Esophageal erosion is an inflammatory disease that occurs with superficial damage to the mucosa. The disease occurs in both acute and chronic forms and is caused by various reasons (chemical burns, infectious lesions, trauma, stomach diseases). The first symptoms of the disease are: heartburn, belching, pain in the epigastric and retrosternal areas. Symptoms and treatment of esophageal erosion depend on the factors that caused the pathology. The therapeutic regimen includes diet, drug therapy, and physical therapy. Traditional medicine methods are often used. How and how to treat pathology will be discussed further.
What is esophageal erosion
A mucosal defect in the form of erosion cannot occur without inflammation. There is a whole group of inflammatory diseases of the esophagus with a common name - esophagitis. Erosive esophagitis is an acute or chronic inflammatory disease of the esophagus, manifested by mucosal erosions.
Esophageal erosion is a superficial defect of the mucosa that does not affect the basement membrane and underlying layers. Damage is limited to the epithelium, so no scars form when healing occurs.
Causes and mechanisms of formation
The causes of acute erosive lesions of the esophageal mucosa are:
- injuries to the mucous membrane, when swallowing rough food or foreign bodies;
- burn of the mucous membrane when swallowing caustic alkalis and acids;
- infectious lesions of the organ (diphtheria, typhus, esophageal candidiasis);
- allergic diseases.
Symptoms of candidal esophagitis
The most common cause of chronic erosive esophagitis (disease duration of more than six months) is regurgitation of stomach contents into the esophageal tube.
There are three main components in the pathogenesis of the development of peptic erosions:
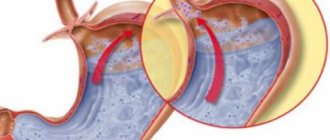
- Impaired functioning of the LES (lower esophageal sphincter), which may be the result of dysfunction of smooth muscles, diaphragmatic hernia, as well as the result of uncontrolled use of drugs that relax smooth muscles (calcium antagonists, aminophylline, nitrates). In addition, the causes of cardia insufficiency can be obesity, pregnancy, and scleroderma.
- The rate of cleansing and emptying of the esophagus (esophageal clearance). With normal esophageal clearance, even frequent reflux of gastric contents does not lead to disease. Reduced esophageal clearance is facilitated by: excessively hasty eating, swallowing large amounts of air, fatty and fried foods, frequent alcohol consumption, smoking.
- Violation of the mucosal protection mechanism (the result of a violation of the aqueous-mucosal pre-epithelial layer containing bicarbonates). This occurs as a result of changes in the composition of saliva and disturbances in the salivary-esophageal reflexes.
Erosion of the esophagus is formed as a result of damage to the epithelial layer of the inner lining by refluxate (stomach contents), against the background of a decrease in its motor function and a violation of the protective mechanism of the mucosa.
Esophageal erosion: symptoms
Erosive inflammation can be practically asymptomatic; patients in this case are bothered by slight discomfort in the epigastrium. Such cases are especially difficult to diagnose. More often, the clinical picture is quite pronounced.
Symptoms of esophageal erosion can be divided into esophageal and extraesophageal.
The esophageal ones include:
- Heartburn is a burning sensation in the epigastric (above the stomach) and retrosternal region (behind the sternum), more often occurs when there are errors in the diet: after drinking alcohol, carbonated drinks, coffee. In severe cases, heartburn is almost constant.
- Pain in the epigastrium and in the retrosternal region, sometimes it is of a burning or pressing nature, radiates to the left side of the back and left arm, unlike coronary pain, it goes away after taking antacids.
- Dysphagia with erosive esophagitis is explained by esophageal dyskinesia and is transient.
- Nausea in the morning, associated with passive flow of stomach contents into the esophagus.
- Belching with a sour or bitter aftertaste.
- In severe cases of the disease, vomiting mixed with scarlet blood may occur.
Extraesophageal symptoms of esophageal erosion:
- from the cardiac system: cardialgia (pain in the heart area), tachycardia (rapid heart rate), arrhythmias;
- from the pulmonary system: hacking cough at night, sleep apnea (the symptom can become a trigger for bronchial asthma, pneumonia);
- from the ENT organs: chronic laryngitis, hoarseness, pharyngitis;
- from the dental organs: destruction of tooth enamel, chronic stomatitis, chronic periodontitis.
Symptoms
The clinical manifestation of such a pathological process quite often resembles the symptoms of other diseases of the small intestine, stomach or liver. In some cases, the pathology occurs without expressing any symptoms. Despite this, symptoms of esophageal erosion are:
- heartburn - can be permanent or occur due to consumption of spicy and fatty foods, as well as acidic foods. In addition, it may appear when the body is in a horizontal position;
- pain and discomfort in the chest area, which may intensify while eating;
- heaviness in the stomach and rapid satiety;
- disturbance of the swallowing process - the appearance of pain when eating solid food;
- belching with a sour and unpleasant odor of undigested food;
- persistent hiccups;
- nausea and vomiting in the morning. In severe cases of the disease, the vomit contains blood admixtures;
- increased salivation;
- the occurrence of an unpleasant odor from the oral cavity.
Such signs quickly go away, which is why a person may not pay attention to them, attributing everything to the consumption of low-quality products. But as the disease progresses, such symptoms occur more frequently and become more intense. Drinking alcoholic beverages, frequent smoking and stress contribute to the aggravation of the disease.
The symptoms of esophageal erosion can be eliminated by taking medications or treating esophageal erosion with traditional medicine.
Degree of development of the erosive process
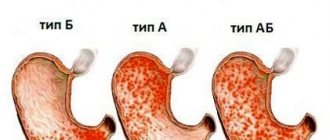
Erosive esophagitis, especially if it is localized in the proximal (upper) sections, can go away on its own. However, if the cause of esophagitis is GERD - gastroesophageal reflux disease, then as the disease develops, the erosive process also progresses. There are four degrees of development of esophageal erosions against the background of GERD:
- first degree - single, small, non-confluent erosions against the background of inflamed esophageal mucosa;
- second degree - merging erosions, with areas of healthy tissue between the lesions.
- third degree - erosive lesions deepen, ulcerative defects appear, merged erosions and ulcers spread to the entire surface of the mucosa;
- fourth degree, complications appear: chronic ulcer, stenosis, Barrett's esophagus.
Treatment and prevention of complications of erosive reflux esophagitis
Lecture transcript
XXV All-Russian Educational Internet Session for doctors
Total duration: 19:23
00:00
Oksana Mikhailovna Drapkina, Secretary of the Interdepartmental Scientific Council on Therapy of the Russian Academy of Medical Sciences, Doctor of Medical Sciences, Professor:
— Yuri Alexandrovich Kucheryavy. Treatment and prevention of complications of erosive reflux esophagitis.
Yuri Aleksandrovich Kucheryavyi, Candidate of Medical Sciences:
— Good afternoon, dear colleagues! This topic is no less relevant today than the previous one, since GERD is a fairly common disease in the population. According to epidemiological studies, the incidence rate, as you know, reaches 10%, and in some age groups it exceeds this figure.
Many authors dealing with this problem present the structure of reflux disease in the form of a pyramid, the basis of which is non-erosive and erosive reflux disease. It is the second form that is threatening with its complications, which develop quite often, forming the “heart” and top of the pyramid in a figurative sense. The most formidable, most severe complication is, of course, cancer in the form of adenocarcinoma, absolutely associated with GERD.
So, the incidence of complications in patients with GERD exceeds 20%. The most common is stricture and Barrett's esophagus, the development of gastric and intestinal metaplasia in the esophagus, which is the background, the basis for the development of adenocarcinoma of the esophagus. Its risk increases tenfold in patients with Barrett's esophagus. We see that more than 10% of patients suffering from reflux disease experience these dangerous complications.
The first question that arises for a clinician is: how to classify ulcers and strictures in the structure of GERD? The Los Angeles classification of reflux esophagitis, which has been very often used in recent years, does not allow us to diagnose complications. We can only stage the esophagitis. But no one has canceled the old classifications: in particular, stage IV reflux esophagitis according to the Savary-Miller classification implies both the presence of strictures and the presence of Barrett’s esophagus.
02:33
In large epidemiological studies, the incidence of complications of reflux disease varies widely. This depends, of course, on the design of the studies. If we take endoscopic studies, the patients who were included in them were sent to endoscopic rooms regarding certain complaints that they had already made during the initial examination, during the screening examination.
Their frequency is higher, but we take this into account and see that in large studies involving more than a thousand patients, the incidence of Barrett's esophagus and strictures exceeds 1.5%-2% and increases with age (as for Barrett's esophagus - almost three times ).
Esophageal strictures develop slowly over many months and years. These are precisely the months and years when we could prevent their development if the diagnosis of reflux disease was made in a timely manner and adequate treatment was prescribed.
Hundreds of my patients who come to see us have been complaining of heartburn for many years. Nobody pays serious, worthy attention to this - including the patients themselves. This cannot but cause surprise. We can’t help but talk about this. Of course, heartburn may subside over time as a stricture develops. Other complaints dominate, such as dysphagia.
There is a certain relationship with NSAIDs, which are talked about so much today. This is partly because NSAIDs and proton pump inhibitors are extremely commonly prescribed drugs in internal medicine.
Case-control studies have shown that there is an increased risk of developing peptic esophageal strictures in individuals taking NSAIDs. At the same time, it has been absolutely proven that drugs of this group do not cause or initiate reflux disease, without in any way pathogenetically affecting the tone of the lower esophageal sphincter, the adequate function of which is essential in the pathophysiology of reflux disease.
There may be a random relationship, since erosive forms of reflux disease are more common in older patients. These patients are more likely to take NSAIDs.
It is possible that NSAIDs and aspirin, taken in a non-coated form, may have a local irritant effect in patients with reflux disease, causing increased inflammation and the formation of a stricture. However, this pathophysiological relationship has not been proven at all and remains only a hypothesis.
05:47
How do esophageal strictures progress clinically? Of course, the dominant symptom is dysphagia: difficulty swallowing. Odynophagia (pain when swallowing) is less common. With severe strictures, regurgitation of undigested food occurs (vomiting after eating). In advanced cases, weight loss also appears. During the examination, we detect a narrowing of the esophagus (according to X-ray and endoscopic methods). It is possible to detect anemia as a consequence of nutritional deficiency.
For many years, X-ray examination was the main and main thing. It remains indicative to this day. We see what strictures can be diagnosed in patients with complaints of dysphagia. If the patency is extremely compromised, priority for radiological examination may be in favor of water-soluble contrast.
The most important method for diagnosing complications of reflux disease and strictures, which we are talking about now, is esophagogastroduodenoscopy. Endoscopic methods that allow not only to evaluate the localization of the stricture and the degree of narrowing with the eye, but also to carry out sampling for morphological examination, for staging, to identify Barrett's esophagus. Often both stricture and Barrett's esophagus are combined in one patient.
Or verify another diagnosis, which I will say a few words about today: eosinophilic esophagitis.
According to localization, strictures are divided into high, medium and low. Reflux disease is characterized by low strictures, while other diseases (in particular, eosinophilic esophagitis) are characterized by high and combined strictures. Less often combined.
07:48
This table briefly presents the differential diagnosis of strictures and the main nosological forms that require inclusion in the differential diagnosis.
These are GERD-associated strictures, which are characterized by a long course of symptoms of reflux disease, that is, heartburn. Over time, it can be, say, reduced and resolved. These patients will develop dysphagia. The examination often reveals a solitary stricture in the lower third of the esophagus. Histological examination of the mucous membrane of the esophagus often reveals a picture of Barrett's esophagus.
In the presence of dysphagia in a patient with eosinophilic esophagitis, examination often reveals multiple circular strictures. Most often this is the upper and middle third of the esophagus, but it may also be the lower third, which will to some extent mislead us towards the more common reflux disease with a complication in the form of a stricture. Histological examination may reveal pronounced eosinophilic infiltration.
In patients with esophageal cancer, two forms are most common (about 50/50, as you know). Adenocarcinoma of the esophagus, absolutely associated with reflux disease, as I already said. Squamous cell carcinoma: the significance of gastroesophageal reflux in the pathophysiology of this form of cancer has not yet been completely proven. With exophytic tumor growth, dysphagia may also occur. There may be a history of reflux disease to varying degrees. This applies to a greater extent, of course, to adenocarcinoma.
With achalasia, dysphagia and regurgitation of undigested food are manifested. A pronounced narrowing in the lower third of the esophagus is revealed by fluoroscopy. Moreover, during esophagogastroduodenoscopy in the early stages of achalasia, this seemingly narrowing zone is absolutely passable. The mucous membrane is most often unchanged.
Just a few words about eosinophilic esophagitis. This is what multiple circular narrowings or solitary strictures look like, as shown in the top pictures. But (this must be remembered) with this disease, edema with hyperemia is often detected (relatively less often than with GERD), which can confuse us in terms of making a diagnosis.
As Oleg Samuilovich said today, it is necessary to establish a correct diagnosis. After that we will be confident in carrying out treatment, so regarding strictures and dysphagia, of course this is important. Especially when every year we know more and more about eosinophilic esophagitis.
10:47
During X-ray examination, we see typical signs - jagged contours and high multiple strictures.
Histological examination shows more than 15 eosinophils per field of view for eosinophilic esophagitis. In order to establish a diagnosis (I emphasize again), histological examination data may not be enough, although there are international criteria for establishing this diagnosis. The presence of symptoms, the presence of histological signs of eosinophilic esophagitis, the exclusion of other diseases, first of all. In any case, the approach must be comprehensive.
The most common are strictures associated with GERD. Treating them is not an easy task, especially when patients present at advanced stages of stricture, when only surgery can help.
The key to successful treatment of strictures, if they are diagnosed at an early stage, and their prevention is timely diagnosis and timely treatment of GERD. With an adequate approach, when prescribing modern medications, it is also possible to reverse the (partial) development of the stricture that has formed.
In the event that there is clinically significant dysphagia and esophageal obstruction, of course, we will need the help of a surgeon. At the first stage, as a rule, minimally invasive interventions are performed: dilatation of strictures, that is, bougienage or installation of stents. These measures provide a fairly good clinical effect. Most often, their success is consolidated by the subsequent administration of modern proton pump inhibitors.
In the event that conservative treatment is ineffective or impossible, and minimally invasive surgical techniques are not effective, then extensive surgical interventions are performed.
12:58
The practical doctor is faced with the question of which drug to choose. All I can say is that you need to choose a proton pump inhibitor. This is absolutely clear. The more severe the form of reflux disease, the more effective the drug should be prescribed. But there should be no thought about whether to prescribe antacids or maybe prescribe prokinetics or H2 blockers or PPIs.
Definitely proton pump inhibitors! These results have been proven at the level of meta-analyses. This situation is not discussed. Prescribe any drug that you work with, that you trust, taking into account the accompanying prescriptions, as Tatyana Lvovna said today. The choice of drug may be significant due to drug-drug interactions.
I want to show the results of a fairly large meta-analysis, indicating the advantages of PPI stereoisomers (esomeprazole at a dose of 40 mg) over first-generation drugs in the effectiveness of treating severe C, D stages (according to the Los Angeles classification) of erosive esophagitis within 4, and for 8 weeks. This meta-analysis shows the benefits of newer PPIs (such as Nexium).
Why should the duration of treatment for reflux disease be long enough? Of course, you know that the morphological basis of reflux disease (both erosive and non-erosive forms) is the expansion of intercellular contacts. This is a typical sign of reflux disease, which we can rarely diagnose, since electron microscopy is not usually used in clinical practice to verify this condition.
There are several studies that have assessed the dynamics of the width of the intercellular spaces of squamous epithelium in the esophagus during PPI therapy. It has been shown that even if we use modern PPIs (Nexium at a dose of 40 mg per day for 8 weeks), only just over 80% of patients experience normalization of the intercellular spaces, indicating the onset of some remission of reflux disease.
Moreover: only those patients in whom the intercellular spaces in the squamous epithelium in the esophagus were normalized had 100% control of the symptoms of the disease. This also proves the concept.
15:35
If we resort to balloon dilatation, bougienage, we still need to use conservative therapy. We see that severe damage to the mucous membrane is accompanied by erosive esophagitis. There are often tears in the mucous membrane, accompanied by bleeding.
The prognosis for strictures is as follows. It is relatively favorable when it comes to reflux disease and adequate treatment for this disease. Patients in most cases can completely return to their normal lifestyle. With continuous maintenance antisecretory therapy, strictures rarely recur.
In the event that conservative measures are ineffective, we resort to the help of a surgeon - operations such as Lewis or Garlock are performed with plastic surgery of a removed segment of the esophagus with the stomach.
A few words about esophageal ulcers. Etiology: reflux disease also most often contributes to the overall structure of esophageal ulcers. We see that other viral and fungal infections that cause ulcers occur, as a rule, in HIV-infected patients who, in fact, already have AIDS.
Quite often, an esophageal ulcer causes bleeding.
Here are other causes not associated with reflux disease: fungal esophagitis, herpetic, cytomegalovirus ulcers, which will require etiotropic therapy in terms of treatment if we identify them.
As for ulcers within the framework of GERD, pathogenetic treatment is also needed here. PPIs and the drug of choice are the more effective, more modern stereoisomers that are on our market. Modern prokinetics may be prescribed as additional treatment. For symptomatic purposes - antacids and alginates.
The duration of therapy is determined by the healing time. As I already said, this is at least 8 weeks for standard therapy for reflux esophagitis. If we are talking about complications, then this is a longer period of time. For Barrett's esophagus, this is absolutely a continuous treatment.
18:00
We see from the results of one of the studies demonstrated on this slide that the more severe the heartburn, the longer it lasts, the higher the risk of complications. This issue simply needs to be addressed.
This slide shows us why longer and more powerful acid suppressive therapy is necessary for Barrett's esophagus. Yes, because there is brighter, more pronounced, more powerful acid reflux.
Our patients must stay with us. Perhaps only those who do not experience symptoms of reflux disease, which are present in patients with a complicated form of the disease, are satisfied. Only successful therapy can increase treatment adherence. The faster the effect occurs and the more predictable it is, the greater will be our overall success.
As a conclusion, I would like to say a few words. The key to the success of treatment and prevention of complications of reflux disease is timely, adequate and long-term antisecretory therapy.
Thank you very much for your attention.
19:23
What is linear erosion of the esophagus
There are superficial and linear erosions. Superficial defects during development involve increasingly deeper layers of the mucous and submucosal membranes in the inflammatory process, resulting in the formation of ulcers.
Linear erosion is an inflammatory damage to the esophagus, characterized by the spread of the process deep into the esophageal wall, initially with the formation of small ulcers, which then turn into diffuse lesions. With this type of development of the process, scar-adhesive deformations of the organ occur, disrupting the configuration and function of the organ. Such changes, of course, cannot be cured quickly.
Inflammation of the esophagus is a common pediatric pathology, but in a child it usually occurs in the form of edematous and catarrhal forms (without the formation of mucosal defects).
Why is pathology dangerous?
Erosive processes are far from harmless. What is dangerous about erosion of the esophagus and stomach is its complications. Untimely or illiterate treatment can lead to very dangerous conditions:
- Esophageal stricture more often occurs with unreasonably short courses of treatment (up to 4 weeks) or with insufficient therapy to reduce gastric secretion. Strictures of the esophagus lead to disruption of the nutritional process, cachexia, and require surgical intervention, which is difficult for the patient.
- A peptic ulcer of the esophagus is a deep defect in the wall of the esophagus, leading to deformation and shortening of the organ.
- Barrett's esophagus is a metaplasia of squamous epithelium into columnar epithelium, which greatly increases the risk of cancer.
- Periodic or constant bleeding from ulcerative defects.
- Threat of esophageal perforation with deep peptic ulcers.
With gastric erosions, there is also a danger of bleeding, deformation and malignancy (development of tumor diseases). These two diseases are similar in morphological changes, symptoms and treatment.
Diagnostics
All patients with suspected esophageal erosion undergo a mandatory set of instrumental and laboratory examinations:
- Esophagoscopy - allows you to determine the severity of the lesion, the depth of the defect, and identify diseases and conditions such as esophageal cancer, bleeding, strictures of the esophagus and outlet. The method allows you to take a biopsy for histological and cytological analysis.
- X-ray examination with contrast of the esophagus - used to identify scar changes, deformities and narrowings. Allows you to determine the presence of diaphragmatic hernias.
- Esophageal manometry - identifies symptoms of esophageal motility disorder, how well the work of the upper and lower esophageal sphincters is coordinated with esophageal motility.
- Daily pH metry - this technique allows you to determine how often a patient experiences reflux during the day, how long it lasts, as well as esophageal clearance indicators.
Of the laboratory indicators, doctors are primarily interested in:
- peripheral blood test to look for signs of anemia in cases of internal esophageal bleeding (this may be a symptom of occult bleeding);
- stool analysis - this study allows you to determine small amounts of blood that do not yet affect hemoglobin and hematocrit.
Detection of Helicobacter pylori infection is not important for diagnosing esophageal erosion. But in order to fully treat erosive changes, it is necessary to know about the presence of Helicobacter pylori in the patient. Therefore, it is necessary to determine the presence of Helicobacter in the feces, do an enzyme-linked immunosorbent assay (ELISA) of the blood, and conduct a breath test.
Manifestation of erosive lesions of the esophagus
The patient complains of symptoms and signs such as nagging pain in the chest, worsening after eating and when lying down. Dysphagia, a swallowing disorder, often occurs. A person finds it difficult to eat, and sometimes it is difficult for him to even drink water. This condition can be debilitating, so it is important to treat the condition early.
Other symptoms of esophageal erosion include nausea and vomiting. The patient is bothered by severe heartburn, hiccups and belching of air, and increased salivation often occurs. Often the patient has the sensation of a foreign object stuck in the esophagus. Such symptoms indicate the presence of erosion and severe inflammation of the mucous membrane.
A danger signal is vomiting blood or tarry stools. The patient is prohibited from eating and drinking. These symptoms indicate internal bleeding, which requires immediate hospitalization. Bleeding from the esophagus occurs for various reasons: it can be either mechanical damage or a side effect from taking NSAIDs. Symptoms of organ damage include pain when swallowing or odynophagia.
Diagnosis of esophageal erosion
The doctor sees the full picture of the disease during esophagogastroduodenoscopy. With erosive damage to the esophagus, its lining is hyperemic and vulnerable to contact. Defects are rarely isolated; signs of inflammation of the esophagus are also increased mucus formation and swelling.
To determine the exact causes of a disease, a tissue sample is sometimes taken during the procedure for later testing.
Additionally, the following methods for diagnosing esophageal erosion are used:
- clinical and biochemical blood test;
- coprogram with stool examination for occult blood;
- Ultrasound of the peritoneal organs.
Fluoroscopy is required. The patient is asked to drink a solution of barium sulfate. During the procedure, the presence of a diaphragmatic hernia is established, the structures and erosions of the esophagus are determined, and gastroesophageal reflux is diagnosed. In difficult cases, research methods such as magnetic resonance or computed tomography, daily pH impedance measurements are recommended.
Therapy
Before treating esophageal erosion, it is necessary to eliminate those habits and lifestyles that directly or indirectly led to the appearance of symptoms and the development of the disease:
- It is necessary to accustom yourself to eat regularly, often, in small portions. Avoid hyperphagia. Avoid foods that irritate the esophageal mucosa (fats, chocolate, citrus fruits).
- Quit cigarettes and alcohol.
- It is necessary to get full rest. Avoid stressful situations
- It is necessary to sleep with the head of the bed raised.
The diet for erosive esophagitis and GERD has been developed in detail. Here you just need to listen to the advice of your doctor. It is necessary to exclude from the menu foods that increase the production of hydrochloric acid and have a relaxing effect on the esophageal sphincter (salted, smoked and fried foods). Food should be boiled or steamed. Diet, as well as drug treatment, are selected individually, taking into account concomitant pathology.
Treatment of esophageal erosion with medications
- Antacids and alginates. Antacid therapy reduces the acidic aggression of gastric juice. By increasing the pH of gastric juice, these drugs reduce its damaging effect on the esophageal mucosa (Maalox, Phosphalugel, Magalfil), and reduce pain symptoms and discomfort. Recently, preparations containing alginic acid salts have been used to treat esophageal erosion. Alginates (Gaviscon, Topalkan) form a thick foamy mass in the stomach, which, entering the esophagus during reflux, has a beneficial effect on the esophageal mucosa, due to which epithalization of erosions in the esophagus occurs faster.
- Drugs that lower the pH in the stomach. PPI (Omez, Controloc, Razo) or IGR (Zantac, Kvamatel). By inhibiting the proton pump, these drugs provide a pronounced suppression of HCl formation. But these drugs do not eliminate reflux.
- Prokinetics. The drugs increase peristalsis of the antrum of the stomach. As a result, the evacuation of food from the stomach to the intestines is accelerated, congestion is eliminated, and the tone of the esophageal sphincters (ganathon, motilium) increases.
Treatment of esophageal erosion will be ineffective if the treatment regimen does not include treatment for concomitant gastric ulcer. In addition to drugs that increase the pH of gastric juice, it is necessary to carry out anti-Helicobacter therapy (Ulkavis, Furazolidone, Amoxicillin), prescribe antispasmodics (Papaverine, No-shpa), selective anticholinergics (Atropine, Platyfillin).
Alternative medicine: treatment with folk remedies
Alternative medicine offers many recipes and treatments for erosive processes in both the esophagus and stomach. The mechanism of action of many of them is clear. Acting superficially, in conditions where the mechanism of protecting the mucosa from damage is impaired, these drugs protect the inner lining of the esophagus. They reduce the severity of symptoms, heal erosions on the walls of the esophagus, increasing the mood of patients and their belief in a speedy recovery.
Substances such as propolis, sea buckthorn oil (a tablespoon, on an empty stomach, three times a day), pharmaceutical chamomile (brew as tea, drink a cup, on an empty stomach). These substances have a beneficial effect on the process of epithelization of erosions. However, it is unlikely that it will be possible to cure severe erosions of the esophagus with folk remedies; they are quite suitable for treating mild cases of erosion at home.
The same recommendations as treating erosions and peptic ulcers with pure alcohol or creolin, to put it mildly, are puzzling.
Creolin is a highly toxic substance and there is no “medical” version of it, so you should not treat it or experiment with your health.
Forecast
With timely and correct treatment, the prognosis is quite favorable.
If the disease is not treated, and the patient is negligent about his health, then severe complications may develop, the most severe of which is adenocarcinoma of the esophagus.
Drug treatment of erosive lesions of the esophagus
If unpleasant symptoms appear, you should consult a gastroenterologist. Treatment of esophageal erosion should be comprehensive. The key to recovery is adherence to a strict diet, the correct daily routine is important. To treat erosive lesions of the esophagus, the following medications are prescribed:
1. PPIs are proton pump inhibitors, or proton pump inhibitors. Their action is aimed at blocking the formation of hydrochloric acid in the stomach, giving erosion the opportunity to drag on. Treatment with these drugs should be a course. The consumer is offered PPIs with such active substances as Esomeprazole, Rabeprazole, Omeprazole, Pantoprazole, Lansoprazole.
2. Antacids. Treatment with drugs based on aluminum, magnesium, and calcium compounds will quickly eliminate the symptoms of the disease. They neutralize stomach acid and coat the esophagus. This category includes Gastal, Maalox, Rennie, Phosphalugel, Almagel.
To relieve severe pain from esophageal erosion, it is recommended to take Almagel A, which additionally has a local anesthetic effect.
3. Gaviscon belongs to the group of alginates and has no analogues on the Russian market. It occupies a special place in the treatment of GERD and its complications in the form of erosions on the esophageal mucosa. When Gaviscon interacts with acid, a gel is formed that prevents reflux and also promotes epithelial repair.
4. Injections of Actovegin solution, which is a tissue regeneration stimulator, will help cure the disease.
5. Prokinetics. The action of these drugs is aimed at improving gastrointestinal motility. Treatment is carried out using such agents as Domperidone (Motilak), Itopride (Ganaton). Accelerated emptying of the stomach promotes recovery.
6. H2-blockers of histamine receptors. Treatment with them is provided if for some reason the patient cannot take PPIs. Famotidine or Ranitidine reduces the production of hydrochloric acid in the stomach, giving the esophageal mucosa the opportunity to recover.
7. Drugs to replenish the deficiency of pancreatic enzymes will help cure erosion. They help improve food digestion. For this, Creon, Mezim, Festal are prescribed.
8. It is recommended to take Vinilin balm (Polivinox). It creates a protective film on the surface of the esophagus. This remedy has a bactericidal and anti-inflammatory effect. With its help, it is proposed to treat not only erosion, but also ulcerative lesions of the gastrointestinal tract.
9. The pharmacy sells sea buckthorn oil for oral administration; it will quickly relieve erosion.
Proper nutrition for erosion
Recovery will not occur if you do not adhere to certain dietary restrictions. The diet for esophageal erosion involves avoiding fried, spicy and spicy foods. During treatment, canned food, pickles, smoked foods, fatty fish and meats, rich soups and broths are prohibited. Citrus fruits, chocolate, black tea, coffee, lemonade, and kvass contribute to erosion. The diet excludes sauces and seasonings.
Food should be boiled or steamed. Overeating is unacceptable; you should eat small meals, at least 5 times a day.
The diet includes:
- puree soups;
- lean meats, liver;
- omelet, soft-boiled eggs;
- dried white bread, biscuits;
- boiled potatoes, carrots, pumpkin, zucchini, beets, broccoli, cauliflower;
- rice, buckwheat, oatmeal;
- jelly, marshmallows, soufflé, marmalade;
- unsalted butter;
- mild cheese.
Drinks allowed are kefir, milk, rose hip decoction, and herbal teas. The diet does not provide for fresh fruits, with the exception of bananas. You can eat baked apples and pears. The disease in the acute stage requires an even more strict diet. When erosion is affected, the pain intensifies. During treatment, food is taken only in liquid or pureed form; bread is prohibited.
Forecast and prevention of erosive lesions
To get rid of erosion in the esophagus, as well as to prevent its occurrence, you should follow a number of recommendations. Prevention includes:
- rejection of bad habits;
- body weight control;
- sleeping with the head of the bed raised;
- eliminating abdominal exercises and forward bends;
- Limiting heavy lifting;
- eating 2-3 hours before bedtime;
- Belts and corsets that compress the body should be abandoned.
If treatment is started in a timely manner and diet is followed, the prognosis is favorable. Erosion in the esophagus lasts for 7-10 days. However, if you do not change your lifestyle and habits, a relapse is possible. In difficult cases, the disease has to be fought for weeks, and a long course of PPIs is prescribed. If treatment of erosion does not produce results, surgical intervention is indicated.