Principle of ultrasound examination
A special device that creates ultrasonic waves scans the internal organs in the selected area and sends the received information to the monitor in the form of an image. So, with the help of sound, you can “see” the structure of the internal organ, the composition of its tissues and possible pathologies.
A special gel is applied to the abdominal area, along which the doctor moves a sound sensor. The patient feels the sensor sliding across the body, as well as slight pressure on certain parts of the abdominal area. The procedure is carried out with a deep breath. A sinographic examination takes about 10-15 minutes. It is absolutely harmless and painless.
The accuracy of the results of this examination largely depends on how the ultrasound of the pancreas is performed: on an empty stomach or not?
Advantages and disadvantages of the method
The main advantages of the method are absolute safety, ease of implementation, accessibility and high information content. Ultrasound of the pancreas can be performed in almost any multidisciplinary clinic, but it is important that it is performed on a modern scanner by a qualified specialist.
Due to the high safety profile, the study can be performed as many times as required by a particular patient. There are no contraindications to its use, with the exception of an open wound in the abdominal area.
Why is ultrasound of the pancreas performed on an empty stomach?
For ultrasound to show the most accurate results, it is not recommended to eat for 12 hours before the ultrasound. The procedure should be performed on an empty stomach. Eating food provokes gas formation, which interferes with high-quality visualization of organs. In addition, food debris in the intestines distorts the overall picture. As a result, the diagnostician may make erroneous conclusions or may need to repeat the study after preliminary preparation.
In addition, on the day of the examination, the patient is prohibited from smoking, taking medications and drinking alcoholic beverages. Even drinking plain water is prohibited for 6 hours before the session.
If the patient has a tendency to increased gas formation, the day before the procedure, he is prescribed adsorbents - medications that reduce gas formation in the intestines.
Application to diseases
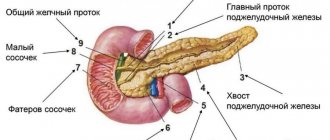
The generally accepted size of the pancreatic duct on ultrasound is less than 2 mm, and in the head - up to 3 mm.
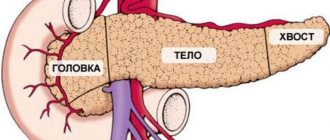
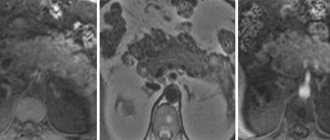
The size does increase with age, and the duct becomes dilated in patients with gallstones. In acute pancreatitis, the duct also increases to 3 mm and decreases in size as the patient's condition improves. A dilated duct is usually a sign of obstruction due to pancreatitis or carcinoma. Likewise, once disease occurs, the disease cannot be contained within the pancreas. Exudate or malignant neoplasms come out early in the natural course of the disease. Chronic pancreatitis Chronic pancreatitis is a chronic inflammation of the pancreas tissue, leading to fibrosis, loss of exocrine tissue, and hence gland dysfunction. For the pancreas to lose exocrine function, more than 90% of the exocrine tissue must be lost. Then symptoms of fat malabsorption and steatorrhea appear, preceded by protein malabsorption and creatorrhoea. Malabsorption of carbohydrates occurs only when the secretion of enzymes is almost completely inhibited. In contrast, patients with malabsorption syndrome due to pathology of the small intestine have a small volume of stool, since the absorption of water and electrolytes is preserved. Vitamin B12 deficiency may occur because pancreatic proteases are required to break down the B12 complex and R protein. Only after this does vitamin B12 bind to the Castle factor and can be absorbed. Chronic calcific pancreatitis accounts for 80% of all cases of chronic pancreatitis. pancreatitis that occurs against the background of alcoholism. It is characterized by the formation of protein plugs or stones in the ducts. Stenosis and atrophy of the pancreatic ducts may also be observed. Chr. Obstructive pancreatitis occurs against the background of obstruction of the duct or papilla of Vater by a tumor or stricture. Chr. Inflammatory pancreatitis is a rare form, the etiology is not completely clear. The first attack of pain is at the age of 30-40 years; attacks are repeated in the next two years. The frequency of attacks increases, and finally a syndrome is formed. pain syndrome, malabsorption syndrome, diarrhea. Calcifications form in the tissue, which can be detected on a plain X-ray of the abdominal cavity. In chronic pancreatitis with abdominal pain, the levels of lipase and amylase in the blood are normal. Or the atrophy is such that the gland does not contain a sufficient amount of exocrine tissue. Either due to pronounced fibrotic changes, the glands prevent the entry of enzymes into the blood. This occurs in diseases of the pancreas, for example, chronic pancreatitis. The patient would have felt unwell, steatorrhea, fat intolerance, abdominal pain, bloating and flatulence. The incidence of type II diabetes increases with age due to the loss of insulin-secreting beta cells. Obstruction of the duct will lead to atrophy of the gland, associated with a stone in the duct, a neoplasm on the neck and head. In chronic pancreatitis - contour irregularities and expansion of the main duct and side branches. Lateral branches are usually not visible; if they are visualized indirectly, they are expanded. In severe cases, there is a sharp expansion of the lateral branches, resulting in a “chain of lakes.” Other signs of chronic pancreatitis include stricture formation and intraductal stones. General loss of gland volume is usually caused by aging, chronic pancreatitis, or a blocked duct. Diffuse enlargement of the gland is rare and is caused by acute pancreatitis, lymphoma and metastases. The relative degree of swelling and enlargement of the pancreas in severe pancreatitis is minimal. This is due to the fact that in the pancreas, fluid leaks into the surrounding tissues - peripancreatic effusion. The retroperitoneal organ surrounded by gas from the small and large intestine of the pancreas is often not optimally visible on ultrasound. With pancreatitis, obstruction of the small intestine leads to gasification of the intestine, poor visibility of the pancreas. Filling the stomach with water sometimes helps during examinations because it improves ultrasound transmission. The tail of the pancreas can be seen and the spleen is used as a visualization window. CT is much better suited for obtaining consistent images of the retroperitoneum. The presence of the disease is sometimes judged only by thickening of Gerota's fascia or lateral conical fascia on CT. Pancreatic adenocarcinoma is usually a rapidly fatal disease. The few lucky enough to survive the disease were diagnosed at an early stage. It is important that routine assessment of the pancreas focuses on subtle changes in shape and texture. In cystic fibrosis, the juice thickens significantly and forms stones. Can eventually become impacted, restricting upstream flow and causing a blockage. When narrowing from pancreatitis or carcinoma, the flow is also obstructed. The upstream portion of the duct will be dilated and the downstream portion will be decompressed. The most difficult problem is identifying early asymptomatic pancreatic carcinoma. Shape deformation and pattern deviation are key issues to pay attention to. Ductal acinar carcinoma is the most common form of carcinoma. An important characteristic is that it has poor blood supply and is a hypovascular mass. The body and tail are easy to identify, but the head and uncinate processes show normal heterogeneity. There are tumors that have fooled the most experienced observers because they are exophytic. The development of adenocarcinoma from the exocrine part is more likely, since it dominates in terms of pure volume. It has been said that 98% of the cellular volume of the pancreas is exocrine and 2% endocrine. Adenocarcinoma of the exocrine part is much more common than tumors of islet origin. Exocrine adenocarcinoma exhibits a characteristic desmoplastic (fibrotic) response. Leads to blockage of ducts, arteries, veins and lymphatic vessels and has important clinical significance. Vascularization distinguishes endocrine from exocrine pancreatic tumors. The endocrine system is closely related to the vascular system, and these tumors are hypervascular. They also tend to be large at the time of discovery because they remain asymptomatic for a long time. Because the islets are larger in the tail, endocrine tumors are more common in the tail. Exocrine tumors are the most common forms of cancer. They are hypovascular and exhibit a characteristic fibroblastic reaction. Damage to the bile ducts, pancreatic ducts, arteries, veins and nerves is not uncommon. Bile duct strictures cause jaundice, and nerve damage causes pain. Damage to blood vessels usually has no clinical correlation, but has prognostic significance. Due to fibroblastic changes and strictures, exocrine adenocarcinomas appear when the tumor is small. Despite this, the prognosis for this tumor is grim. Take care of yourself, Your Diagnosticer !
Tags: lectures pancreas ultrasound
How to prepare for an ultrasound?
The main goal of preparing for an ultrasound examination is to eliminate gas formation and irritation on the mucous membranes. Three days before the ultrasound, the patient is prescribed a gentle diet. Excluded from the diet: fruits, carbonated drinks, raw vegetables, dairy products, sweet juices, legumes, beer and other foods that cause flatulence. A sample menu for the next three days before the ultrasound consists of:
- boiled beef;
- boiled eggs;
- skinless chicken;
- steamed lean fish;
- porridge - oatmeal, barley, buckwheat.
Eating should be done in a calm environment. To avoid swallowing air, it is not recommended to talk or rush while eating. You should eat in crushed portions and preferably at three-hour intervals. You need to have dinner no later than 20:00. You cannot drink food with water. Food diluted with liquid is poorly absorbed, since the digestion process in the gastrointestinal tract is disrupted. You are allowed to drink unsweetened tea an hour before meals or 40 minutes after meals.
If necessary, 12 hours before the ultrasound session, you should clean your intestines in advance. This can be done with an enema or taking laxative medications. It is not recommended to use breath fresheners or chewing gum immediately before the session. Failure to comply with any of the requirements must be reported to the diagnostician, otherwise the resulting image may be misinterpreted.
Cases of exceptions in performing ultrasound
There are times when the pancreas is difficult to detect. In such situations, the stomach must be filled with liquid. Use still water at room temperature. The patient drinks it through a thin tube in small sips.
Sometimes an exception may be diabetes mellitus or decreased glucose tolerance. Patients with diabetes should not deny themselves food for too long. He can have breakfast in the morning before the session. However, breakfast should consist of carbohydrates. Boiled water or any other liquid should be excluded on the day of the ultrasound.
Only in emergency situations can a diagnostician decide to conduct an ultrasound examination of the pancreas without prior preparation. However, the informative reliability of the studies is reduced to 40%.
The medical specialist provides a detailed transcript of the research materials in writing, attaching photographs of the examined organ to the document.