Gastritis associated with Helicobacter Pylori: what is it?
Hp-associated gastritis (inflammation of the gastric mucosa) is a disease caused by the presence and activity of the bacterium Helicobacter Pylori in the stomach.
Hp-associated gastritis (inflammation of the gastric mucosa) is a disease caused by the presence and activity of the bacterium Helicobacter Pylori in the stomach. According to statistics, about 50% of the total population of the Earth is infected with this microorganism, and in some regions this figure reaches 80-90%.
In addition to the fact that inflammation of the gastric mucosa causes many unpleasant symptoms, it disrupts the digestive processes and absorption of nutrients. But the greatest danger is hp-associated gastritis with this bacterium, from the point of view of forecasts: according to various estimates, peptic ulcer of the stomach and/or duodenum develops in 15-24% of patients, and not much less often inflammation leads to atrophic processes in gastric mucosa - one of the predisposing factors for cancer.
Therefore, gastritis caused by Helicobacter Pylori requires timely and professional treatment - this will restore health and quality of life, and also protect against possible complications.
At the First Family Clinic of St. Petersburg, highly qualified specialists, modern diagnostic facilities and individual therapy programs are waiting for you, which together makes the treatment of gastritis the most comfortable and effective process.
Causes
Attention! Helicobacter pylori can be transmitted from one person to another due to violations of personal hygiene rules!
Helicobacter pylori produces highly active enzymes urease, catalase, and mucinase, which lead to changes in the qualitative characteristics of gastric juice. Helicobacter pylori, upon penetration into the pyloric part of the stomach, in which there is a high content of urea, creates an alkaline environment, converting urea into ammonia, which leads to the launch of the mechanism of infection pathogenesis: destructive processes at the molecular, cellular and tissue levels, cytotoxic effects, impaired secretion, compensatory reactions of the glands, an intense inflammatory reaction with a predominance of neutrophil infiltration and a large number of plasma cells producing IgA in the mucosa.
Predisposing factors:
- Dietary disorders and poor nutrition.
- Smoking.
- Alcoholism.
- Psychologically severe, stressful conditions.
Antral gastritis HP – associated (type B)
The primary treatment tactics are effective eradication of HP in the gastric mucosa, stabilization of the general status of the patient and prolongation (lengthening) of the remission period. The European Association of Gastroenterologists Maastricht II (2000) recommended that targeted eradication of HP be carried out only in patients with atrophic gastritis.
The average duration of eradication therapy is from 7 to 14 days and directly depends on the HP status:
- Degree of infection;
- Activity of urease test;
- The activity of the inflammatory process.
The combination of drugs is usually three-component and includes, in addition to a proton pump inhibitor (the main representative is omeprazole), two combined antibacterial drugs:
- clarithromycin and amoxicillin, or:
- furazolidone and clarithromycin.
The primary treatment tactics are effective eradication of HP in the gastric mucosa, stabilization of the general status of the patient and prolongation (lengthening) of the remission period.
Doses are selected individually depending on many factors: age, weight of the patient, life history, allergic disease. A sharply reduced secretory function in a patient predetermines the prescription of a bismuth drug instead of a secretion inhibitor - de-nol 240 mg twice a day. In addition, it has antioxidant and antibacterial properties. Evaluation of the effectiveness of the therapy should be carried out no earlier than a month to a month and a half after its completion.
If the patient suffers from herpesvirus infection type 4 in the acute stage, amoxicillin is not prescribed. It is possible to include an antiviral drug in the treatment regimen.
If the first line of therapy is ineffective, it is necessary to prescribe four-component therapy. Typically, tetracycline is added to the treatment regimen at a therapeutic dose. The ideal option is to prescribe antibacterial therapy after determining the sensitivity of HP to it.
The principles for prescribing symptomatic drugs are as follows:
- Prokinetics (Motilak).
- Preparations that adsorb excess gas in the intestines (silicon containing).
- Normalization of dysbiosis (probiotics and eubiotics).
Bifidumbacterin, subalin, bifiform, biosporin have proven themselves very well.
If the secretion of hydrochloric acid is reduced, the following is included in treatment:
- plantaglucide 1 g twice a day before meals;
- plantain juice 15 ml 2-3 times a day, it also has good reparative and anti-inflammatory properties;
- delicious bitters.
Among the herbal remedies that alleviate flatulence, you can prescribe romazulan or a special carminative mixture containing several herbs with a similar effect. Acidinpepsin, betacid, abomin or pepsidil are the first-line drugs prescribed for replacement therapy for achylia. For the same purpose, it is necessary to prescribe drugs containing a set of various pancreatic enzymes: digestal, pankurmen, solizym, pancitrate, etc.
A very effective and at the same time safe method of treating chronic atrophic gastritis, which is best used not as monotherapy, but in combination with other drugs prescribed by the attending physician, is the daily use of propolis for one month in a dose of approximately 10 grams. Necessary condition: thorough chewing of propolis.
Helicobacter-associated gastritis is a disease that requires a professional approach to treatment
Treatment of other forms of chronic gastritis
For all other forms of this disease, symptomatic treatment is carried out using the following drugs:
- For ulcerative dyspepsia
:
- gastrocepin 25–50 mg 2 times a day
- Maalox (Gastal, Remagel, Phosphalugel, etc.) 2 tablets or 15 ml an hour after meals
:
The duration of inpatient treatment is 10 days. Requirements for treatment results:
- absence of symptoms, endoscopic and histological signs of inflammatory activity and infectious agent (complete remission);
- cessation of pain and dyspeptic disorders, reduction of histological signs of process activity without eradication of HP.
Helicobacter-associated gastritis: symptoms
Self-treatment of Helicobacter Pylori-associated chronic gastritis is impossible: to eliminate the infection and the damage it has caused to the stomach, the participation of qualified and experienced specialists and the use of the latest generation medical equipment is required. Therefore, if you have one or more of the following symptoms, be sure to consult your doctor:
- pain in the upper abdomen, which can occur both immediately after eating and 1-2 hours later;
- stool disorders, expressed in a tendency to constipation at the initial stage of the disease, and as it develops - in alternating constipation and diarrhea;
- heartburn and/or frequent belching with a sour taste;
- dyspeptic syndrome (a feeling of rapid satiety, a feeling of heaviness in the stomach, a bursting sensation in the epigastric region);
- appetite disorders.
Helicobacter-associated gastritis is a disease that requires a professional approach to treatment. This is the only way it becomes possible to eliminate the cause of the problem and prevent the development of gastric ulcers or atrophic processes in its mucous membrane.
Treatment
Treatment is aimed at achieving remission of the disease and preventing further progression of atrophy and the development of complications
- Antacids (to normalize the acidity of gastric juice).
- Gastroprotectors (drugs that protect (envelop) the mucous membrane).
- Antimicrobials.
- Prokinetic drugs.
- Individual selection of diet.
Attention!
The selection of drug therapy should be made individually, taking into account the severity of the disease, the presence of concomitant diseases, the patient’s age and the risk of possible side effects.
We ask you not to self-medicate based on Internet data!
Branch phone:
+7 (495) 695-56-95
Alarming symptoms of associated Helicobacter gastritis
Helicobacter pylori - gastritis, which occurs from the harmful effects of this microorganism, has 3 stages of development, each of which is accompanied by certain symptoms.
Initial, having increased or (which is quite rare) normal acidity. It is characterized by the following general symptoms:
- Epigastric pain that occurs 2 hours after eating;
- Frequent belching with a sour taste, turning into heartburn;
- Stool disorders (tendency to constipation).
Appetite is generally not affected, only occasionally an increase is noted. With the advanced stage of Helicobacter gastritis, the signs are the same, only their manifestation becomes more acute.
Helicobacter pylori - gastritis, which occurs from the harmful effects of this microorganism, has 3 stages of development, each of which is accompanied by certain symptoms
But the last, chronic, stage of this Helicobacter-associated gastritis will already be characterized by signs of atrophy, manifested in the mucous membrane of the digestive organ. Among them, the most common symptoms are:
- Indigestion (heaviness in the stomach after eating even a small amount of food);
- Lack of appetite;
- The presence of diarrhea due to the fact that the barrier function of hydrochloric acid is impaired;
- Rotten-tasting belching and metallic taste in the mouth;
- Significant reduction in body weight.
The complaints of patients with Helicobacter pylori gastritis are completely similar to the complaints of patients with stomach ulcers. These are hunger pains that appear in the morning (on an empty stomach), frequent constipation, sour belching, heartburn. If you do not pay timely attention to them and do not begin the necessary treatment, the disease begins to progress very quickly.
In this case, the following signs of bacterial gastritis are added - nausea, mostly turning into vomiting and containing bloody inclusions, as well as bloating, which appears due to excessive gas formation caused by the activity of Helicobakter pylori.
If a person has at least one of the above signs, you should not hesitate to contact a specialist, and not attribute it to the fact that perhaps you have eaten something of insufficient quality, and you need to drink no-shpa to prevent unpleasant symptoms stopped.
Only timely diagnosis of the gastrointestinal tract for the presence of Helicobacter gastritis will allow taking all necessary measures in a timely manner and preventing the disease from progressing to a more severe stage. Modern research methods suggest an accuracy of determining HP gastritis of up to 99%.
Forecast, prevention, clinical observation
The prognosis for life with chronic gastritis is favorable.
Primary prevention is aimed at eliminating risk factors, bad habits, promoting a healthy lifestyle and a balanced diet. Secondary prevention is aimed at limiting the use of non-steroidal anti-inflammatory drugs, eliminating occupational hazards, identifying and treating diseases of other organs and systems.
Patients with active gastritis associated with HP, autoimmune gastritis and reflux gastritis are subject to dispensary observation. Patients with diffuse atrophic gastritis, hypertrophic with dysplasia and
Erosive gastritis nr associated gastritis
The disease can occur in acute or chronic form.
Considering the factors that cause associated diseases in the chronic stage, primary and secondary types of associated diseases are distinguished. Diseases of the digestive tract disrupt the normal functioning of the body. The gastrointestinal tract is of great importance to the body, and inflammation can lead to complications if timely treatment is not started. It is extremely important to consult a doctor in time to carry out the necessary treatment complex. One of the most common diseases is associated gastroduodenitis, which is a type of gastroenteritis. Frequent diagnosis of associated gastroduodenitis is associated with constant contact of the duodenum and stomach. When an illness occurs, the patient's duodenal mucosa becomes inflamed.
The disease can occur in acute or chronic form. Taking into account the factors that cause associated diseases in the chronic stage, primary and secondary types of associated diseases are distinguished. The appearance of the primary type is characteristic of impaired digestion, which occurs due to an incorrect diet. The secondary type may appear as a consequence of other diseases, for example, gastritis, pancreatitis, etc.
There are several classifications of HP associated gastroduodenitis. In the presence of a certain level of acidity, types such as normal gastroduodenitis, an associated disease with a decreased or increased level of secretory function, are distinguished.
The appearance of gastroduodenitis is associated with the proliferation of the bacterium helicobacter pylori. Helicobacter is the cause of the disease in 80% of cases.
In advanced stages, it is impossible to determine the presence of Helicobacter, because the digestive environment becomes unsuitable for its existence. A properly formulated diet, an active lifestyle, and giving up bad habits are the main points necessary to maintain health and prevent the occurrence of inflammatory processes in the digestive tract. If unpleasant signs appear with associated gastroduodenitis, you should immediately consult a doctor to avoid complications.
Inflammatory processes at the initial stage can be characterized by such signs as:
- the appearance of heartburn, belching with a sour smell;
- increased appetite;
- pain in the area under the stomach that appears 2 hours after eating;
- Constipation may occur.
In advanced stages, it is impossible to determine the presence of Helicobacter, because the digestive environment becomes unsuitable for its existence.
The initial stage is most often characterized by an increased level of acidity. But in the last stages of the disease, the patient experiences atrophy of the gastric mucosa. This manifests itself in the development of symptoms such as:
- loss of appetite;
- a feeling of heaviness in the stomach area resulting from undigested food;
- dull pain in the gastric area;
- reduced barrier function of hydrochloric acid leads to diarrhea;
- the appearance of a metallic taste;
- the manifestation of belching, which may have the smell of consumed food, and sometimes has a rotten character;
- sudden weight loss;
- Cracks may appear in the corners of the mouth, which are called jams;
- the appearance of nausea.
If Helicobacter has spread to the duodenum, the patient begins to experience the following symptoms:
- a feeling of bitterness in the mouth, which may be accompanied by belching of bile;
- the appearance of nausea and vomiting;
- pain in the area of the right hypochondrium.
Treatment of reflux gastritis
The goal is to normalize gastrointestinal motility and bind bile acids.
To normalize motor function, prokinetics are prescribed. Dopamine receptor blockers have these properties: metoclopramide (Raglan, Cerucal), motilium (domperidone); cholinergic receptor stimulants: coordinax (cisapride). They increase pyloric tone and intragastric pressure, increase propulsive clearance of contents from the stomach, and eliminate the symptoms of dyspepsia.
An important place in treatment is occupied by antacids, mainly non-absorbable (Maalox, phosphalugel, gastal, etc.), which reduce the aggressive properties of intestinal contents and protect the gastric mucosa by binding bile. Sucralfate (Venter) is also prescribed 1.0 g orally 3 times 30 minutes before meals and at night. The drug, combining with protein, forms a protective layer on the mucous membrane, prevents the action of aggressive factors, and absorbs bile. If ineffective, surgical treatment is indicated.
Features of the course of gastritis associated with HP
The main symptoms of chronic gastritis are dyspeptic disorders. Patients complain of nausea, heaviness in the stomach after eating, belching, heartburn, and rumbling in the stomach. A characteristic symptom of gastritis associated with HP is stool disorder: pasty stool, imperative urge to defecate. Abnormalities in bowel movements are intermittent, but they make themselves felt. Less common is bitterness and burning in the mouth, and belching of air. Chronic gastritis can cause symptoms such as weakness, irritability, increased fatigue, and loss of interest in what is happening. Such symptoms are called “general” and are characteristic of many infectious diseases.
Additional treatments
Physiotherapeutic methods of treatment are used as additional ones. They normalize the motor and secretory functions of the stomach, reduce inflammation, and improve blood circulation. Electrophoresis with novocaine, platiphylline, dia-dynamic and sinusoidal modulated currents are used, and during the period of remission - thermal procedures (paraffin and ozokerite applications, peloid therapy). To stimulate the glands in gastritis with reduced secretory function, microwave therapy in the decimeter range and sinusoidal modulated currents, inductothermy of the adrenal zone are used.
Sanatorium-resort treatment includes nutritional therapy, climate therapy, and balneotherapy. It is better to send patients with increased secretory function to resorts with alkaline mineral waters (Borjomi, Zheleznovodsk, etc.), patients with decreased secretory function to resorts with salt and saline-alkaline mineral waters (Essentuki, Staraya Russa).
However, now less importance is attached to the characteristics of mineral water; the time of its use relative to food intake is more important. It is recommended, given the general pattern, to take mineral water 15–20 minutes before meals, which stimulates secretion, or 0.5–1.5 hours before meals, which blocks gastric secretion.
Diagnosis of Helicobacter gastritis: gastroscopy, biopsy, helic test
In addition to standard methods of examining the patient (blood tests, urine tests, stool tests, ultrasound of internal organs), if chronic gastritis of a bacterial nature is suspected, gastroscopy is mandatory. The stomach is examined through a probe with a lighted camera at the end. Changes in the gastric mucosa are assessed, its surface is examined for the presence of erosions, ulcers, and neoplasms.
During gastroscopy, a biopsy of tissue from different parts of the stomach is performed. The resulting samples are sent for microscopic examination. Using a special staining of the preparations, the doctor can determine the presence of Helicobacter pylori in the patient's stomach under a microscope. A simpler and more accessible method is to conduct a helic test (urease breath test). This is an absolutely painless test based on the ability of the HP bacterium to exhibit urease activity. The patient drinks a urea solution and then breathes through a special tube with an indicator. As a result of the hydrolysis reaction, gas is released, which is noted in the tube by a change in color.
Treatment of drug-induced chronic gastritis
The goal is to increase the protective properties of the mucous membrane.
First of all, it is necessary to discontinue non-steroidal anti-inflammatory drugs, which can lead to regression of inflammation in the stomach. Of the medications, the most important are synthetic prostaglandins, which improve microcirculation and promote the formation of surfactant-like compounds: misoprostil (Cytotec) is prescribed 200 mcg 3-4 times with meals and at night. In addition, proton pump blockers are indicated: omeprazole (Omez, Losek, etc.), histamine H2 receptor blockers (ranitidine, famotidine) and antacids.
Types of schemes
For the treatment of Helicobacter pylori infection, 1st and 2nd line drugs are used, and each regimen can have a three-component or four-component composition.
First line
A three-component treatment regimen for Helicobacter pylori eradication includes taking the following medications:
- One of the proton pump inhibitors in standard dosage (Pantoprazole, Lansoprazole, Omeprazole, Rabeprazole, Esomeprazole).
- Metronidazole or Amoxicillin.
- Clarithromycin.
The effectiveness of a three-component eradication scheme can be enhanced by increasing its duration to 10-14 days.
Helicobacteriosis (Helicobacter pylori, Helicobacter pylori infection, Helicobacter pylori, H. pylori)
Gastritis
Ulcer
Iron deficiency
Vomit
Diarrhea
28205 January 28
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Helicobacteriosis: causes, symptoms, diagnosis and treatment methods.
Definition
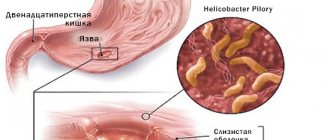
Helicobacteriosis is an infectious disease that affects the pylorus of the stomach, or pylorus, and duodenum. Its causative agent is a unique pathogenic microaerophilic gram-negative bacterium Helicobacter pylori (H. pylori). The bacterium got its name from the section of the stomach in which it lives - the pyloric.
As a result of its vital activity, H. pylori forms a “cloud” of alkaline environment around itself, which allows this bacterium to survive in the aggressive acidic environment of the stomach, causing accelerated secretion of hydrochloric acid, as well as a decrease in alkali secretion in the duodenum.
As a result, the microorganism further colonizes the mucous membrane, forms its increased susceptibility to hydrochloric acid and provokes inflammation, leading to the development of ulcerative defects.
Helicobacter pylori is a spiral-shaped bacterium 3.5 microns long and 0.5 microns wide. It has flagella, with the help of which it moves freely along the wall of the stomach or is securely attached to it. The bacterium H. pylori is very variable; its strains (varieties) differ from each other in their ability to attach to the gastric mucosa, cause an inflammatory process, and have varying degrees of pathogenicity.
Helicobacter pylori, which colonizes the gastric mucosa, is a common cause of its inflammatory changes; it is recognized as the etiological factor of gastritis, and gastritis itself is an infectious disease. Depending on the state of the protective factors of the stomach, the resulting infectious process can occur latently or with severe clinical symptoms of inflammation. According to modern concepts, H. pylori causes chronic gastritis in all infected individuals. This can lead to peptic ulcer disease, atrophic gastritis, gastric adenocarcinoma or low-grade gastric lymphoma. H. pylori is a first-order carcinogen.
The results of numerous studies suggest a possible pathogenetic or indirect role of H. pylori infection in the development and/or course of diseases not related to digestion: cardio-, cerebrovascular, autoimmune diseases, diseases of the blood, skin, nervous system and many others.
The pathogen is relatively resistant to the environment: when boiled, Helicobacter bacteria die almost instantly, and when treated with disinfectant compounds, they die within a few minutes.
Causes of helicobacteriosis
You can become infected with the bacteria through contact with contaminated water or food. Infection is possible during endoscopy and when using other poorly sterilized medical instruments that have had direct contact with the patient’s gastric mucosa.
Household transmission (for example, through kisses, personal belongings, etc.) is also possible, as evidenced by the release of bacteria from saliva and dental plaque.
The prevalence of infection varies depending on the geographic region, patient age, ethnicity, and socioeconomic status. According to the Moscow Department of Health (2019), the prevalence of this infection in Moscow is 60.7–88%, in St. Petersburg - 63.6%, in Eastern Siberia reaches 90%.
Classification of diseases
Diseases associated with H. pylori:
- gastritis,
- duodenitis,
- gastroduodenitis,
- esophagitis,
- stomach ulcer,
- duodenal ulcer,
- iron deficiency anemia of unknown origin,
- stomach cancer,
- duodenal cancer.
Symptoms of Helicobacteriosis
The main manifestation of Helicobacter pylori is chronic inflammation of the stomach. In the case of rapid primary manifestation of the pathogen, the acute period of helicobacteriosis lasts about 10 days. The general condition of patients usually remains satisfactory, sometimes there is a short-term low-grade fever and decreased performance.
The main complaint with which patients with signs of Helicobacter infection consult a doctor is stomach pain. The localization of the symptom may change and move to the area of the duodenum.
The pain can be sharp, aching, dull, and occurs in the upper abdomen on the left and in the center in the umbilical region. Discomfort can occur during prolonged fasting, on an empty stomach, or after a certain time after eating.
Symptoms of helicobacteriosis depend on the clinical form of the disease and may include:
- feeling of heaviness in the stomach after eating;
- loss of appetite associated with sudden attacks of nausea (if the gastric mucosa is severely injured);
- causeless vomiting against the background of normal body temperature;
- heartburn (burning sensations in the esophagus and even larynx) and belching with an unpleasant sour or bitter taste;
- chronic constipation (lack of bowel movements for three days or more);
- liquefaction of stool, the appearance of a foamy or watery consistency;
- intestinal cramps and bloating.
If there is a strong contamination with Helicobacter, a number of atypical symptoms may occur, which indicate significant infection and progression of the disease:
- loss of appetite to its complete absence;
- nausea may be replaced by vomiting with blood clots;
- a sharp decrease in body weight that is not normal;
- dry mouth and metallic taste;
- the appearance of a white coating on the tongue;
- bad breath in the absence of caries;
- seizures in the corners of the mouth;
- bleeding gums.
In the chronic course of the disease and atrophic damage to the gastric mucosa, signs of iron deficiency anemia appear - frequent headaches and dizziness, pallor of the skin, decreased blood pressure and tachycardia.
Diagnosis of helicobacteriosis
For a long time, helicobacteriosis may not manifest itself in any way, while provoking the development of ulcers, adenocarcinoma or gastric maltoma. People whose relatives have a history of these diseases are at particular risk.
Diagnosis can be invasive (endoscopy followed by biopsy of gastric tissue) and non-invasive (laboratory tests).
According to international recommendations, the methods of choice for diagnosing the bacterium and assessing the effectiveness of treatment for H. pylori are a breath test with 13C-labeled urea and determination of specific H. pylori antigens in stool using an immunochromatographic method.