One of the most serious inflammatory bowel diseases is ischemic colitis. It is caused by damage to the vessels penetrating the abdominal cavity and often occurs in patients who have already been diagnosed with various diseases of the cardiovascular system.
This is a very dangerous disease , fraught with the development of serious, sometimes life-threatening, complications. If symptoms appear that may indicate the development of ischemic colitis, you should immediately consult a gastroenterologist. Our specialized gastroenterology and hepatology department sees patients daily.
Symptoms of ischemic colitis
It is impossible to make a correct diagnosis based on symptoms alone. The fact is that the symptoms characteristic of ischemic colitis may actually be signs of another disease of the gastrointestinal tract - for example, irritable bowel syndrome. That is why if the following symptoms appear, you should immediately consult a doctor:
- sudden attacks of acute abdominal pain that are recurring;
- incomplete absorption and breakdown of food;
- diarrhea and vomiting interspersed with mucus;
- bleeding from the anus, etc.
.
If qualified medical care is not provided on time, complications may develop, the most severe of which is gangrene with a fatal outcome.
Causes of development of ischemic colitis
The main cause of ischemic colitis is insufficient blood flow to a certain area of the intestine. Other diseases can provoke this condition.
| GreenFlames09 Flickr |
Due to what pathologies can ischemic colitis develop:
- embolism and vascular thromboembolism;
- atherosclerosis;
- intestinal infection with severe intoxication;
- severe anemia;
- tumors and hernias in the intestinal lumen;
- stroke;
- blood loss due to injuries, operations;
- systemic vasculitis;
- hypotension;
- heart failure accompanied by shock conditions;
- DIC syndrome, etc.
Ischemic colitis can also become a complication of reconstructive therapy after an abdominal aortic aneurysm.
Diagnosis of ischemic colitis
First of all, a gastroenterologist collects anamnesis during a face-to-face consultation, examines the patient and determines the severity of his condition. He may refer the patient for the following studies:
- endoscopic examination of the intestines;
- blood and stool tests;
- Doppler ultrasound;
- irrigoscopy, etc.
All examinations are performed in our medical center, which is equipped with all the necessary equipment. You can undergo a comprehensive examination in one day.
Clinical picture of mesenteric circulation disorder
Mesenteric circulation disorders can be acute or chronic. The first form, leading to the development of intestinal infarction, has more or less distinct symptoms and is correctly diagnosed in a significant number of cases [8]. As for the clinical picture of chronic disorders of the blood supply to the digestive organs, it is less defined, since it is similar to the clinical picture of a number of diseases of the gastrointestinal tract. The clinical manifestations of chronic ischemia of the digestive organs (CIOD) are extremely diverse; the disease has a lot of clinical “masks”.
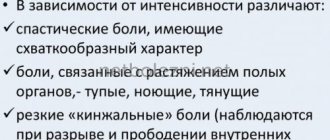
In 94–96% of patients, the main symptom is pain that occurs after eating. This fact is explained by insufficient blood flow to the digestive organs during the period of their maximum activity, as well as the sensitivity of the digestive organs to ischemia. The nature of the pain is different: in the initial stage of the disease, the pain is equivalent to a feeling of heaviness in the epigastric region, then with the worsening of circulatory disorders, aching pain appears, the intensity of which gradually increases [8, 12]. The second common sign of chronic ischemia of the digestive organs is intestinal dysfunction, manifested in the form of a violation of the secretory and absorption functions of the small intestine (flatulence, unstable frequent loose stools) and the evacuation function of the large intestine with persistent constipation. Progressive weight loss is considered the third most common symptom of CIOP and is associated both with the refusal of patients to eat due to pain, and with a violation of the secretory and absorption functions of the small intestine, which is especially pronounced in the late stage of the disease [8, 13, 14].
A pathognomonic sign during an objective examination is a systolic murmur 2–4 cm below the xiphoid process in the midline, determined when the abdominal aorta and/or SN are predominantly affected. With severe stenosis or occlusion of the visceral arteries, systolic murmur may be absent, which is not a reason to exclude their damage [8, 13].
The localization of ischemic damage to the digestive organs depends on the visceral artery feeding them. Thus, when an emergency occurs, the organs of the upper floor of the abdominal cavity are predominantly affected: the liver, pancreas, stomach, duodenum (duodenum) and spleen. Stenosis or occlusion of the SMA is manifested by various dysfunctions of the small intestine, and damage to the IMA often causes ischemia of the large intestine [3, 14]. At the same time, the developed collateral network between the visceral arteries contributes to long-term functional compensation in conditions of impaired main blood flow, therefore, occlusive or stenotic lesions of the visceral branches of the abdominal aorta do not always lead to the appearance of CIOP symptoms. The most striking clinical picture of CIOP is described when two or all three visceral arteries are affected [3, 8, 12, 14].
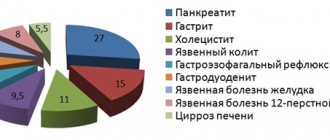
The frequency of ulcerative lesions of the stomach and duodenum when the patency of unpaired visceral arteries is impaired is noteworthy. Thus, Olbert F. et al. found them in 18% of patients with SN stenosis and in 50% of patients with SMA lesions [15]. Other authors found ulcerative lesions of the stomach and duodenum in more than 30% of cases of CIBOP of atherosclerotic origin, and suggested that peptic ulcer disease in elderly and senile patients is the most common manifestation of CIBOP [3, 9, 16].
According to a survey conducted at the Central Research Institute of Gastrointestinal Diseases, ischemic gastroduodenopathy was detected in 46.2% of cases and ranks first among the clinical forms of CIBOP [14]. With chronic disruption of the blood supply to the stomach and duodenum, progressive atrophy of the mucous membrane of these organs is observed, while the mucous membrane of the antrum of the stomach is affected more often than the body and fundus, which is associated with the characteristics of vascularization and sensitivity to hypoxia. Impaired blood supply to the mucous membrane of the stomach and duodenum leads to a decrease in the production of protective mucosubstances by epithelial cells, which contributes to ulcer formation [17]. Characteristic clinical features of erosive and ulcerative lesions of the gastroduodenal zone in chronic abdominal ischemia are manifestation of the disease in the form of bleeding, lack of seasonality of exacerbations, atypical clinical picture, high frequency of concomitant cardiovascular diseases, relapses, large size of the ulcer defect, low effectiveness of antiulcer therapy.
The incidence of ischemic pancreatopathy in CIBOP is 33.9% [17]. The main feature of the blood supply to the pancreas is the absence of its own large arteries. The pancreas is supplied with blood from the branches of the common hepatic, superior mesenteric and splenic arteries. It is these features that determine the incidence of pancreatic necrosis, as well as the frequency of ischemic pancreatopathies during abdominal ischemia. There are certain difficulties in the differential diagnosis of ischemic pancreatopathy with banal chronic pancreatitis, since the clinical manifestations of chronic ischemic pancreatitis are nonspecific. Both conditions are characterized by: intense pain after eating in the epigastric region, left hypochondrium, intractable (or poorly controlled) with antispasmodics, as well as sitophobia, pancreatic insufficiency, weight loss [17]. Ischemic pancreatopathy can occur as acute ischemic pancreatitis, including fatal, chronic ischemic pancreatitis. It should be noted that chronic pancreatitis itself can be the cause of abdominal ischemia. Pancreatic cysts, exerting compression on nearby vessels, can eventually cause abdominal ischemia.
Ischemic damage to the large intestine (ICH), which, according to our data, ranks third among other forms of CIBOP deserves special attention [17]. Thus, when examining individuals with clinical symptoms of ischemic lesions of the colon (IPTC) in the mucous membrane of the sigmoid colon (the most vulnerable to disruption of the blood supply to the colon, since it is located in the area of underdeveloped anastomoses), signs of impaired microcirculation and inflammation characteristic of ischemic lesions were almost always revealed . Microscopic signs of ischemia occurred even before the development of macroscopic changes.
Histological examination of the mucous membrane in these cases revealed superficial necrosis of the epithelium, a decrease in the number of goblet cells, focal lymphoid cell infiltrates, paresis and plethora. These changes were accompanied by emptying of blood vessels, the development of stasis, thrombosis of the microvasculature and plasmorrhagia. We considered the described morphological changes in the mucous membrane of the sigmoid colon, identified by biopsy, to be the earliest reliable signs of IPTC.
Based on the data obtained, we identified another form of IPTC - microscopic. By analogy with the known microscopic (lymphocytic and collagenous) colitis, we called this form “microscopic ischemic colitis” (MIC). This form of IPTC develops in elderly and senile patients suffering from diseases of the cardiovascular system. Characteristic symptoms of microscopic ischemic colitis are: abdominal pain with predominant localization in the left iliac region, appearing after eating; constipation; abdominal discomfort and flatulence. On examination, the sigmoid colon is painful, spasmodic, and the cecum is often dilated; A positive Obraztsov symptom is characteristic [18].
Depending on the severity of clinical manifestations and the degree of disturbance of visceral blood flow, the following functional classes of CIBOP are distinguished [13, 14]: • First functional class (I FC) – absence of signs of disturbance of blood flow at rest and the appearance of abdominal pain only after a stress test. Clinical symptoms are not expressed. • Second functional class (II FC) – the presence of signs of circulatory disorders at rest and their intensification after functional load. Severe clinical symptoms: pain and dyspeptic syndromes, weight loss, impaired pancreatic function, impaired secretory absorption function of the intestine. • Third functional class (III FC) – the presence of severe circulatory disorders, detected at rest and combined with constant pain, severe weight loss and dystrophic changes in the digestive organs.
Treatment of ischemic colitis at ON CLINIC in Ryazan
The treatment regimen that our gastroenterologist will prescribe is selected individually for each patient and depends primarily on how far the disease has progressed. If intestinal ischemia is reversible, then this regimen may be limited to diet and the use of antispasmodics and mild laxatives. In the case of a more pronounced form of the disease, it is impossible to do without the use of drugs necessary to normalize the water and electrolyte balance. Blood transfusion and parenteral nutrition may also be needed. Finally, in the case of gangrenous intestinal ischemia, urgent surgery will be required to remove the affected part of the intestine.
Our specialists successfully treat ischemic colitis. The clinic provides the opportunity to pay for treatment on credit, and also constantly operates various programs to reduce the cost of treatment. Discounts are available for a number of patient categories.
Treatment of ischemic colitis
Therapy for the disease is complex and carried out under the strict supervision of a gastroenterologist. Drug therapy is prescribed in the initial stages in the absence of associated complications. To relieve the pathological process and disturbing symptoms, the following groups of drugs are used:
- means that normalize blood flow;
- electrolyte solutions;
- antibiotics;
- probiotics and vitamin-mineral complexes.
To consolidate the results of conservative therapy and prevent the progression of the disease, a therapeutic diet is prescribed, the rules of which are simple and accessible to everyone:
- normalization of diet;
- cooking food using gentle methods: steamed, oven, boiled;
- compliance with the drinking regime, in which it is advisable to drink at least one and a half liters of regular drinking water without gas during the day.
If drug treatment does not lead to normalization of the condition, surgery is prescribed, which involves removing the area of the organ affected by necrosis. If necrotic processes have spread to most of the intestine, the affected tissue is removed, and a stoma is formed on the front wall of the abdomen through which feces will leave the body.