Causes
Diarrhea with mucus is a symptom whose appearance indicates damage to the digestive system. Excessive mucus secretion is characteristic of diseases of the large intestine - colitis. This is due to the fact that in the wall of the colon there are many more goblet cells, which are responsible for the production of mucous secretion1.
The causes of diarrhea with mucus in a child can be divided into infectious and non-infectious2.
Up to contents
Infectious causes
Intestinal infections last 1-3 weeks2. Infectious factors include viruses, bacteria and pathological fungi that affect the intestinal mucosa and cause diarrhea2. Also, often mucous diarrhea is a manifestation of the active activity of parasites in the intestines2. In addition to mechanical injury to the intestinal wall, worms can have a toxic effect on the body with the substances they secrete. Parasites can provoke allergies and maintain constant inflammation in the gastrointestinal tract9.
Depending on the mechanism of development, the following types of diarrhea are distinguished:
- Secretory . The basis of diarrhea of secretory origin is enteritis - damage to the wall of the small intestine, primarily of viral origin. With this pathology, stool becomes liquid and watery14.
- Invasive diarrhea. Invasive is associated with damage to the large intestine by pathogenic bacteria - for example, Salmonella, Shigella or Escherichia. They penetrate the intestinal wall and cause active inflammation - colitis, which is manifested by the appearance of diarrhea with mucus14
It is the large intestine that normally ensures the formation of stool, so disruption of its function leads to the appearance of loose stools with abundant mucus1.
Up to contents
Non-infectious causes
Non-infectious diarrhea lasts more than 3 months and becomes chronic2.
Mucous diarrhea in a child often occurs as a result of an allergic reaction2,11. In young children, the main food allergens are cow's and goat's milk proteins. The list of allergens is expanding as new dishes are introduced; schoolchildren and teenagers are often allergic to eggs and gluten-containing products10. Food allergies can be triggered by an unbalanced diet, frequent or, conversely, too infrequent meals11.
Liquid, light stool mixed with mucus and blood is observed in the following cases2:
- Ulcerative colitis is a disease in which active damage to the mucous and submucosal layer of the large intestine occurs with the formation of ulcers. It is based on a disruption of the body’s immune response, which leads to chronic inflammation16.
- Crohn's disease is a long-term pathology that occurs with exacerbations. Unlike ulcerative colitis, this disease can affect all parts of the digestive system. In children and adolescents, the disease begins in the large intestine. In this case, chronic inflammation affects all layers of the intestinal wall16,17.
- Juvenile polyposis is the formation of multiple polyps in the small and large intestines, in which epithelial glands that produce mucus are actively working5.
Up to contents
Irritable bowel syndrome
Another cause of diarrhea in children and adolescents is irritable bowel syndrome. It develops due to a functional disorder of the digestive system. In this case, the child usually experiences mucous diarrhea with particles of undigested food1.
In most cases, symptoms appear in the morning, immediately after breakfast - for example, on the way to school. This phenomenon is called “morning rush syndrome.” In this case, the teenager first passes formed stool, then the stool becomes mushy or liquid feces are released. After bowel movements, the child feels well and, as a rule, diarrhea does not recur during the day1.
Up to contents
Antibiotic-associated diarrhea in children
It is customary to separately distinguish antibiotic-associated diarrhea - a bowel disorder that occurs while taking antimicrobial drugs or several months after a course of treatment2. When using drugs, the composition of the intestinal microflora is disrupted - dysbacteriosis develops. Against this background, clostridia actively multiply, and pseudomembranous colitis develops. Because of this, the child develops painful, repeated diarrhea with the release of mucus or blood6,15.
Up to contents
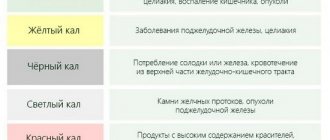
Red stool
Consumption of coloring products
Most often, the appearance of red feces in adults is associated with eating large quantities of foods of the corresponding color - beets, tomatoes, berries. The reddish tint of stool is caused by artificial dyes in candies and carbonated drinks. In this case, the stool has a normal consistency, the frequency of bowel movements does not change. There are no other unpleasant sensations from the gastrointestinal tract. Normalization of the color of stool occurs in 1-2 days.
Haemorrhoids
Blood from enlarged hemorrhoids is released in drops already at the beginning of the disease. In this case, the feces have a normal color, but red streaks become noticeable on its surface. The frequency of stool with hemorrhoids is reduced to 3-4 times a week, which is due to a reflex spasm of the rectal sphincter muscles. Characterized by pain in the anus, which sharply intensifies during defecation.
As the disease progresses and the venous nodes increase in size, hemorrhoidal bleeding becomes more frequent. The stool takes on a greasy or liquid consistency and a reddish color due to the large amount of blood. In severe situations, with ulceration of hemorrhoidal veins, profuse bleeding begins, in which the stool loses its fecal character, and bright red blood is released from the anus.
Other diseases of the rectum
The appearance of red inclusions in stool is caused by inflammatory causes. In acute erosive proctitis, blood is released from the affected mucous membrane, which stains the stool. In the case of a bacterial infection, stool of a liquid consistency with abundant bloody-purulent inclusions is observed. Patients also experience constant pain in the anal area, radiating to the perineum and sacrum.
Red stool is caused by anal fissures. They are characterized by severe sharp pain during bowel movements, followed by the appearance of stool mixed with blood. Symptoms often develop with prolonged constipation, when a person has to strain very hard, and dry, hard feces injure the intestinal mucosa. The formation of an anal fissure is possible in women after childbirth.
Infections
Red streaks in stool are a characteristic symptom of dysentery (shigellosis). Bacterial toxins cause damage to the intestinal walls, from which blood is released. At the beginning of the disease, the stool is liquid and has a fecal character with isolated bloody inclusions. In severe cases, the number of bowel movements increases to 10-12 times a day, stools are scanty in the form of mucus mixed with blood. Patients complain of severe cramps in the abdomen, especially in the left side.
Copious red stools sometimes occur at 3-4 weeks during the typical course of typhoid fever, which is associated with bleeding from a deep typhoid ulcer. Liquid, mucous stool with a lot of blood, like “raspberry jelly,” is a pathognomonic sign of amoebiasis. In addition to the reddish color of the stool, severe abdominal pain, nausea and vomiting are disturbing. With such symptoms, emergency medical care is indicated.
Inflammatory bowel lesions
In Crohn's disease and nonspecific ulcerative colitis, deep ulcerative defects are formed that bleed. Red stool is more common in UC because it causes damage to the distal bowel. Against the background of a painful imperative urge to defecate, the discharge of scanty feces with admixtures of scarlet blood is noted. Exacerbations are provoked by reasons such as stress, errors in diet, and concomitant intestinal infections.
Neoplasms
Occasionally, a reddish color of feces is observed with colonic polyps and other benign tumors, which eventually become covered with ulcers due to constant traumatization by hard feces. Red color of stool is more common with intestinal cancer tumors, since they ulcerate and disintegrate faster, involving blood vessels. I am concerned about dull pain in the abdominal cavity, prolonged constipation, and progressive weight loss.
Complications of pharmacotherapy
Most often, stool staining occurs during prolonged treatment with the anti-tuberculosis drug rifampicin. It is red in color and when it enters the body it turns into metabolites, which are excreted in different ways. Therefore, not only feces, but also urine, tear fluid, and sweat acquire a reddish color. Atypical coloring of stool is sometimes possible with long-term use of vitamin A in high doses, which contains carotene pigments.
Symptoms of diarrhea with mucus
Diarrhea is not an independent disease, but a separate symptom. When it appears, it is important for parents to pay attention to the frequency of stool in the child, its abundance and consistency.
Normally, a child over one year old should have stool no more than 1-2 times a day. Feces are usually dark brown, shaped, and hard. There should be no visible impurities. With diarrhea, the stool becomes thinner, sometimes to the point where there are no solid particles at all13.
Diarrhea with green mucus most often occurs due to a bacterial infection3. When the large intestine is affected, stools are usually repeated, but not too abundant. In addition to mucus, it sometimes contains blood or pus2,7.
Food allergies can manifest as colicky abdominal pain, frequent loose stools with the discharge of glassy mucus11. The persistence of loose stools is a reason to suspect more serious problems, primarily of a non-infectious nature2.
With an intestinal infection, diarrhea is accompanied by abdominal pain - usually it is quite strong and cramping. It is painful for the child to go to the toilet, sometimes he has a false urge to defecate - tenesmus3.
The situation requires close attention from parents if loose, mucous stools are accompanied by additional symptoms7:
- Vomiting of undigested food debris or bile, sometimes mixed with blood;
- Increased body temperature – fever;
- Chills and weakness;
- Rare urge to urinate;
- Flatulence - bloating;
- Body aches, muscle pain;
- Skin rash;
- Loss of appetite;
- Drowsiness or, conversely, emotional excitement;
- The stool is black.
With severe diarrhea, children become dehydrated and complain of extreme thirst. Due to malabsorption of nutrients due to diarrhea, the child loses weight7.
If episodes of diarrhea with mucus recur and are accompanied by other alarming symptoms, it is necessary to show the child to a pediatrician7. The doctor will make the correct diagnosis and prescribe adequate treatment.
Up to contents
Causes of red stool
Consumption of coloring products
Most often, the appearance of red feces in adults is associated with eating large quantities of foods of the corresponding color - beets, tomatoes, berries. The reddish tint of stool is caused by artificial dyes in candies and carbonated drinks. In this case, the stool has a normal consistency, the frequency of bowel movements does not change. There are no other unpleasant sensations from the gastrointestinal tract. Normalization of the color of stool occurs in 1-2 days.
Haemorrhoids
Blood from enlarged hemorrhoids is released in drops already at the beginning of the disease. In this case, the feces have a normal color, but red streaks become noticeable on its surface. The frequency of stool with hemorrhoids is reduced to 3-4 times a week, which is due to a reflex spasm of the rectal sphincter muscles. Characterized by pain in the anus, which sharply intensifies during defecation.
As the disease progresses and the venous nodes increase in size, hemorrhoidal bleeding becomes more frequent. The stool takes on a greasy or liquid consistency and a reddish color due to the large amount of blood. In severe situations, with ulceration of hemorrhoidal veins, profuse bleeding begins, in which the stool loses its fecal character, and bright red blood is released from the anus.
Other diseases of the rectum
The appearance of red inclusions in stool is caused by inflammatory causes. In acute erosive proctitis, blood is released from the affected mucous membrane, which stains the stool. In the case of a bacterial infection, stool of a liquid consistency with abundant bloody-purulent inclusions is observed. Patients also experience constant pain in the anal area, radiating to the perineum and sacrum.
Red stool is caused by anal fissures. They are characterized by severe sharp pain during bowel movements, followed by the appearance of stool mixed with blood. Symptoms often develop with prolonged constipation, when a person has to strain very hard, and dry, hard feces injure the intestinal mucosa. The formation of an anal fissure is possible in women after childbirth.
Infections
Red streaks in stool are a characteristic symptom of dysentery (shigellosis). Bacterial toxins cause damage to the intestinal walls, from which blood is released. At the beginning of the disease, the stool is liquid and has a fecal character with isolated bloody inclusions. In severe cases, the number of bowel movements increases to 10-12 times a day, stools are scanty in the form of mucus mixed with blood. Patients complain of severe cramps in the abdomen, especially in the left side.
Copious red stools sometimes occur at 3-4 weeks during the typical course of typhoid fever, which is associated with bleeding from a deep typhoid ulcer. Liquid, mucous stool with a lot of blood, like “raspberry jelly,” is a pathognomonic sign of amoebiasis. In addition to the reddish color of the stool, severe abdominal pain, nausea and vomiting are disturbing. With such symptoms, emergency medical care is indicated.
Inflammatory bowel lesions
In Crohn's disease and nonspecific ulcerative colitis, deep ulcerative defects are formed that bleed. Red stool is more common in UC because it causes damage to the distal bowel. Against the background of a painful imperative urge to defecate, the discharge of scanty feces with admixtures of scarlet blood is noted. Exacerbations are provoked by reasons such as stress, errors in diet, and concomitant intestinal infections.
Neoplasms
Occasionally, a reddish color of feces is observed with colonic polyps and other benign tumors, which eventually become covered with ulcers due to constant traumatization by hard feces. Red color of stool is more common with intestinal cancer tumors, since they ulcerate and disintegrate faster, involving blood vessels. I am concerned about dull pain in the abdominal cavity, prolonged constipation, and progressive weight loss.
Complications of pharmacotherapy
Most often, stool staining occurs during prolonged treatment with the anti-tuberculosis drug rifampicin. It is red in color and when it enters the body it turns into metabolites, which are excreted in different ways. Therefore, not only feces, but also urine, tear fluid, and sweat acquire a reddish color. Atypical coloring of stool is sometimes possible with long-term use of vitamin A in high doses, which contains carotene pigments.
How is the child examined?
In most cases, diarrhea with mucus does not require any specific examination7. The doctor assesses the child’s condition, examines him and, based on this, makes recommendations for treatment. To distinguish infectious causes of mucous diarrhea from non-infectious ones, the pediatrician prescribes laboratory tests and instrumental research methods4,7.
For a correct diagnosis, you should inform the doctor about the child’s eating habits, recently taken medications, and a tendency to allergies2.
Up to contents
Treatment
Treatment of diarrhea in a child should be carried out by a specialized specialist - a pediatrician or pediatric gastroenterologist. Only a doctor can adequately assess the severity of the patient’s condition and prescribe rational therapy.
If the disease is mild, the child is given more fluids to drink to quickly make up for the deficiency. If severe dehydration develops, hospitalization and intravenous saline solutions will be required3,7.
Diet therapy
In order for intestinal function to recover faster, it is important to monitor the child’s nutrition. If the diarrhea is mild and there are no signs of intoxication, in older children the amount of food should be reduced by 15-20%. The food must be well prepared; it is better to serve the dish pureed or mashed. From 3-5 days you can return to your previous diet. With moderate diarrhea, in the first days the amount of food is reduced by 20-30%, and over the course of 4-6 days they gradually return to the usual menu14.
It is advisable not to consume foods that increase diarrhea. Food containing soft fiber should be added to the menu14.
Diet for diarrhea with mucus in a child14
| Products to exclude | Recommended Products |
|
|
Up to contents