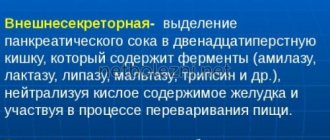
The pancreas is a unique organ of the digestive system that simultaneously performs two functions:
- endocrine – internal secretion of hormones (insulin, glucagon, somatostatin, vasoactive intestinal peptide) and pancreatic polypeptide;
- exocrine - external secretion of pancreatic juice, the basis of which are digestive enzymes.
Parenchyma (organ tissue) consists of cells and stroma, including excretory ducts and blood vessels. Normally, the parenchyma should be homogeneous (uniform).
A heterogeneous, otherwise diffusely heterogeneous structure of the pancreas indicates the presence of pathological processes, dysfunction, and possible cell necrosis.
General information
Often, when examining the gastrointestinal tract in patients, diffuse changes in the pancreatic parenchyma . Receiving such a conclusion, a person often does not understand what such a diagnosis means and whether it is necessary to take any measures to treat it. According to experts, diffuse changes in the pancreatic parenchyma indicate that the body already has prerequisites for the development of pancreatitis .
Therefore, already at the stage of receiving such a diagnosis, the patient should reconsider his lifestyle in general and his diet in particular. Most often, such changes are diagnosed in elderly people, as well as in those who suffer from pancreatitis , diabetes , liver dysfunction, and digestive tract organs. Pathology can develop as a consequence of infectious and inflammatory diseases of internal organs, in which there is a violation of metabolic processes in the body.
This article will discuss what such a diagnosis means, how this pathology manifests itself, and what treatment methods should be practiced.
Factors influencing the development of diseases
In most cases, pancreatic pathologies develop as a result of chronic pancreatitis. The disease is characterized by a progressive inflammatory process and includes several varieties, which are classified according to the causes of their occurrence.
| View | Cause |
| biliary | violation of the outflow of bile due to inflammatory diseases (cholangitis, cholecystitis), cholelithiasis |
| alcoholic | chronic alcoholism |
| destructive | structural destruction of gland cells |
| medicinal or medicinal | incorrect therapy with diuretics, cardiovascular drugs, antiviral drugs, antibiotics, statins, hormones, psychomotor and psychotropic drugs |
| parenchymal | inflammation of the parenchyma caused by impaired enzyme production |
| pseudotumorous | proliferation of connective tissue, formation of cysts and calcifications |
One of the reasons for the development of dysfunction and the formation of a diffusely heterogeneous structure of the pancreas is considered to be eating behavior: the predominance of fatty foods, smoked foods in the diet, an unhealthy addiction to confectionery, hot spices and seasonings, and abuse of alcoholic beverages. An unhealthy diet provokes a failure of metabolic processes; alcohol and its breakdown products poison the tissues and cells of the gland.
Another factor in reducing functional abilities and changing the morphological characteristics of the gland is prolonged neuropsychological stress (distress) and depressive states. Psycho-emotional instability causes hormonal disruptions that negatively affect the functioning of the entire body, including the hormone-producing pancreas.
Pathogenesis
Diffuse changes in the pancreas are not an independent diagnosis, but evidence of the development of a pathological condition and its separate symptom. This symptom is not always accompanied by an underlying disease.
The pancreas is the largest endocrine and exocrine gland. It produces pancreatic juice, performing an exocrine function. The pancreatic tissues also contain endocrine glands that produce insulin . Parenchyma is the main component in the structure of the gland. If the biochemical balance is disturbed, destruction and replacement of its tissues can occur. Consequently, when parenchyma cells are replaced, the process of normal pancreatic functioning may gradually be disrupted.
With certain disorders in the gland, along with tissue density, the echo structure , that is, the ability to reflect sounds during an ultrasound examination. Consequently, this condition is interpreted not as a disease, but as a fact that is observed on ultrasound.
How to recognize the disease?
First, the doctor collects a thorough medical history and asks about all the diseases that the patient previously had. To confirm the diagnosis on an outpatient basis, an ultrasound of the abdominal organs and coprogram is sufficient. The first study allows you to clearly examine the gland. It usually becomes smaller. On ultrasound you can see areas of compaction, cysts and other complications of necrosis. Pancreas tumors are also well detected by this method. A coprogram is a complex stool analysis that examines the presence of undigested fiber and fats in the discharge. This may indicate impaired organ function.
For more accurate and specific diagnosis, CT, MRI and biopsy are used.
Classification
According to the characteristics of the changes, the following forms of pathology are distinguished:
- Moderate diffuse changes in the pancreatic parenchyma - as a rule, this form does not lead to the appearance of unpleasant symptoms. Moderate changes are observed throughout the parenchyma and are distributed evenly.
- Diffuse changes in the pancreas like lipomatosis - with this form, the parenchyma is gradually replaced by fat cells. As long as no more than 30% of the tissue is replaced, a person does not feel any unpleasant symptoms. Replacement of the lipomatosis type occurs due to toxic lesions, chronic inflammatory processes, and injuries. Most often observed in older people with diabetes . If the pathological process progresses, then the functions of the organ are disrupted.
- Diffusely heterogeneous changes in the structure of the pancreas - such changes may be associated with the development of a number of diseases, in particular diabetes mellitus, pancreatitis. In addition, diffusely heterogeneous changes can be a consequence of edema, the formation of pseudocysts, and inflammatory processes.
Depending on the severity, the following forms of pathology are distinguished:
- Minor changes - appear as a consequence of a recent inflammatory disease, frequent stressful situations, constant errors in the diet. Such disorders may be associated with the influence of the central nervous system, since due to frequent stress, pancreatic juice is very actively secreted, and with depression its secretion is inhibited. To prevent further development of the pathology, it is necessary to adjust your lifestyle.
- Moderate changes are observed in the first stages of gastrointestinal diseases and inflammatory processes. A similar pathology can be observed in chronic pancreatitis, diseases of the gallbladder, and duodenum.
- Unexpressed changes are determined if pathological processes occur in the organ that do not affect its functions. Their appearance may be associated with elevated blood sugar levels, liver and gallbladder diseases. They may also be associated with hereditary disposition, infectious diseases, etc.
- Pronounced changes are a consequence of the pathological process. Sometimes they may be accompanied by pain and discomfort in the gastrointestinal tract.
Detection of deviations
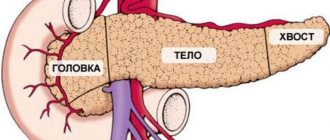
The primary methods for diagnosing pancreatic diseases are laboratory tests and ultrasound. Among the ultrasound parameters, the main ones are echogenicity (conductivity or the degree of reflection of ultrasound, indicating tissue density), contours and structure of the organ. Next, the sizes of the constituent parts of the gland (body, head, tail) are examined.
Normal indicators of an ultrasound examination of an adult
| Echogenicity | Outlines | Structure | Body | Head | Tail | Neoplasms |
| normal or isoechoic | clear | homogeneous | 2.5 cm | 3.5 cm | 3 cm | none |
Homogeneity on an ultrasound monitor is defined as a uniform gray coloration of the entire organ with a fine-grained or coarse-grained echostructure. The degree of ultrasound conductivity is determined by the presence and volume of liquid:
- isoechoicity – average, normal ultrasound reflection (gray parenchyma);
- hypoechogenicity – reduced conductivity (dark tissue);
- hyperechogenicity – increased conductivity (visualized in shades of white);
- anechoicity - ultrasound is not reflected (black parenchyma).
A diffuse-heterogeneous structure is most often characterized by hyperechogenicity of varying intensity, which indicates the development of pathological processes (inflammatory, tumor, fibrous, necrotic, etc.).
Diffusely heterogeneous changes mean a uniform violation of the homogeneity of the structure throughout the gland. Efficient parenchyma cells are gradually replaced by adipose or connective tissue that does not bear a functional load.
Ultrasound detection of a diffusely heterogeneous structure of the pancreas is not a diagnosis, but a sign of disorders indicating a particular disease. The patient may be prescribed additional diagnostic examinations (retrograde cholangiopancreatography, magnetic resonance and computed tomography).
Features of preparation for ultrasound
To objectively identify structural changes in the pancreas before performing an ultrasound, the patient must:
- 2-3 days before the examination, avoid alcohol-containing drinks and foods that cause intense gas formation (legume dishes, cabbage, fermented milk drinks, baked goods);
- the day before the procedure, start taking carminative drugs (Espumizan, activated carbon).
The fasting regime before an ultrasound of the abdominal organs is 8-12 hours.
Causes
Diffuse changes can occur due to various reasons. The reasons that provoke the development of such a pathology may be:
- Metabolic-dystrophic processes.
- Circulatory disorders.
- Metabolic disorders.
- Endocrine diseases ( diabetes , etc.).
- Functional disorders of the biliary tract and liver.
- Diseases of the gastrointestinal tract.
The development of such changes can be provoked by the following factors:
- Poor nutrition – excessive amounts of spicy, sweet, starchy, salty, fatty foods in the diet.
- Constant stress.
- Hereditary disposition.
- Alcohol abuse, smoking.
- Irrational use of medicines.
Reasons for changes
Changes in the structure of the pancreas against the background of hyperechogenicity accompany acute inflammation, edema, fibrosis, and fatty deposits. The main diseases diagnosed based on the results of an ultrasound examination:
What does an ultrasound of the pancreas show?
- an increase in the volume of intracellular fat and replacement of parenchyma with adipose tissue - steatosis;
- accumulation of fluid (edema) is not an independent pathology, but a consequence of diseases of the gland itself, the duodenum, hepatitis, helminthic infestations, stones in the gall bladder, etc.;
- benign tumors (gastrinoma, insulinoma, glucagonoma);
- proliferation of atypical cells – pancreatic cancer;
- acute and chronic inflammation of the organ - pancreatitis;
- synchronous inflammatory damage to adjacent organs of the hepatobiliary system (pancreas and gallbladder) - cholecystopancreatitis;
- motor-tonic dysfunction of the gallbladder and bile duct sphincters - biliary dyskinesia;
- death of gland cells - pancreatic necrosis;
- diabetes mellitus (insulin-dependent type 1 with hereditary predisposition);
- proliferation of connective tissue and replacement of its working cells – fibrosis;
- pancreolithiasis - the presence of calcifications (calculi) in the ducts and parenchyma of the organ;
- a cavity in the parenchyma, devoid of epithelial lining and containing pancreatic secretion - a false cyst (pseudocyst), may not be single;
- poor circulation in the gland due to chronic venous stagnation;
- disruption of the blood supply to the organ due to pathologies of the splenic and gastric arteries;
- increased hydrostatic pressure in the portal vein – portal hypertension.
A separate genetic disease is cystic fibrosis, in which the pancreatic secretion has a too thick consistency that blocks the ducts. Pancreatic juice does not enter the intestines, enzyme deficiency leads to digestive disorders and lack of nutrients.
As well as rare congenital pathologies: Shwachman-Diamond syndrome and Johanson-Blizzard syndrome, characterized by secretory pancreatic insufficiency in combination with bone marrow dysfunction.
Temporary structural changes provoke:
- overeating and drinking alcoholic beverages;
- acute infectious and inflammatory diseases not related to the pancreas (influenza, ARVI, intestinal infections, pneumonia, etc.);
- side effects of antibiotics, statins and other medications;
- sudden nervous shock.
The non-pathological cause of the moderately diffuse-heterogeneous structure and increased echogenicity is old age. As the body ages, all organs and systems of the body undergo pathological changes.
Symptoms
As a rule, signs of diffuse changes in the pancreas depend on the underlying disease, which provoked the development of such signs. However, most often with such changes their signs are detected on ultrasound. The following echographic signs of diffuse changes in the gland are distinguished:
- Heterogeneous texture of the pancreas due to changes in echogenicity in some areas.
- Bile ducts are unevenly enlarged.
- Unevenly increased echogenicity.
- The volume of the gland has changed.
- Additional echo signs may also be detected - cysts, pseudocysts.
With such pathological changes, the following symptoms may appear:
- Feeling of heaviness under the right rib.
- Pain in the hypochondrium.
- Constant feeling of nausea, feeling of heaviness in the stomach.
- Decreased appetite.
- Heartburn , bitter belching.
- Constipation or diarrhea.
- Feeling of weakness, decreased ability to work.
- Headache.
Depending on the diseases in which this pathology develops, other symptoms may be observed. Thus, in acute pancreatitis, intoxication of the body tachycardia develops blood pressure decreases . There is severe pain in the hypochondrium. With chronic pancreatitis, the symptoms are less pronounced.
However, very often diffuse changes in the pancreas do not cause concern, and symptoms of the condition do not appear.
Clinical picture - symptoms
As a rule, age-related changes in the gland are not as noticeable as dystrophy after pancreatitis. The first symptoms of a violation of external function are indigestion. The patient's appetite worsens, bloating appears after eating, and stool changes (diarrhea alternates with constipation). Sometimes undigested fiber and fat appear in the stool. Patients who have such changes in the pancreas have a characteristic appearance - they are pale, emaciated, with dry skin and poorly developed muscles.
Symptoms of a violation of the endocrine (internal) function of the gland are as follows: the patient develops a constant feeling of thirst, itchy skin and decreased immunity. Wounds and small cracks in the skin heal very poorly. The covers themselves are very thin and lack moisture. The patient suffers from polyuria - frequent, profuse urination. These are symptoms of diabetes mellitus, which develops in response to the destruction of the islets of Langerhans. Usually other endocrine functions are also affected, but this has little effect on the clinic.
Tests and diagnostics
Diffuse changes in the pancreatic parenchyma are determined during ultrasound examination. However, to establish the reason why diffuse changes appear, it is necessary to conduct the following additional studies:
- Laboratory tests - general and biochemical blood tests.
- Endoscopic examination - allows you to determine the condition of the excretory duct of the gland.
- X-ray – can be performed as an additional study.
- CT or MRI.
Other studies may also be performed, which are prescribed depending on the disease and condition of the patient.
The main symptoms of the inflammatory process
The symptoms of pancreatitis most often manifest themselves when diffusely heterogeneous changes in the structure of the organ are clearly defined and echogenicity is increased. The main manifestations include:
- heaviness in the epigastric (epigastric) region, nausea, vomiting;
- severe pain syndrome;
- subfebrile (37-38℃) body temperature;
- dyspepsia (painful and difficult digestion);
- intense gas formation;
- constipation (constipation), alternating with diarrhea (diarrhea);
- dry mouth, heartburn.
External symptoms include yellowness of the eyeballs, pallor, loss of body weight, and bloating.
Clinical signs - deviations in test results:
- Complete blood count: decreased hemoglobin and red blood cells, increased ESR, leukocytosis (significant increase in white blood cells).
- Blood biochemistry: high levels of enzymes (amylase, phospholipase, lipase), increased bilirubin, glucose, urea, decreased amount of total protein and protein fractions.
- Coprogram (stool analysis): steatorrhea - excess fat, the presence of undigested food fragments, increased elastase levels.
- Urinalysis: amylasuria (increased amylase), proteinuria (presence of protein), dark color.
When analyzing insulin, elevated levels of the hormone are recorded.
Treatment with folk remedies
If a patient experiences unpleasant symptoms, some traditional methods of treatment can be practiced to improve the condition. However, you must first coordinate the use of such methods with your doctor.
- Honey with pumpkin . Carefully remove seeds from a small pumpkin and fill with honey. Leave in a dark place for 20 days. Drink liquid from pumpkin three times a day, 1 tbsp. spoon.
- Oat infusion . Pour 500 g of oats into 1 liter of boiling water and leave for an hour. Strain and drink half a glass of the product three times a day.
- Lemon remedy . Grind 1 kg of lemons with peel in a meat grinder (remove the seeds first), 300 g of garlic and 300 g of parsley. Mix everything and place in a glass jar. Store in the refrigerator and consume 3 tsp. in a day.
- Herbal mixture . Mix lingonberry, blueberry, strawberry leaves, as well as corn silk and bean pods in equal proportions. 2 tbsp. l. Place the mixture in a thermos and pour 300 ml of boiling water. Leave for 1 hour, drink throughout the day.
- Potato juice . Grate two medium potatoes and squeeze out the juice. Drink half a glass twice a day.
- Kefir and buckwheat . Grind the buckwheat in a coffee grinder and pour in 1 tbsp in the evening. such flour with 1 glass of kefir. Drink in the morning on an empty stomach.
- Lingonberry tincture . Pour 500 ml of water over lingonberry leaves (2 tablespoons of raw material) and boil for 20 minutes. Drink 250 ml of the product twice a day.
Prevention
To prevent the development of diffuse changes in the pancreas, it is necessary to follow the following rules of prevention:
- Get rid of bad habits - do not abuse alcohol, do not smoke.
- Drink herbal teas instead of regular teas. A specialist will help you choose the right herbs. You can also buy special preventive teas at the pharmacy.
- Eat rationally and properly, removing all harmful foods from the menu. Maintain moderation in food. You need to eat often and in small portions.
- If you experience unpleasant symptoms indicating problems with the gastrointestinal tract, immediately visit a doctor and undergo the prescribed examinations.
- Sleep at least 8 hours a day.
- Avoid stressful situations.
Diet
Diet for diffuse changes in the pancreas
- Efficacy: therapeutic effect after 14-21 days
- Terms: 1-6 months/permanently
- Cost of products: 1600-1700 rubles. in Week
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
If you have problems with the pancreas, it is recommended to follow the Table No. 5 . In addition, nutrition may vary depending on the disease that caused problems with the pancreas.
The following products must be entered into the menu:
- lean fish and meat;
- dairy and fermented milk products;
- porridges from various cereals;
- vegetable dishes;
- fruits;
- grain products.
The diet should be low-calorie, meals should be fractional. It is also important to give up processed foods and sausages. Products need to be boiled, baked, steamed.
You should strictly avoid eating fried and smoked foods, canned food, sour and spicy foods. It is necessary to completely give up alcohol. It is also important to give up sweets and sweet fruits. The amount of salt in seasonings should be kept to a minimum.
List of sources
- Gubergrits N. B., Linevskaya K. Yu., Belyaeva N. V. Differential diagnosis in gastroenterology. From symptom and syndrome to diagnosis and treatment: practical work. hands - Kyiv: Trush E. N. [ed.], 2021. - 623 p.
- Danilov M.V., Fedorov V.D. Pancreatic surgery. Guide for doctors. M.:b Medicine, 1995. 312 p.
- Zakharova O.P., Egorov V.I., Karmazanovsky G.G. Surgical treatment of pancreatic tumors: computed tomographic criteria for resectability. Annals of surgical hepatology. 2011. 16. No. 1. pp. 84-91.
- Zimmerman Ya.S. Chronic pancreatitis // Bulletin of the Pancreatology Club. - 2009. No. 1. - P. 38-47.