27.02.2020 09:00
1788
Erosion refers to open wounds located on the walls of the stomach. It is easy to guess that if spicy or hard-to-digest foods come into contact with injured areas, they will cause inflammation and bleeding, accompanied by severe pain. Therefore, during the period of activation of erosive gastritis, it is so important to choose the right diet.
Author: Ashurbekova Shamsiyat Tofikovna
Erosion refers to open wounds located on the walls of the stomach from the inside. It is easy to guess that if overly spicy or difficult-to-digest foods come into contact with injured areas, they will cause inflammation and bleeding, accompanied by severe pain. Therefore, during the period of activation of erosive gastritis, it is so important to choose the right diet.
Basic Rules
The main goal of a diet for gastritis is to adhere to a diet that ensures normal digestion. The treatment table for gastritis (per day) should contain:
- 90-100 gr. protein (and 60% are animals),
- 50-80 gr. fat (75% animal)
- 300-320 gr. carbohydrates.
Nutrition rules for gastritis:
- Knowing the measure. With gastritis, the saying “after eating there should be a feeling of slight hunger” is more relevant than ever. Firstly, the feeling of fullness occurs only 10-15 minutes after eating, and, secondly, a full stomach does not cope well with its functions, especially with gastritis.
- Diet. Firstly, you should follow a meal schedule (at the same time). Secondly, with gastritis, meals should be fractional, 4-5 times a day, but at the same time it is necessary to avoid snacks (they provoke “excess” secretion of gastric juice and reduce its production during breakfast/lunch/dinner, which disrupts processes of processing and assimilation of food). Reading while eating, watching TV and “eating while running” should be strictly excluded.
- Rest after eating. After each meal, you need to rest for 15-20 minutes (not necessarily sleep). You can read a book or listen to music.
- Chewing food. Chewing food for a long time (at least 25-30 seconds for each piece) promotes more thorough mechanical processing of food, which makes it easier for a sore stomach. In addition, hunger in this case is satisfied faster (which prevents overeating). Refusal of complex dishes
The total energy value should be 2200-2800 kcal.
What benefits does spinach bring to the body?
All vegetables, without exception, contain useful substances and vitamins - some in greater quantities, some in smaller quantities. Spinach falls into the first category. The concentration of beneficial microelements in it is truly impressive. First of all, carotene and provitamin A, which help restore the mucous membrane. Secondly, a rare vitamin PP. It is responsible for cellular energy, strengthens the immune system and activates carbohydrate metabolism.
How to achieve maximum preservation of the beneficial properties of spinach? Doctors recommend eating it in the form of a fresh salad. If necessary, blanch the spinach with a small amount of water during cooking.
Nutrition for high acidity
For this form of gastritis, it is recommended to use a diet aimed at thermal and mechanical sparing of the stomach, as well as at reducing gastric secretion.
Authorized products:
- casseroles, cheesecakes, dumplings, oven-baked cheesecakes;
- milk, especially with tea, all types of fermented milk products, including yogurt and curdled milk, fresh pureed cottage cheese;
- fish, meat or chicken soups cooked with cereal broth;
- white dry crackers, vegetable and butter, milk soups with cereals or pasta;
- steamed omelettes, eggs in a bag, vegetable dishes in the form of purees, puddings, souffles, weak tea, sweet fruits and berries in jelly, creams and compotes;
- veal, lean beef, chicken in the form of meatballs, puddings, zraz, steam cutlets (it is allowed to eat lean boiled meat in pieces 1-2 times a week).
Prohibited products:
- fatty mushroom and meat broths;
- carbonated drinks;
- smoked meats with spices;
- raw vegetables, pickles, marinades, spicy vegetable snacks, lemon juice;
- black bread.
The purpose of the diet for exacerbation of gastritis with high acidity is to normalize the functioning of the intestines and stomach, limiting thermal, chemical and mechanical irritants.
What's better to marinate in?
In this regard, most people have a question: how not to harm your health in the process of preparing fried meat? The answer is simple - prepare the right marinade. It partially eliminates the potential harm that fried meat can bring to a person. Instead of sour vinegar, use softer kefir or mineral water.
The meat is thoroughly soaked in the marinade for several hours. This will preserve the maximum amount of nutrients. If pork or chicken is marinated correctly, the marinade has a protective function. It prevents microbes from entering the meat and prevents their further reproduction.
So, let's summarize. Instead of traditional vinegar, we use kefir or mineral water as a base for the marinade. Consumption of prepared food should be in moderation. Even if the patient decides to allow himself a portion of kebab, it should be small (150-200 grams). Eat charcoal-cooked meat no more than once every two weeks. If there is an exacerbation, you will have to forget about the meat on skewers.
Nutrition for low acidity
The purpose of the diet for gastritis with low acidity is to stimulate (in moderation) the production of gastric juice, as well as to mechanically spare the stomach.
Prohibited foods for hypoacid gastritis:
- restriction of pearl barley, legumes, millet;
- fresh bread, rich pastries (“heavy” food for the stomach, makes chemical and mechanical processing difficult);
- fatty and salty fish;
- vegetables and fruits with coarse fiber (white cabbage, turnips, radishes, cucumbers, bell peppers), mushrooms;
- fatty meat, meat with fascia (films), canned food, smoked meats (inadequate mechanical processing of food, excess release of hydrochloric acid);
- sharp and salty cheeses, milk – neutralizes hydrochloric acid;
- berries with grains or thick skin (raspberries, strawberries, red currants, gooseberries, figs);
- spices and spices (irritate the gastric mucosa), as well as chocolate, grape juice, alcohol;
- lard and fat from pork, beef, lamb (not digestible due to low production of hydrochloric acid, difficult to digest foods).
Food should be taken after the secretion of hydrochloric acid begins, that is, in the first phase (advertising or programs about food, beautiful photographs of food, “delicious” conversations can provoke the release of gastric juice).
You need to know about this
The harmful properties of apples include the ability to destroy tooth enamel due to the high content of organic acids. However, if you rinse your mouth after eating apples, the enamel will not be destroyed. These same organic acids can cause exacerbation in a patient with gastritis or ulcers, because they are stimulants for parietal cells.
You should be careful when buying apples; it is better to choose domestic, regionalized varieties. Imported products are treated with chemicals for better storage, transportation and attractive appearance.
A huge red or green apple of ideal proportions can be harmful instead of beneficial and cause food poisoning. Therefore, our native fruits from our grandmother’s garden are much healthier than imported fruits.
Now let’s decide which varieties can be consumed by a patient with gastritis, and which ones it is better not to be tempted by. An important criterion for choosing products for gastritis is the acidity of the gastric contents.
Diet for gastritis in the acute stage
The diet for gastritis in the acute stage deserves special attention. The requirements for products are the same as for all types of this pathology, but more stringent.
In acute forms of the disease, it is recommended:
- low-fat cottage cheese;
- yesterday's white bread and no pastries or baked goods;
- only lean meat, boiled and pureed or finely chopped;
- soups made exclusively with vegetable broths;
- non-acidic compotes and jelly;
- soft-boiled eggs or in the form of a steam omelet;
- vegetable purees from the baby food range; it’s also a good idea to borrow fish and meat purees from a jar from your kids;
- teas or infusions without sugar.
During the period of immediate exacerbation, the following are completely excluded from the menu:
- products with preservatives, flavor enhancers, artificial colors;
- raw vegetables and fruits;
- milk and any dairy dishes;
- all types of baked goods, except day-old bread;
- margarine, cooking oil and butter;
- pearl barley;
- all types of beans and beans.
All general restrictions on the products themselves and methods of their preparation also remain in force. Usually, the crisis passes in 3-4 days, then the diet becomes more varied, in accordance with the general recommendations for patients with gastritis.
General rules
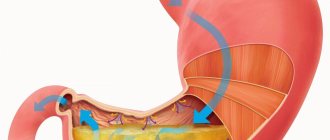
Erosive gastritis is an acute/chronic inflammation of the stomach, which is characterized by the formation of single/multiple erosions (ulcerations) of various sizes on the surface of the mucous membrane that do not penetrate into the deep layers of the stomach wall and heal without scar formation. It is the depth of the erosive defect that is the main distinguishing feature from gastric ulcer , in which the defect extends to the deeper layers of the stomach.
The clinical picture of the disease is polymorphic, but the main symptoms are “hungry” pain in the epigastrium, dyspepsia (dry/bitterness in the mouth, bloating, belching , discomfort/heaviness in the stomach), nausea, vomiting, constipation / diarrhea , blood in the vomit masses and stool.
Treatment of the disease is complex and is aimed at stopping the inflammatory process, reducing excess secretion and reducing the aggressiveness of gastric juice, normalizing the motor function of the stomach, and stimulating the regeneration of mucosal defects. Diet for erosive gastritis of the stomach is an essential component of therapy, however, if the etiological factor of the disease is the bacterium Helicobacter pylori, which is often the case if the antrum of the stomach is involved in the process, eradication therapy with antibiotics .
When diagnosed with erosive gastritis, diet and treatment are largely determined by the level of acidity of gastric juice. Since in the vast majority of cases, erosive gastritis occurs against the background of increased/normal acidity with increased secretory function, Table No. 1 according to Pevzner and its varieties are taken as the basis for therapeutic nutrition. Therapeutic nutrition is aimed at protecting the gastric mucosa from the effects of negative factors, reducing the activity of acid formation and excitability of the stomach, eliminating dyspeptic disorders/pain, and normalizing the motor function of the stomach.
In case of acute erosive gastritis or during an exacerbation of the chronic form, it is recommended to prescribe fasting on the first day, allowing the intake of only free liquid, if this does not increase pain, nausea and vomiting. On the second day, you are allowed to consume rice mucous soup, jelly, meat soufflé, and rosehip decoction.
On the third day, white crackers, vegetable puree, steamed cutlets/meatballs, and weak chicken broth are introduced into the diet. After relief of acute manifestations, the patient is assigned to the main Table No. 1 . In cases of acute, unrelieved symptoms, Table No. 1A , which provides for a maximum limitation of various types of effects on the gastric mucosa for a period of 7-10 days, after which the patient is transferred to treatment Table No. 1B , which is characterized by less pronounced restrictions for a period of 10-14 days and then on to Diet No. 1 .
Unlike Diets No. 1A and No. 1B, therapeutic Table No. 1 is physiologically balanced and complete in all food nutrients (90-95 proteins, 100 g of fat and 350-400 g of carbohydrates). The energy value of the diet is at the level of 2900-3000 kcal/day, which allows it to be prescribed for a long period (3-6 months). The basic principles of nutrition on the treatment table No. 1 are:
- Exclusion of products/dishes that stimulate secretion (concentrated meat/fish broths, mushrooms, smoked meats, coffee, carbonated drinks, alcohol), as well as all products that irritate the gastric mucosa (rough/fried foods, cranberries, salty, spicy, pickled dishes, onions, seasonings, radishes, citrus juices, garlic, ginger, radish, sour fruit juices) and products that promote gas formation processes (legumes, cabbage, kvass).
- Reducing animal fats in the diet (fatty pork, goose, duck, meat products). Butter is added only to prepared dishes.
- Reducing the volume of food per meal (no more than 250 g).
- Fractional meals (up to 6 times/day), ensuring better digestion of food and its absorption.
- Consume foods/dishes only when they are warm.
- Cooking methods - boiling, stewing/baking.
Gradually, the diet expands to the diet familiar to every person, but spicy foods, spices, herbs, smoked foods, pickles, canned food, fatty meat/fish products, and animal fats are still excluded. It is important to prevent the occurrence of complications of chronic erosive gastritis by switching from the usual diet to a dietary one when provoking factors appear (stress, exams, business trips).
Sample menu for the week
To get an impression of the diet, you can look at the approximate menu of the diet for gastritis of the stomach for a week with recipes. There is a clear fractional diet schedule: eating several times a day. This weekly meal plan is attractive and meets your energy needs thanks to its well-thought-out calorie content.
Day 1:
- Breakfast - buckwheat, milk soufflé, tea.
- Second breakfast - 1 glass of sweet oat broth.
- Lunch - slimy rice soup, spaghetti with beef zrazy, boiled carrots and peas, cocoa with milk.
- Afternoon snack - fermented milk cottage cheese.
- Dinner - vegetable casserole, steamed meatballs, light herbal decoction with honey.
- Before going to bed - 1 glass of fruit jelly.
Day 2:
- Breakfast - boiled egg, dried bread, boiled oatmeal, apple and rose hip decoction.
- Second breakfast - compote of boiled dried fruits (1 glass) and dry biscuit.
- Lunch - buckwheat soup, pumpkin puree, chicken zrazy, tea with milk (possibly adding sugar).
- Afternoon snack - 1 glass of milk, curdled milk, kefir and toast (fried bread is not allowed).
- Dinner - noodles with steamed beef patties, sour cream vegetable salad, cocoa. Before bed: 250 grams of low-fat fermented baked milk.
Day 3:
- Breakfast - oatmeal, boiled fish, tea with milk;
- Second breakfast - milk jelly.
- Lunch - vegetable soup with chicken, mashed potatoes and carrots, steam cutlet, cocoa with milk.
- Afternoon snack - fermented milk cottage cheese.
- Dinner - meatball with boiled peas, toast, dried fruit compote.
- Before bed - kefir or milk.
Day 4:
- Breakfast - fermented milk cottage cheese with honey, toast, dried fruit compote.
- Second breakfast - kefir or 1 glass of milk.
- Lunch - mashed potato soup, vegetable and rabbit casserole, dried fruit compote.
- Afternoon snack - milk mousse or soufflé with fresh fruit.
- Dinner - rice porridge with boiled rabbit, boiled carrots and peas, tea with milk.
- Before bed - cocoa with milk and 2 oatmeal cookies.
Day 5:
- Breakfast - boiled egg, dried bread, boiled oatmeal, cocoa with milk.
- Second breakfast - 1 glass of sweet oat broth.
- Lunch - pea soup, steamed fish, baked pumpkin.
- Afternoon snack - milk jelly.
- Dinner - vegetable casserole, steamed fish, rosehip broth.
- Before bed - 1 glass of kefir and oatmeal cookies.
Day 6:
- Breakfast - buckwheat milk groats, milk soufflé, tea.
- Second breakfast - baked fruit and a glass of milk.
- Lunch - pureed cauliflower soup, zrazy with rice, cocoa with milk.
- Afternoon snack - vegetable casserole and tea.
- Dinner - steamed fish with carrots and peas, salad with vegetables and sour cream, rosehip broth.
Day 7:
- Breakfast - baked apples with curd and raisin filling, toast, juice.
- Second breakfast - kefir or milk.
- Lunch - vegetable soup with chicken, mashed potatoes and carrots, steam cutlet, cocoa with milk.
- Afternoon snack - fermented milk cottage cheese with honey.
- Dinner - noodles with boiled chicken, baked pumpkin, cocoa with milk.
- Before bed - 1 glass of fruit jelly.
The acute stage of the disease with such nutrition will quickly go into the stage of remission of gastritis.
What cereals should you not eat during gastritis?
Gastroenterologists do not recommend consuming cereals with hard fibers during inflammation. Porridges are cooked in a certain way to preserve the benefits for the mucous membrane. The first dish should be moderately overcooked: overcooked cereal will cause smooth muscle spasms, flatulence, and bloating.
You should not eat instant cereals. They are not cooked enough and have coarse grains that mechanically irritate the mucous membrane.
You should consult your doctor before taking whole grain millet or oatmeal porridge. You can eat cereal without any problems.
Menu for the week, option No. 2
People who follow a diet for gastritis are advised to plan their menu for the week in advance with recipes. A clear action plan will help you avoid unhealthy snacks. It is much easier when the patient’s refrigerator is stocked with the necessary products. And the person knows how and what can be quickly prepared from them.
Monday:
- Morning - 7:00. Steamed fish cutlet. Boiled potatoes. Tea.
- Reinforcement - 10:00. Low-fat cottage cheese.
- Lunch - 13:00. Barley soup with vegetables. Buckwheat porridge with boiled meat. Compote.
- Reinforcement - 16:00. Sweet crackers. Carrot juice.
- Dinner - 18:30-19:00. Chicken meatballs baked in the oven. Mashed potatoes with water. Charlotte. Tea.
- At night - 21:00. A glass of low-fat kefir.
Tuesday:
- Morning - 7:00. Oatmeal with egg white omelette. Tea.
- Reinforcement - 10:00. Baked apples.
- Lunch - 13:00. Vegetable low-fat soup. Rice porridge with boiled chicken. Compote.
- Reinforcement - 16:00. Sweet crackers. Rosehip drink.
- Dinner - 18:30-19:00. Mashed potatoes with a piece of lean fish. Semolina pudding. Kissel.
- For the night. A glass of low-fat kefir.
Wednesday:
- Morning - 7:00. Rice porridge with turkey meatballs. Tea with milk.
- Reinforcement - 10:00. Cottage cheese casserole with low-fat sour cream.
- Lunch - 13:00. Vegetable soup. Rabbit meat cutlets steamed with vegetable stew. Compote.
- Reinforcement - 16:00. Sweet crackers. Rosehip drink.
- Dinner - 18:30-19:00. Oatmeal with half and half milk and chicken meatballs. Juice from fresh berries.
- At night - 21:00. A glass of low-fat kefir.
Thursday:
- Morning—7:00. Boiled tongue. Semolina porridge with half and half milk. Tea.
- Reinforcement - 10:00. Baked apple.
- Lunch - 13:00. Vegetable soup with small vermicelli. Mashed potatoes in water with boiled turkey meat. Compote.
- Reinforcement - 16:00. Galette cookies. Rosehip drink.
- Dinner - 18:30-19:00. Potato casserole with minced meat. Tea.
- At night - 21:00. A glass of low-fat kefir.
Friday:
- Morning - 7:00. Buckwheat porridge with protein omelette. Tea with milk.
- Reinforcement - 10:00. Kissel.
- Lunch - 13:00. Vegetable soup. Chicken meatballs with boiled vegetable puree. Compote.
- Reinforcement - 16:00. Sweet crackers. Dried fruits compote.
- Dinner - 18:30-19:00. Mashed potatoes in water with boiled fish. Tea.
- At night - 21:00. A glass of low-fat kefir.
Saturday:
- Morning - 7:00. Oatmeal with half and half milk. Steamed fish cutlets made from lean fish. Tea.
- Reinforcement - 10:00. Low-fat fresh cottage cheese. Baked apple.
- Lunch - 13:00. Vegetable soup. Boiled potatoes. Beef stroganoff. Compote.
- Reinforcement - 16:00. Sweet crackers. Tea.
- Dinner - 18:30-19:00. Fish baked in the oven. Boiled carrot puree. Tea.
- At night - 21:00. A glass of low-fat kefir.
Sunday:
- Morning - 7:00. Meat soufflé baked in the oven. Oatmeal with half and half milk. Tea.
- Reinforcement - 10:00. Carrot-apple soufflé.
- Lunch - 13:00. Vegetable rice soup. Buckwheat porridge with steamed rabbit meat cutlets. Carrot-banana juice.
- Reinforcement - 16:00. Sweet crackers. Tea.
- Dinner - 18:30-19:00. Mashed potatoes with water. Boiled fish. Rosehip drink.
- At night - 21:00. A glass of low-fat kefir.
How long should a diet be followed for gastritis? Strict control is necessary during exacerbation and in the first months after. But ideally, a patient diagnosed with gastritis should adhere to the recommended table during remission. Although, menu expansion and holiday exceptions are possible. If only within reasonable limits, and if we are not talking about coffee, cigarettes, alcohol and fatty foods.
How to cook and eat porridges that are healthy for the stomach
Before cooking any cereal or flakes, you must familiarize yourself with the cooking rules. A healthy recipe helps to get a healthy dish for a patient with gastritis. Cereals (flakes) of each type are cooked differently: the volume of water, milk, quantity of product, and production time change.
Millet porridge
You are allowed to cook millet porridge no more than 2 times a week. Cereals are nutritious, quickly saturate the body, but are difficult to digest. It is advisable to consume wheat flakes.
To prepare you will need:
- wheat flakes – 1 cup;
- water – 3 glasses;
- salt - a pinch;
- sugar – 1 teaspoon.
Stages of preparing a dish from wheat flakes.
- Pour 3 glasses of water into the prepared dishes.
- Cook until boiling.
- Add 1 cup of wheat flakes to boiling water.
- Cook over low heat, stirring.
- Sugar and salt to taste.
Cooking time – 20-30 minutes.
Wheat flakes are easy to use because of the minimal cooking time. If you use cereal, you need to cook it according to a similar recipe, but the cooking time changes - 45 minutes.
Oatmeal
Oat dishes are an important element of many diets. It is advisable to cook oatmeal. They will give the finished product the desired slimy texture.
For porridge you will need:
- water – 1 liter;
- salt and sugar to taste;
- oatmeal – 1 cup;
- butter.
Step by step recipe.
- Pour oatmeal into previously prepared boiled water.
- Cook over low heat until desired thickness.
- Add salt, sugar or honey to taste.
- Remove from heat and cover with a lid for 15 minutes to allow the dish to steep.
- Add oil.
Cooking time – 15-20 minutes.
Semolina
Cereals are easy to prepare if you follow the established proportions. The dish should be slimy and liquid. You should not cook thick semolina if you have inflammation of the gastric mucosa.
Required ingredients:
- water – 1 glass;
- sugar and salt to taste;
- semolina – 2 tbsp. spoons;
- butter.
It’s not difficult to remember how to prepare a dish.
- Pour water into the prepared container and place it on the stove.
- Wait until the water boils.
- Add semolina to boiling water, gradually pouring in the cereal and stirring the contents with a spoon.
- Cook over low heat, stirring continuously.
- Add salt, sugar or jam to taste.
- After removing from the stove, add a little oil.
Cooking time – 5 minutes.
Can I...?
What is possible and what is not? List of basic foods and drinks.
- Fish - only low-fat types of sea fish, such as pollock, cod, hake. Among river fish, pike perch and pike are the best. It is better to avoid canned fish and fried fish altogether; during their production, all the beneficial properties of any fish are lost, and you can more than get a lot of spices, preservatives, and carcinogens. Like meat, it is better to steam fish, limiting the spices.
- Coffee - you should absolutely not drink black coffee if you have gastritis on an empty stomach, even in large quantities, especially with increased stomach acidity. With low acidity, coffee or cocoa with milk is allowed, but only in limited quantities.
- Meat - you can eat with gastritis, but only low-fat varieties - beef, veal, chicken, rabbit. Steamed cutlets are especially useful for gastritis, since the meat is finely chopped and steamed. If it’s just steamed meat, then you should chew it very carefully and not overuse the quantity, since any meat product is a burden on the stomach. Naturally, neither smoked nor raw smoked sausages and sausages should be consumed if you have gastritis.
- Cheese - sharp or too salty cheeses are not allowed for any gastritis; even ordinary hard cheese should be consumed in limited quantities in small slices.
- Bananas – Can you eat bananas if you have gastritis? This is a healthy fruit that contains a little fiber, it is soft, easily digestible and contains a lot of useful substances that the body needs. And although diet No. 5 prohibits fruits such as dates and bananas, many gastroenterologists believe that their moderate consumption cannot harm and bananas should and can be eaten for gastritis.
- Watermelon is something you can eat if you have gastritis, but only a little bit. Regardless of acidity, you can eat only 1-2 slices.
- Melon is almost the hardest plant product not only for the stomach, but also for the pancreas and gall bladder. The gastrointestinal tract of even an absolutely healthy person has a hard time dealing with melon, so anyone who suffers from gastritis should avoid such a dubious product.
- Chocolate - it is better to avoid this product completely.
- Nuts, seeds, legumes - no types of nuts should be consumed if you have gastritis, the same goes for seeds and legumes.
- Honey can be consumed because it has wound-healing properties and is considered a fortified and healthy product. However, everything is good in moderation, especially since many people may be allergic to bee products.
Is it possible to completely get rid of gastritis?
In mild cases, with superficial gastritis, it is possible to cure it completely if you lead a healthy lifestyle and follow the following strict rules, which in practice turns out to be quite a difficult task:
- Meals should be 5-6 times a day, at certain hours, the last meal should be at least 2 hours before bedtime.
- Constant adherence to a diet, no dry food, no fast food.
- Avoid smoking and drinking alcohol.
- Avoid any overeating and long breaks in meals.
- No physical overexertion, constantly monitor the condition of the body, do not overwork, do not overstrain, sleep at least 8 hours a day at night and preferably 1 hour during the day.
It is also worth working on yourself to develop resistance to stress (stress tolerance), or to eliminate psycho-emotional overload.
Dish recipes
It is not recommended to buy ready-made mixtures for making jelly in stores, which include dyes, preservatives and other chemical additives. Jelly from frozen fruits. Put washed cherries (about 300 g) and cranberries (200 g), add 6-7 tbsp. sugar and add water (liter). Cook for two hours. At this time, dilute the starch in water and gradually add to the jelly. In a few minutes the jelly is ready.- Salmon soup. The tail must be washed and placed in a pan and filled with water. Bring to a boil, skim off the foam and add a peeled onion and a few bay leaves to the broth. Salmon does not take long to cook. While the broth is cooking, peel the potatoes and cut them into large cubes. Carrots also need to be cut into thick slices. Place the tail, discard the onion and bay leaves. Add prepared vegetables, salmon steak and a few peppercorns to the boiling broth and cook until tender, about 20 minutes. The dish is ready and can be served.