Ultrasound of the pancreas
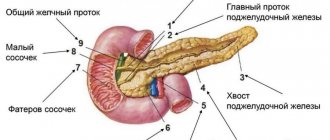
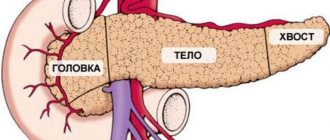
The pancreas is located behind the stomach and is quite tightly adjacent to the duodenum. It consists of a head, body and tail. This organ of the digestive system promotes the release of enzymes for the breakdown of proteins, fats and carbohydrates. The pancreas also produces insulin, which is necessary to regulate blood sugar. Ultrasound is a diagnostic method
, based on ultrasonic waves, allows you to identify various abnormalities and pathologies of internal organs, including the pancreas.
Types of changes
All changes in the pancreas may have different ultrasound signs, depending on different reasons. Most often, doctors use ultrasound to detect differences that occur during dystrophic or metabolic changes in the organ. This happens when there is poor circulation, dysfunction of the bile ducts, etc.
A diffusely heterogeneous structure can also be detected with age-related changes in the pancreas. The organ decreases in size, and part of it is replaced by connective and fatty tissue. Let's consider the types of changes in the structure of the pancreas.
Echogenicity increased slightly and significantly
A change in the permeability of organ tissue may indicate the development of pathology. But often it can show the normal functioning of the organ.
If there are areas of high echogenicity, this is always a sign of a pathological condition of the gland. There are no hypoechoic foci.
Moderately increased echogenicity indicates that altered objects can be detected in the gland:
- Pseudocysts. These are formations that have liquid inside. Develop after acute inflammation. The outline becomes unclear and sometimes has jagged edges. There is a general increase in echogenicity.
- The presence of a cystic-solid structure is noted if there is no fluid in the detected formations.
- Areas of calcification. They are also called calcifications. They are formed as a result of an inflammatory disease, and also occur with chronic degenerative changes in the organ.
- Presence of areas with adipose tissue. Fatty degeneration of the structure is observed due to an increase in body weight as a result of obesity and if the patient consumes a lot of fatty foods. Often such changes occur when a person abuses alcoholic beverages.
- Fibrous areas appear where normal cells are no longer present as they are replaced by connective tissue. Most often, areas of fibrosis develop with pancreatic necrosis. The heterogeneity of the structure is characteristic.
- Presence of stones in the ducts.
- Degeneration of pancreatic tissue. It is the outcome of chronic pancreatitis in an advanced stage.
- Tumors that appeared as a result of the spread of metastases.
Moderately increased echogenicity indicates that altered objects such as tumors can be found in the gland.
High echogenicity
Disturbance and a sharp increase in the echogenicity of the gland structure indicates that an acute inflammatory process is developing in it. Such a patient requires urgent treatment in a surgical hospital. Acute inflammation of the gland is a life-threatening condition.
A sharply increased hyperechogenicity may also indicate an active fibrotic process in the tissues. This means that normal pancreatic tissue is quickly replaced by connective tissue.
Severe hyperechogenicity is also diagnosed in diabetes, especially the insulin-dependent type, as well as in elderly patients. Portal hypertension leads to pronounced changes in ultrasound signs, i.e. increased pressure in the portal vein. This condition often results in significantly increased echogenicity.
Preparation rules
In case of improper preparation, the information content of the study can be reduced by up to forty percent. Therefore, the preparation stage must be approached extremely responsibly and strictly follow all the doctor’s instructions.
On the eve of the study, dinner should be as light as possible, since the procedure is carried out strictly on an empty stomach.
Due to the accumulation of gases in the intestines, the pancreas may be difficult to see. In this regard, three days before the examination, it is necessary to switch to a gentle diet, namely, exclude gas-forming foods from the diet: milk, yeast bread, raw vegetables and fruits.
Directly on the day of the procedure, you should not smoke, drink alcohol or take medications. The doctor will warn you in advance about the need to take laxatives or anti-flatulence medications.
Prevention
To prevent changes in the structure of the pancreas, it is necessary:
- Healthy food;
- avoid overeating and snacking on the go;
- avoid combining fatty foods with alcohol;
- Avoid eating large meals before bed;
- quit smoking;
- eliminate alcohol abuse;
- exercise;
- do not consume foods that are dangerous to the structure of the gland: pickles, marinades, fried foods, smoked foods.
The gastroenterologist will give clear recommendations on nutrition and proper therapy.
How is an ultrasound of the pancreas performed?
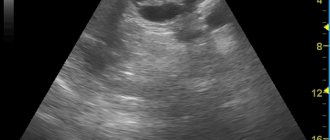
Ultrasound of the pancreas is an absolutely painless and safe procedure. It is performed transabdominally. The patient lies with his back on the couch. The doctor lubricates the area being examined and the transmitting sensor with a special gel for better conductivity of ultrasonic waves. During the procedure, the patient will need to turn over to the left and then to the right side. An ultrasound scanner, which the doctor moves over the skin, transmits images to the monitor of the ultrasound diagnostic apparatus, from which the shape and structure of the pancreas, its location and size can be determined. The whole procedure takes no more than 15 minutes. As a rule, other nearby abdominal organs are examined along with the pancreas: liver, stomach and gall bladder.
What is echostructure and echogenicity
Echogenicity and echostructure are decisive in the diagnosis of diseases of the pancreas and other organs and are used to describe the structure of the objects being studied.
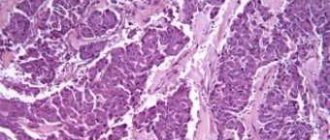
Normally, the gland tissue is homogeneous and of equal density. Often the echogenicity of an organ can be determined subjectively, i.e. based on the doctor's experience. This is due to the fact that in medical practice there are different examples of measuring ultrasound characteristics of the tissues in question. Novice specialists can evaluate the structure of the object being studied and its structure based on the scale.
Types of echogenicity:
- anechoicity (it is visualized as a black object);
- hypoechogenicity (the object in question will be dark gray);
- isoechoicity (this is the normal state of the organ, and it will be visible on the monitor as a light gray object);
- hyperechogenicity (the object will be white).
The degree of echogenicity depends on the acoustic properties of the tissue. The less fluid, the higher the echogenicity, and vice versa. Accordingly, anechoic objects are those that do not have fluid. Hyperechoic objects contain the largest amount of fluid.
[morkovin_vg video=”ptUJcUKCvpw;EtOHdKfvFMc”]
Based on the nature of the structure, a distinction is made between homogeneity (i.e. objects are colored uniformly) and heterogeneity (the organ in the image is colored non-uniformly).
Decoding the result
The results of the examination are issued immediately after its completion. The study protocol fully describes the structure of the organ, size, presence/absence of various formations. In case of obvious deviations from the norm, the uzist makes a diagnosis, which, in his opinion, characterizes the data obtained. However, the final conclusion is made by the doctor who gave the referral for ultrasound diagnostics.
. The norms for the size of the pancreas in adults according to ultrasound are as follows:
- overall size – 16-24 cm;
- body of the gland – 21-25 mm;
- head width – 32-35 mm
- the thickness of the Wirsong duct is 1.5-2 mm.
What is echogenicity
Echogenicity is a sign system used by uzologists, which allows one to establish the correspondence of the anatomy of organs to the level of reflection and absorption of high-frequency waves. Liquid tissue of the pancreas is characterized by an average echogenicity. The echo density of the liver parenchyma is used as a standard sample.
Echogenicity scale for assessing study results
Using ultrasound, you can not only determine the degree to which internal organs perceive high-frequency waves, but also obtain information about other equally important parameters. During the examination of the gland, the following parameters are carefully studied:
- Size.
- Form.
- Structure.
- Circuit.
When determining the volume of the pancreas, the length of the head, body and tail is calculated. Ideally, they should not exceed 30, 24 and 25 mm, respectively. An increase in the latter indicates local or general inflammation in the organ.
Abnormally large sizes are a typical sign of pancreatitis. Causes of increased size can also be: abdominal trauma, cystic fibrosis, biliary dyskinesia, hepatitis, infectious diseases.
Local changes are associated with malignant tumors and cysts.
In appearance, the digestive gland resembles a comma and has an oblong shape. Sometimes there is a thickening in the head area. Ring-shaped, additional, split forms are deviations from the norm. Improper development of the organs of the digestive system is associated with disturbances in the processes of embryogenesis.
Healthy pancreas. The dark longitudinal stripe is the hypoechoic shadow of the duct.
As for the external contours, they must be clearly defined in the longitudinal and cross sections. Blurring of any part of the gland may indicate the development of an inflammatory process.
Blurred outlines and swelling also cause diseases of the organs adjacent to the pancreas (stomach and duodenal ulcers). Uneven borders are created by tumors, cysts, and stones.
The contours of malignant formations are lumpy and blurry.
The structure of the digestive gland should be homogeneous and fine-grained. Having discovered single fatty inclusions or numerous calcifications and pseudocysts in the organ, the doctor has every reason to suspect fibrolipomatosis and chronic pancreatitis in the patient.
Insufficient preparation of the person himself can lead to errors in research results. Three days before the procedure, the patient must adhere to a diet that eliminates the possibility of increased gas formation. For prevention, patients are recommended to take adsorbents. On the day of the procedure, it is advisable to empty your bowels and limit your food intake.
What are diffuse changes in the pancreas
Video: Increased echogenicity of the pancreas: signs
What does increased echogenicity mean?
An unusual increase in the recoil force of the waves indicates compaction of the parenchyma and a reduction in the amount of fluid in it. Diffuse hyperechogenicity, the causes of which are external factors, is not considered a pathology. Most often it manifests itself in the hot season, after eating hot and rich food, and during colds.
Echogenicity increases markedly with inflammation. Causes for concern may be: tumors, metastases, calcium deposits and stones, cysts, fibrosis. Such inclusions are the consequences of ignoring the early symptoms of pancreatitis.
A number of parameters indicate acute pancreatitis:
- General increase in organ size.
- Presence of large echogenic areas.
- Heterogeneity of structure.
- Exceeding the width of the gland duct.
- Blurred boundaries.
A more severe form of the disease involves changes in the density and contours of neighboring organs. Possible formation of pseudocysts.
When diagnosing chronic pancreatitis, the following picture is observed:
- Echogenicity increases slightly.
- The width of the duct increases by more than 2 mm.
- The size of the gland itself increases.
- Unclear outline.
- Heterogeneous structure.
- There is fluid in the omental bursa behind the stomach.
The disease may be accompanied by the formation of stones. In the picture they appear as spots with an echogenic trace. The progressive disease is easy to notice due to the significant discrepancy in the ratio of the size of the gland to the Wirsung duct. The latter is greatly swollen in width.
Parameters such as increased echogenicity and blurred contours suggest that healthy cells in the organ have replaced fat cells, which occurs with lipomatosis. Hyperechogenicity along with a decrease in the pancreas indicate the development of fibrosis. The growth of connective tissue and its replacement of normal cells is accompanied by the appearance of scars.
Ultrasound alone is not enough to accurately diagnose a patient. The patient is sent for auxiliary procedures: magnetic resonance or computed tomography, laparoscopy or biopsy.
A lighter image of the pancreas indicates increased echogenicity
Heterogeneity of structure
In a healthy person, pancreatic tissue is homogeneous, fine-grained, and homogeneous. The echostructure suspiciously increases in subacute and chronic pancreatitis, cysts and tumors.
Acute interstitial pancreatitis is often diagnosed in people who abuse alcoholic beverages and high-fat foods. On palpation they feel sharp pain. Unpleasant symptoms are associated with swelling of the gland. A person complains of cramps in the upper abdomen may contact a doctor.
The heterogeneity of the structure is indicated by arrows (white and dark areas).
Severe pain in the left or right hypochondrium occurs with chronic pancreatitis. During periods of exacerbation of the disease, the patient experiences an increase in temperature, abnormal blood pressure, changes in the color of the skin and sclera (jaundice). The patient is worried about constant nausea, vomiting, and lack of appetite. In addition to poor nutrition, the following diseases can affect the development of pancreatitis:
- Cholecystolithiasis.
- Ulcer penetration.
- Viral hepatitis.
- Parasites (worms).
- Typhoid and typhus.
- Alcohol abuse.
There are many lovers of alcoholic beverages among men, so the likelihood of chronic pancreatitis in the stronger half of humanity is much higher than in women.
Heterogeneity of structure in children
Changes in the homogeneity of the structure of the pancreas often occur in childhood. They manifest themselves as disruptions in the functioning of the gastrointestinal tract. Disturbances occur due to spasms of the gland ducts and increased enzyme activity. The obstructed outflow of the latter causes swelling of the pancreas in the child.
How to treat the pancreas with folk remedies
This form of the disease occurs even in children 1 year of age. Parents who do not follow the schedule for introducing complementary foods (early inclusion of meat and fish dishes in the menu) can be blamed for this.
Why deviations are dangerous
Negligence towards pancreatitis can increase the risk of new foci of inflammation. The combination of diseases affects the overall health of a person. A critical manifestation of complications is disability.
If treatment of the disease is not started at its early stage, pancreatic enzymes enter the blood and create conditions for infection of other organs. Several diseases find a corresponding response:
- Liver and kidney failure.
- Bleeding in the stomach and intestines, erosions, ulcers.
- DIC syndrome (blood clotting disorder).
- Purulent-necrotic parapancreatitis.
- Mechanical jaundice.
- Liver hepatosis.
- Cholangitis, cholecystitis.
- Abdominal abscess.
Necrosis of the gland parenchyma develops tumors and cysts. Malignant tumors often appear in older men. Unusual thinness, loss of appetite, abdominal pain are the main symptoms of the disease. Only adequate timely therapy can reduce the chances of such complications occurring.
Video: Complication of chronic pancreatitis
How to treat
A gastroenterologist can give a specific definition of the term “increased echogenicity.” To begin with, he will make sure that the ultrasound data is accurate and will exclude the manifestation of a diffusely heterogeneous structure of the gland.
What does an ultrasound of the pancreas show?
Ultrasound of the pancreas shows:
- tissue structure;
- size, shape and contours of the gland;
- location of the gland.
The doctor will also see the following pathologists:
- various neoplasms (cysts, pseudocysts, tumors);
- change in the density of the gland structure;
- inflammatory and infectious processes;
- injuries.
Pancreas thickening on ultrasound
Compaction of the pancreas is not a disease, but a consequence of inflammatory processes occurring in this place. The cause is usually a dystrophic change in tissue and structure, which occurs with chronic endocrine diseases and circulatory disorders.
White pancreas on ultrasound
The white pancreas on ultrasound is detected during an acute inflammatory process - acute pancreatitis. The white color in this case is due to low echogenicity due to the fact that the outflow of enzymes is impaired, blood circulation stagnates and the size of the organ increases. Also, a light or white pancreas is recorded with the development of a disease such as lipomatosis. It occurs most often in older people and obese people. In this case, normal gland tissue is replaced by fatty tissue, the size of the organ increases, due to which the echogenicity also increases, which is recorded on the monitor of the ultrasound machine as a white or light spot.
Is pancreatic cancer visible on ultrasound?
Ultrasound of the pancreas can detect malignant tumors.
- If the doctor sees on the monitor a formation that is well defined and, unlike the pancreas itself, has a clear outline.
- If the lymph nodes located nearby are enlarged.
- The person also complains of sudden weight loss, yellowness of the mucous membranes and skin, vomiting that does not bring relief, and nausea.
In this case, there is a high probability that the formation is of an oncological nature.
What does a decrease in echo density mean: table of pathologies
A hypoechoic node can be found in many organs and does not always turn out to be a pathology. Let's take a closer look at what a formation with reduced echogenicity is in various organs, and what preliminary diagnosis can be made.
| Organ | Features of the ultrasound image | What could it indicate? |
Thyroid | Hypoechoic node | Cyst |
| Fluid formation | ||
| Vascular formation | ||
| Oncology (in 5% of cases) | ||
Uterus | Hypoechoic structure with a fuzzy shape, M-echo indicators are increased, the uterine cavity is expanded, heterogeneous endometrial structure | Carcinoma |
| Hypoechoic zone with internal echo structure | Inflammatory process | |
| An area on the wall of an organ with reduced echogenicity | Myoma | |
| Hypoechoic zone near the fertilized egg | Accumulation of blood under the embryo - an incipient miscarriage | |
Mammary gland | A formation that is heterogeneous in structure with reduced echo density, with a fuzzy and uneven contour, gives a shadow | Carcinoma |
| Hypoechoic formation (often irregular in shape) with unclear contours and boundaries | Adenosis | |
| Round hypoechoic inclusion with unclear contours | Typical cyst | |
| Formation with reduced echo density, thickened walls, internal growths and calcifications | Abnormal cyst | |
| Hypoechoic formation with smooth and clear contours | Fibroadenoma (similar to a malignant tumor) | |
Ovaries | Areas with reduced echo density | Follicle |
| Vascular formation | ||
| Corpus luteum | ||
| Cyst | ||
| Oncology (rather rare) | ||
| Heterogeneous structure of the organ during childbearing age and homogeneous during menopause | Normal, not pathological | |
Kidneys | Hypoechoic area with clear boundaries and homogeneous structure | Cyst |
| A formation of heterogeneous structure with reduced echogenicity and unclear contours | Tumor | |
| Hypoechoic formation, retroperitoneal lymph nodes are enlarged, blood flow is not visualized | Oncology | |
Pancreas | Hypoechoic formation with unclear contours, which does not occupy all the tissue of the organ | Metastases |
| A homogeneous formation with low echo density and a smooth contour, without inclusions | Cyst | |
| Several hypoechoic areas | Fibrolipomatous process | |
| Hemorrhagic pancreatitis | ||
| Hypoechoic formation with thin peripheral outgrowths, increased size of the gland, displacement of its large vessels, blood flow is not visualized | Gland cancer | |
Liver | Hypoechoic formations near the portal vein or gallbladder bed, often have a triangular or oval shape | Residual areas of normal tissue against the background of liver steatosis (accumulation of fat in the cells of the organ) |
| Hypoechoic round nodes, possible tuberosity along the periphery | Cirrhosis | |
| Formation with reduced echo density, smooth contours and internal echo signals | Cyst with hemorrhage | |
| Oval, round or elongated inclusion with a loose echostructure | Thrombosis | |
| Areas of varying echogenicity, presence of gas bubbles (not always), uneven contour, echogenic membrane | Abscesses | |
| The hypoechoic zone is round in shape with smooth contours, the presence of echogenic outgrowths extending to the periphery | Nodular hyperplasia | |
| Homogeneous formation with smooth contours, presence of internal signals (not always) | Adenoma | |
| An area with a heterogeneous structure, the presence of areas of hemorrhage and calcifications (not always), changes in local lymph nodes, possible definition of ascites | Liver cancer | |
| Formations with uneven borders and a hypoechoic contour (sometimes), the organ tissue has not changed | Metastases |
For the most accurate and informative study, the patient must properly prepare for the procedure, taking into account exactly how it will be carried out.
Contraindications for ultrasound of the pancreas
Due to the fact that the sensor comes into contact with the skin, in case of any lesions of the skin in the epigastric region (dermatitis, purulent inflammation, herpes zoster, various wounds, scabies, etc.), the examination will have to be postponed. It will also not be possible to carry out the procedure if you are severely obese due to the difficulty, and sometimes even impossibility, of seeing the pancreas behind the thick layer of fat. An allergic reaction to the gel used during the procedure is also a contraindication, but is extremely rare.
Signs
On ultrasound you can notice diagnostic symptoms of structural heterogeneity:
- In acute inflammation, the organ on the screen is bright, its contours are uneven. Due to the active inflammatory process, the pancreas is significantly increased in size.
- With chronic inflammation, the normal size of the organ is noted; in the monitor it is not as bright as with acute pancreatitis. The structure is heterogeneous, sometimes fine-grained.
- With fibrosis, the organ is slightly reduced in size. It is most often visualized as hyperechoic and structurally heterogeneous.
- With an age-related change such as lipomatosis, the gland will be moderately hyperechogenic. The doctor notes diffusely heterogeneous changes in the gland tissue.
Experience in the use of echography in acute pancreatitis and its complications
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Introduction
In Russia, in recent years, there has been a tendency towards an increase in the number of patients with acute pancreatitis, the frequency of which reaches 2.5 - 8.4% among patients with acute surgical diseases of the abdominal organs [1]. In Western European countries, in particular in Denmark, from 1979 to 1992, the incidence of acute pancreatitis increased from 26.8 to 35.4 per 100,000 population [15], i.e. by 25%. According to M.V. Grinev [8], of all patients with acute pancreatitis, destructive forms were noted in 16.2%, which, with progression, lead to mortality in almost 50% of cases [4].
Thanks to new research methods (ultrasound, CT, NMR), the early diagnosis of acute pancreatitis and its complications has improved, and it has become possible to dynamically monitor patients during treatment. Ultrasound diagnostics is of particular interest for wide practice - a non-invasive, non-ionizing method that can be used repeatedly without causing harm to the patient. With the help of echography, it has become possible to effectively carry out not only diagnostic, but also therapeutic minimally invasive interventions on the pancreas - biopsy, drainage of pathological formations, etc. [4, 6, 8].
Despite the intensive introduction of echography into practice and certain successes in studying the capabilities of the method, the literature has not yet sufficiently covered issues related to the details of ultrasound semiotics of acute pancreatitis. The echographic picture of acute pancreatitis depending on the stage of the disease is not specified; issues related to the diagnosis of complications of acute pancreatitis, especially rare but clinically significant ones, are poorly reflected [2, 5, 9 - 14, 16]. In patients treated surgically for acute pancreatitis, the problem of ultrasound monitoring in the postoperative period remains relevant. The role of ultrasound data for developing individual treatment tactics and predicting possible complications in each individual patient has been practically not studied.
Materials and methods
The work is based on data from 534 ultrasound examinations of 278 patients with acute pancreatitis who were treated at City Clinical Hospital No. 9 for the period 1992-1995. The studies were carried out using an ultrasonic scanner equipped with a 3.5 MHz convex sensor and a 5 MHz sector sensor.
results
Based on our observations, the following sonographic features of acute pancreatitis were identified:
Changes directly in the pancreas:
- an increase in the size of the pancreas (Fig. 1) was noted in 88% of cases. Normal dimensions of the pancreas: head 3-4.5 cm; body 2.5 - 3 cm; tail 3-4 cm;
- blurred contours - 90.6% of cases;
- an increase in the distance between the posterior wall of the stomach and the anterior surface of the pancreas over 3 mm and reaching 10 - 20 mm, which characterizes swelling of the parapancreatic tissues, was noted in 53% of cases (Fig. 1);
- change in the echogenicity of the gland: increase - 85.6% of cases (Fig. 2); normal - 8.6% of cases; decrease - 5.8% of cases.
Rice. 1.
Acute pancreatitis, destructive form. An increase in the size of the pancreas, blurred contours, an increase in the distance between the posterior wall of the stomach and the pancreas.
Rice. 2.
Acute pancreatitis, increased echogenicity of the pancreas (compared to the echogenicity of the liver).
Changes in the abdominal cavity, which are indirect signs of acute pancreatitis and related to its complications:
Omentobursitis
(Fig. 3) occurs in 28.4% of cases (of which 48% in men and 52% in women). Some authors designate this pathology as “pancreatic pseudocyst.” The volume of such formations has been noted to range from 5 ml (small volumes must be differentiated from vascular aneurysms) to 3 liters or more. The rate of formation of omentobursitis in acute pancreatitis is from 2 to 4 days. from the onset of the disease to 2 - 4 weeks. During ultrasound examination, omentobursitis is presented as an anechoic formation with clear contours, irregular or rounded shape, often with a homogeneous structure, with a wall thickness of 0.2 - 0.4 cm. With echographic monitoring, wall thickening is up to 0.5 - 1.0 cm with the appearance of structural heterogeneity should be regarded as a sonographic sign of abscess formation.
Rice. 3.
Pancreatic pseudocyst in acute pancreatitis in the form of an anechoic formation with clear contours, a homogeneous structure, with the presence of hyperechoic inclusions (detritus of the pancreas).
Free fluid in the abdomen
- noted in 18% of cases (Fig. 4), of which 80% in men and 20% in women. Fluid in a volume of up to 100 ml is detected only in one anatomical area (usually in the pelvis), more than 100 ml - in the lateral canals and in other parts of the abdominal cavity. In the first days of development of acute pancreatitis, the fluid is homogeneous, after 6-12 days. often the structure is heterogeneous due to “thread-like” inclusions (usually fibrin).
Rice. 4.
Dilated loops of the small intestine up to 3.5 cm, filled with liquid contents against the background of free fluid in the abdominal cavity.
Biliary hypertension
- occurs in 13% of cases, of which 25% in men and 75% in women. Echography reveals dilation of the intrahepatic bile ducts, common hepatic duct and common bile duct. In the absence of choledocholithiasis, biliary hypertension is usually observed with focal pancreatic necrosis in the area of the head of the pancreas.
Abdominal infiltrates
- found in 5.4% of cases (Fig. 5, 6), including 64% in men and 36% in women. As a rule, the greater omentum is infiltrated (omentitis), visualized as a formation of increased echogenicity with unclear uneven contours, a heterogeneous structure, with areas of reduced echogenicity, which may indicate the formation of abscesses in it. The sizes of infiltrates range from 5 to 15 - 20 cm.
Rice. 5.
Infiltration in the abdominal cavity in the projection of the greater omentum is represented by an irregularly shaped formation with unclear contours, a heterogeneous structure, and the presence of hyper- and hypoechoic areas. The size of the infiltrate is 8.5 x 3.9 x 5.3 cm.
Rice. 6.
Infiltrate in the projection of the greater omentum with an anechoic inclusion up to 4 cm (abscess formation).
Retroperitoneal phlegmon
- occur in 4.3% of cases (Fig. 7), of which 67% in men and 33% in women. In 95% of cases, left-sided localization of phlegmon was diagnosed, which was determined in the form of an anechoic or hypoechoic formation, often slit-like or oval in shape. As a rule, the cause of the development of this complication is the spread of pancreatic secretion through the retroperitoneal space from the pseudocyst, sometimes reaching the groin area. Pancreatogenic paranephritis can be considered as a variant of retroperitoneal phlegmon.
Rice. 7.
Retroperitoneal phlegmon on the left is an anechoic formation of irregular shape with unclear contours. The scan was performed from the left lumbar region.
Hydrothorax
- occurs in 2.2% of cases, equally often in men and women, with predominantly left-sided localization.
Thrombosis in the portal vein system
- noted in 1.5% of cases (Fig. 8 a, b) and can be determined quite well, in our opinion, without a Doppler study. If there are signs of portal hypertension, a targeted ultrasound examination of the vessels of the portal vein system must be performed. Thrombi can be single or multiple. They are localized both in the portal vein itself and in the splenic and superior mesenteric veins.
Rice. 8.
Portal vein thrombosis. The lumen of the vein is completely obstructed by an isoechoic formation with clear contours, heterogeneous structure, up to 4.7 cm long (a - sagittal section, b - transverse section).
Intestinal paresis
- occurs in 1.4% of cases (see Fig. 4), of which 75% in men and 25% in women. It is characterized by the expansion of the loops of the small intestine up to 3 - 5 cm with their filling with liquid contents and recorded “pendulum-like” peristalsis.
Hydropericardium
- occurs in 0.4% of cases.
Ascending mediastinitis
, noted by other authors, was not observed by us.
Pancreatic abscesses
- usually occur against the background of existing ultrasound signs of chronic pancreatitis.
Ruptures of pancreatic pseudocysts
during ultrasound diagnostics were observed in 2 patients (0.7%).
Hemorrhage into a pancreatic pseudocyst with the formation of an organized hematoma
(Fig. 9) was noted in 1 patient (0.35%).
Rice. 9.
A pancreatic pseudocyst in the form of an anechoic formation with clear contours, in which another anechoic formation with a capsule of 0.2 - 0.3 cm is identified (at surgery - a pseudocyst with an organized hematoma).
Pancreatic pseudocysts with atypical localization
(in the liver, spleen, periduodenal, etc.) were detected in 2 patients - 0.7% (Fig. 10).
Rice. 10.
An atypically located pancreatic pseudocyst (paraduodenal) in the form of an anechoic formation of a round shape with clear contours, a homogeneous structure, up to 4.5 cm in size, located next to the duodenum.
Splenic infarctions
(1 patient - 0.35%) - against the background of portal vein thrombosis with portal hypertension.
Splenic ruptures
due to portal hypertension (we did not observe).
Pancreatogenic paranephritis
— found in 2 patients, which amounted to 0.7% (Fig. 11).
Rice. eleven.
Left-sided pancreatogenic paranephritis, visualized as a liquid formation surrounding the kidney on all sides. Cross section.
Conclusion
The study shows that ultrasound diagnostics should be a mandatory element of the diagnostic algorithm in patients with acute pancreatitis. To increase the diagnostic value of echography, a certain sequence in performing an ultrasound examination is necessary: a detailed examination of the parapancreatic tissues and the gland itself; examination of all parts of the abdominal cavity for free fluid and infiltrates; examination of the pleural cavities and pericardial cavity for the presence of effusion; detailed examination of intra- and extrahepatic bile ducts; targeted examination of the vessels of the portal vein system; examination of the retroperitoneal space; dynamic observation (the frequency of repeated ultrasound is determined by the severity of the disease and the likelihood of complications).
To improve ultrasound results, the following techniques can be recommended:
- if visualization is poor, it is better to examine the tail of the pancreas through the spleen or left kidney;
- to improve visualization of the pancreas, you can fill the stomach with 500 - 800 ml of degassed liquid (water);
- use sensors with different radiation frequencies for a more detailed study of pathological foci located at different distances from the sensor;
- use polypositional scanning with dosed compression on the abdominal wall to improve visualization of the organs being examined, which allows you to “spread apart” the intestinal loops, thereby creating an additional “acoustic window”;
- use ultrasonic fistulography with liquid and gas-forming solutions (furacilin, novocaine, Echovist) to determine cavities in the presence of pancreatic fistulas [7], which may be the subject of separate studies.
Literature
- Skuya N. A. Diseases of the pancreas. - M.: Medicine, 1986.
- Zubarev A. R., Grigoryan R. A. Ultrasound angioscanning. - M.: Medicine, 1990.
- Filin V.I., Kostyuchenko A.A.. Emergency pancreatology. - St. Petersburg, 1994.
- Nesterenko Yu. A., Mikhailusov S. V., Imanaliev M. R. Ultrasound in the diagnosis and treatment of pancreatic necrosis / Sat. scientific tr. Plenum of the problem commission on emergency surgery. - M.: 1994. - P. 26 - 29.
- Baranov G. A., Mogutov M. S., Zavyalova N. I. Ultrasound diagnosis of portal vein thrombosis as a rare complication of acute pancreatitis / Sat. scientific tr. international conference “New technologies in diagnostics and surgery of the biliopancreaticoduodenal zone”. - M.: 1995. - P. 4 - 5.
- Belokurov GO. Ya., Utkin A.K., Zhokhov V.K., Belokurov S.Yu., Mogutov M.S. Prerequisites for the use of precision technology in the treatment of false cysts of the pancreas/ Sat. scientific tr. international conference “New technologies in diagnostics and surgery of the biliopancreaticoduodenal zone”. M.: 1995. - P. 78.
- Builov V. M., Mogutov M. S., Karpov N. R. Ultrasound fistulography with “Echovist-300” in surgery and urology. — Materials of the II Congress of the Association of Ultrasound Diagnostics in Medicine. - M.: 1995. - P. 80.
- Grinev M.V., Krasnogorov V.B., Ryss A.S., Veselov V.S., Smelyansky A.I., Alekseenko E.N. Effective tactics for the treatment of destructive pancreatitis based on early plasmapheresis and minimally invasive surgical interventions/ Coll. scientific tr. "Minimally invasive interventions in surgery." M.: 1996. - P. 257.
- McCormick P.A., Chronos N., Burroughs A.K., McLaughlin N., McLaughlin J.E. Pancreatic pseudocyst causing portal vein thrombosis and pancreatico-pleural fistula. In: Gut (1990 May) 31(5):561-3.
- Fernandez-Cruz-L., Margarona-E., Llovera-J., Lopez-Boado-MA, Saenz-HT. Pancreatic ascites. Hepatogastroenterology. 1993 Apr; 40(2): 150-4.
- Nishida-K., Terai-Y., Nojiri-L, Kato-M., Higashijima-M., Takagi-K., Adashi-R. A case of pancreatic pseudocyst with intracystic hemorrhage and repeated gastrointestinal bleeding. Nippon-Ronen-Igakkai-Zasshi. 1993 Aug; 30(8): 714-9.
- Sonak-R., Stock-W., Janzik-U., Hayduk-K., Borchard-F. Duodenal duplication cyst is a rare cause of acute recurrent pancreatitis. Leber-Magen-Darm. 1993 Sep; 23(5): 211-5.
- De-Ronde-T., Van-Beers-B., de-Canniere-L., Trigaux-JP., Melange-M. Thrombosis of splenic artery pseudoaneurysm complicating pancreatitis. Gut. 1993 Sep; 34(9): 1271-3.
- Hamm-B., Franzen-N. Atypically located pancreatic pseudocysts in the liver, spleen, stomach wall and mediastinum: their CT diagnosis. Rofo-Fortschr-Geb-Rontgenstr-Neuen-Bildgeb-Verfahr. 1993 Dec; 159(6): 522-7.
- Worning-H. Acute pancreatitis in Denmark. Ugeskr-Laeger. 1994 Apr 4; 156(14): 2086-9.
- Yasuda I., Tomita E., Nishigaki Y., Ino Y., Shimizu H., Yamada T., Kawamura H., Kuroda T., Takahashi T., Nagura K. A case of portal vein thrombosis subsequent to acute pancreatitis. Nippon Shokakibyo Gakkai Zasshi (1995 Apr) 92(4):820-5.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.