hematocrit, and albumin; the severity of liver disease according to the Child-Pugh scale was also an aggravating factor [15]. However, it is reasonable to assume that premature slipping of the ligature may also be due to high tension in the varicose node, reflecting the degree of portal hypertension. It is known that the probability of bleeding from a damaged varicose node increases with increasing pressure in it, which is proportional to the pressure gradient in the hepatic veins [3]. It is necessary to clarify the effect of pressure in the esophageal veins on the outcome of endoscopic ligation.
The purpose of our study is to determine the leading prognostic risk factors for premature ligature slippage with the development of bleeding in patients with liver cirrhosis.
Causes of varicose veins of the esophagus
The cause of this disorder is most often portal hypertension, that is, an increase in pressure in the portal vein. Its causes may be liver disease (cirrhosis, chronic hepatitis, tumors, tuberculosis, echinococcosis, etc.), thrombosis or compression of the portal vein (tumors, cysts, adhesions, bile duct stones, etc.). Less commonly, varicose veins of the esophagus occur due to increased pressure in the systemic bloodstream, for example, in chronic cardiovascular failure. When the outflow of blood is difficult, the veins of the esophagus expand, twist and lengthen, forming varicose nodes; the walls of such vessels become thinner and can rupture, causing bleeding.
Material and methods
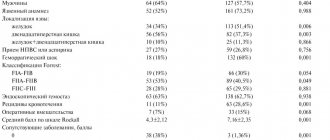
The characteristics of the patients participating in the study are presented in Table. 1.
Table 1. Characteristics of patients participating in the study
The “Control” group included patients who underwent endoscopic ligation in 2010–2015. with a favorable outcome (98), the “Case” group consisted of patients who developed bleeding associated with slipping of the ligature in the immediate post-manipulation period [5].
103 patients with liver cirrhosis (54 men, 49 women, average age 6.6±13.54 years) underwent 193 sessions of endoscopic ligation for prophylactic purposes in 2010-2015, including: 19 patients - once, 72 - twice , 10 patients - three times. The patients experienced bleeding of varying intensity from the area where the ligature was applied, which was confirmed during esophagogastroduodenoscopy (EGD), while other (non-varicose) sources of bleeding were excluded. Hemorrhages occurred from 1 to 8 days after the intervention, in 4 patients after the first ligation, in 1 - after the second one. All ligation sessions were performed by one doctor with experience in performing this manipulation in more than 200 cases. The procedure for ligating esophageal varices was typical in all cases: under intravenous sedation, varicose veins of the esophagus were visualized, the degree and prevalence of varicose veins was determined according to the Scherzinger classification (grade I - vein diameter 2-3 mm, grade II - vein diameter 3-5 mm, grade III degree - vein diameter more than 5 mm [16]) and Sarin classification [17]. Blood pressure measurements in varixes were performed using endosonography using a Waldmann apparatus (patent No. 2456913 dated October 27, 2010) (Fig. 1). This method of measuring blood pressure in the veins of the esophagus combines direct endoscopic examination and ultrasound scanning. During endoscopy, the distance from the incisors to the most dilated venous nodes was measured. Subsequently, a probe with a rubber balloon at the end and an ultrasonic sensor in it was passed over the same distance. Deaerated water was pumped into the cylinder. Under the influence of increasing pressure, the veins of the esophagus were compressed, the blood flow stopped, which was visually determined on the monitor screen based on the ultrasound picture and Doppler ultrasound data. At this moment, using a Waldmann apparatus connected through a T-shaped adapter to a balloon, the pressure was determined, which corresponded to the venous pressure in the veins of the esophagus.
Rice. 1. A device for measuring pressure in the veins of the esophagus.
Endoscopic studies in combination with endoscopic ultrasonography and pressure measurements in esophageal varices were performed on an OlympusExera II series 180 endoscopic complex using ultrasound mini-probes with a scanning frequency of 12 and 20 MHz. Next, aspiration of the varix was performed and the rubber ring was dropped from the cardia in a proximal direction in a spiral using the EndoflexOVL ligation device with 6 or 7 ligatures. In one session, from 4 to 10 ligatures were applied. The patients were observed for 3 days in the surgical hospital; liquid food intake began the next day after the intervention. In cases of postligature bleeding, a Blackmore probe was installed in two patients, and intravasal therapy was performed once with a 3% solution of ethoxysclerol using the foamform method. Patziora's operation was performed once.
The clinical significance of the selected symptoms was determined using the alternative sequential Wald analysis method, which allows the calculation of a prognostic coefficient. When the sum of signs reached ±13, the probability of an event occurring was considered equal to 95% ( p
<0.05). Analysis of the influence of various factors on the likelihood of a ligation complication (ligature slippage) allowed us to calculate predictive coefficients for the occurrence of such complications using Wald regression analysis. The most significant clinical and biochemical indicators, as well as ultrasonographic signs (vein wall thickness, pressure in the veins of the esophagus) were assessed as risk factors for complications using a biometric method - sequential Wald analysis. Wald analysis is based on comparing the frequency (probability) distribution of symptoms in two diseases, in our case a condition without a complication and a condition with a complication. Calculations were carried out in the following sequence.
After identifying the main, most characteristic factors, their frequency was determined:
P1=S1P2=S2
n1n2,
where P1 and P2 are particulars (probability assessment) of the presence of a risk factor; S1 and S2 - number of symptoms in each group; n1 and n2 are the number of subjects examined in each group (complication group and group without complications).
The prognostic coefficient for each symptom was calculated using the formula:
PC=√10Lg P1
where PC is the prognostic coefficient, Lg is the logarithm of the ratio of particulars, which was increased 10 times for convenience of calculations.
The decision threshold was determined based on the level of acceptable errors. The collection of diagnostic information continues until any of the established thresholds are reached (+13 or –13).
The data obtained were used to identify patients with a high risk of developing postligature bleeding.
Complications of the disease
The most severe complication of varicose veins is bleeding. It can occur after overeating, during physical stress, but can also happen in a dream. Bleeding can be minor, almost imperceptible to a person, or massive, posing a threat to life. But even insignificant in volume, but regular blood loss due to illness can cause the development of chronic iron deficiency anemia. A characteristic sign of esophageal bleeding is vomiting blood.
Treatment of varicose veins of the esophagus
Treatment is primarily aimed at treating diseases that lead to increased pressure in the portal and superior vena cava system. Prevention of the occurrence or treatment of existing reflux esophagitis is also of great importance. For minor or moderate bleeding, effective treatment methods are the administration of vasoconstrictor drugs, compression of the esophageal vessels with tamponing balloons, or the use of a special probe for local cryotherapy on the damaged vessel. As well as endoscopic operations, during which electrocoagulation, application of an adhesive film or thrombin, and clamping of a bleeding vessel with hemostatic staples are performed. However, in case of massive bleeding, more radical surgical intervention is necessary. To compensate for blood loss, patients are transfused with whole blood, red blood cells and plasma replacement solutions.
results
An analysis of cases of postligature bleeding is presented in Table. 2.
Table 2. Analysis of cases of postligature bleeding
The incidence of bleeding resulting from premature slippage of the ligature (Fig. 2) was 2.59% (5 episodes per 193 endoscopic ligations). Episodes of hemorrhage occurred within 1 to 8 days after the procedure. In three patients, EGD was performed in a hospital setting immediately at the first signs of bleeding. In one case, two ligatures slipped, in 2 cases, one at a time. In 2 cases, the bleeding was so massive that it required the installation of a Blackmore probe, and in 1 of the patients the Blackmore probe was ineffective; against the background of ongoing bleeding, the patient underwent a Paciora operation. However, massive blood loss provoked the development of liver failure with a fatal outcome on the 9th day after ligation. In 1 case, it was possible to perform endoscopic sclerotherapy in the area of premature slipping of the ligature with a 3% solution of ethoxysclerol 6 ml, but in the coming days signs of bilateral polysegmental pneumonia appeared, respiratory failure increased, requiring tracheal intubation and mechanical ventilation, then sepsis developed and the patient died on the 12th day after ligation. Episodes of bleeding in 2 more patients are known from the anamnesis. In both cases, patients were hospitalized in surgical hospitals (7 and 8 days after ligation, respectively), and endoscopically revealed ulcerative defects with necrotic content in the bottom and bleeding stigmas. Drug therapy using intravenous infusion of octreotide solution at a rate of 50 mcg/h for 2 days and antibiotic therapy with broad-spectrum drugs were sufficient to stop bleeding.
Rice. 2. Premature slippage of the ligature.
Sources
- He LL., Ma JL., Jiang Y., Yang JR., Li P., Zhang Y., Wei HS. In Reply. // Ann Hepatol - 2021 - Vol21 - NNULL - p.100313; PMID:33640103
- Lee CM., Lee SS., Choi WM., Kim KM., Sung YS., Lee S., Lee SJ., Yoon JS., Suk HI. An index based on deep learning-measured spleen volume on CT for the assessment of high-risk varix in B-viral compensated cirrhosis. // Eur Radiol - 2021 - Vol31 - N5 - p.3355-3365; PMID:33128186
- Chen Y., Li X. New model predicting gastroesophageal varices and variceal hemorrhage in patients with chronic liver disease. // Ann Hepatol - 2021 - Vol21 - NNULL - p.100275; PMID:33075577
- Huang XQ., Ni LY., Jiang SY., Xia RQ., Ma LL., Wang J., Li F., Chen SY. . // Zhonghua Gan Zang Bing Za Zhi - 2021 - Vol28 - N9 - p.747-752; PMID:33053974
- Li L., Zhang SB., Zhang YN., Ding HG. . // Zhonghua Gan Zang Bing Za Zhi - 2021 - Vol28 - N9 - p.732-736; PMID:33053971
- Chen S.Y., Huang X.Q. . // Zhonghua Gan Zang Bing Za Zhi - 2021 - Vol28 - N9 - p.724-727; PMID:33053969
- Wang X., Luo X., Yang L. The use of balloon-assisted antegrade transvenous obliteration should be cautious. // Eur J Gastroenterol Hepatol - 2021 - Vol32 - N11 - p.1479; PMID:33009175
- Zheng KI., Liu C., Li J., Zhao L., Zheng MH., Wang F., Qi X. Validation of Baveno VI and expanded Baveno VI criteria to identify high-risk varices in patients with MAFLD-related compensated cirrhosis . // J Hepatol - 2021 - Vol73 - N6 - p.1571-1573; PMID:32972730
- Kolb JM., Wani S., Soetikno R., Edmundowicz SA., Hammad H. Endoscopic submucosal dissection for early esophageal and gastric neoplasia in decompensated cirrhosis with varices. // Endoscopy - 2021 - Vol53 - N4 - p.E128-E129; PMID:32757192
- Pinto C., Parra P., Magna J., Gajardo A., Berger Z., Montenegro C., Muñoz P. . // Rev Med Chil - 2021 - Vol148 - N3 - p.288-294; PMID:32730372