Other articles from the section “Diseases of the digestive system”:
Dysbacteriosis: concept, types, treatment tactics. Bifilakt BIOTA
Chronic intestinal dysbiosis, signs and symptoms. Bifilakt BIOTA
Chronic dysbiosis, what causes it, symptoms and causes. Biphylact biota
Diet during dysbacteriosis, products for adults and children. Bifilakt BIOTA
Increase in temperature during dysbacteriosis. Bifilakt BIOTA
Rash due to dysbacteriosis: causes and symptoms in children and adults. Bifilakt BIOTA
The main causes of the development of dysbacteriosis. Bifilakt BIOTA
List of drugs for dysbacteriosis. Bifilakt BIOTA
The occurrence of dysbiosis after antibiotics. Bifilakt BIOTA
Diet for dysbacteriosis. Bifilakt BIOTA
Which doctor treats intestinal dysbiosis: symptoms, causes of the disease. Bifilakt BIOTA
Fungal infection of the digestive system
Constipation and its treatment, causes, prevention. Bifilakt BIOTA
Remedies for constipation. Tablets, pribiotics, laxatives. Bifilakt BIOTA
Effective home remedies for constipation. Bifilakt BIOTA
What to eat during constipation. Bifilakt BIOTA
Constipation in the elderly, main causes, therapy. Bifilakt BIOTA
Constipation in an adult, causes and treatment. Bifilakt BIOTA
What to do if constipation occurs. Some effective tips. Bifilakt BIOTA
How to do an enema at home during constipation. Bifilakt BIOTA
Lactase deficiency. Bifilakt BIOTA
Bloating: treatment for bloating. Bifilakt BIOTA
Causes of bloating and constipation. Bifilakt BIOTA
Bifilakt BIOTA for liver treatment
Bifilakt BIOTA for the treatment of stomach
Irritable bowel syndrome. Bifilakt BIOTA
Colitis: symptoms and treatment. Bifilakt BIOTA
Enterocolitis: symptoms and treatment of enterocolitis. Bifilakt BIOTA
Bifilakt BIOTA for intestinal treatment
Intestinal dysbiosis is a violation of the quantitative and qualitative composition of the flora caused by pathological conditions or provoking factors. Normal microflora helps maintain immunity, the digestion process and normal absorption of nutrients. With dysbiosis, pathogenic microorganisms predominate in the flora, as a result of which the body's defenses are reduced, digestion worsens, gastrointestinal dysfunction occurs, the intestinal walls become inflamed, and they become covered with erosions. This process is accompanied by unpleasant symptoms, poor health, abdominal pain, abnormal bowel movements and bloating.
What is dysbiosis
Contrary to popular belief, dysbiosis is not an independent disease.
There is no such diagnosis in the International Classification of Diseases, Tenth Revision (ICD-10). It would be more correct to say that dysbiosis, or dysbiosis, is a condition accompanied by an imbalance of intestinal microflora, which occurs as a consequence of other diseases or as a result of treatment with antibiotics. The risk group primarily includes newborns and infants. The fact is that at birth their digestive tract is sterile, which means that there is no microflora as such in it yet. Bifidobacteria and lactobacilli enter the child's body along with mother's milk. However, if a woman was treated with antibiotics during pregnancy, breastfeeding may worsen the situation.
This group also includes patients who have suffered severe illnesses accompanied by exhaustion of the body, infection, hematopoietic disorders or malignant neoplasms. Those people who are subject to frequent stress and bad habits are also at risk.
Dysbacteriosis in newborns
Dysbacteriosis occurs quite often in newborns.
A newly born baby's intestines are sterile, and bacteria, both beneficial and harmful, enter there after birth (more precisely, the first bacteria enter the intestines during childbirth). During breastfeeding, beneficial bifidobacteria, which normally make up the main (up to 98%) part of the microflora, multiply quickly in the intestines of a newborn.
The cause of dysbacteriosis may be late breastfeeding. In this case, other bacteria manage to colonize the baby’s intestines, and it is no longer so easy for bifidobacteria to colonize their habitat.
Another reason is artificial feeding. When bottle-feeding, bacteria inevitably enter the baby's body from the surface of the formula bottle. It is quite difficult to achieve absolute sterility of the nipple. And infant formula does not create an environment as nutritious for bifidobacteria as breast milk.
The causes of dysbiosis can also be allergic reactions, improper introduction of complementary foods, lack of necessary food enzymes, and the use of antibacterial drugs.
How dangerous are pathogenic microflora?
The human intestine is inhabited not only by obligate bacteria, but also by opportunistic bacteria. If the former are considered a “useful” segment of the intestinal microflora, ensuring normal digestion and supporting immunity, then the situation with opportunistic microbes is more complicated. Under normal conditions, such bacteria do not manifest themselves in any way, but when the natural balance shifts, when their number begins to predominate, a complex of symptoms arises, which is called intestinal dysbiosis.
Representatives of obligate microflora include:
- bifidobacteria;
- lactobacilli;
- propionobacteria;
- Escherichia coli (non-invasive Escherichia).
Representatives of opportunistic flora:
- staphylococci;
- streptococci;
- bacteroides.
There are also pathogenic bacteria (for example, salmonella, yersinia, vibrio cholerae) that are absent in the intestines of a healthy person. However, they can get there by drinking contaminated water or poorly washed food.
A shift in the healthy balance of intestinal microflora and the activity of pathogenic bacteria can be fraught with a number of unpleasant consequences. For example, disruption of the normal biocenosis can contribute to the production of carcinogenic metabolites and the development of malignant neoplasms.
Chronic inflammatory processes accompanying dysbiosis can lead to the development of chronic colitis and enteritis. The danger of the spread of inflammatory processes to the joints cannot be ruled out. Another complication of dysbiosis is a decrease in immunity - a person becomes more susceptible to bacterial and viral diseases.
Other possible complications:
- Hormonal imbalance.
- Premature aging.
- Diseases of the cardiovascular system.
- Sensitization of the body (tendency to allergic reactions).
- Development of atherosclerosis.
- Disorders of the nervous system.
- General weakness and increased fatigue.
Methods for diagnosing dysbiosis
First of all, it is necessary to establish the cause of the disturbances caused. Only when the influence of the factor that caused dysbiosis is stopped, is it possible to restore normal intestinal microflora.
To identify the cause of dysbiosis, laboratory diagnostic methods are used.
Stool analysis for dysbacteriosis
Analysis of stool for dysbacteriosis refers to cultural studies. The microflora is inoculated. The concentration and ratio of beneficial, opportunistic and pathogenic microorganisms are assessed.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Reasons for the development of dysbiosis
There are a lot of factors that provoke the development of dysbiosis - from regular stress to unfavorable environmental conditions. The most common reasons:
- Use of antibiotics. Antibacterial drugs (especially broad-spectrum) destroy not only pathogenic, but also beneficial microflora.
- Hormonal therapy. This also includes diseases accompanied by changes in hormonal levels. For example, with excess testosterone in women, the balance of intestinal microflora is disrupted.
- Chemotherapy. This radical method of combating metastases produces many unwanted complications, including disruption of the healthy balance of microflora.
- Frequent use of enemas. With regular use of cleansing enemas, beneficial microflora is washed out of the intestines. The greater the volume and frequency of enemas, the more pronounced the manifestations of dysbiosis will be.
- Stress. The microbiota communicates with the brain through the vagus (vagus nerve). Bifidobacteria and lactobacilli themselves are capable of synthesizing acetylcholine, norepinephrine and serotonin. These neurotransmitters are responsible for the psycho-emotional state of a person. At the same time, a reverse relationship is also observed: regular stress suppresses the growth of these bacteria.
- Bad habits. Alcohol and nicotine have a detrimental effect on obligate microflora.
- Poor nutrition. This issue causes controversy among experts. Some are inclined to believe that the role of malnutrition in the development of dysbiosis is overestimated. Others insist that in the absence of a sufficient amount of fiber and lactic acid products in the diet, the healthy balance of microflora is disrupted. Moreover, the situation can be aggravated by a combination with regular consumption of food containing antibiotics, preservatives and other xenobiotics.
- Weakening of intestinal motility. This factor provokes the growth of pathogenic microflora.
- Injuries and inflammations. Any violation of tissue integrity and inflammatory processes weaken the immune system, which affects the biocenosis of the intestinal microflora.
Figure 1. Memo - the main signs and causes of dysbiosis. Source: MedPortal
Symptoms of dysbiosis
Symptoms of dysbiosis are not specific: they can appear in various diseases.
The main symptoms of dysbiosis are as follows:
Stool disorder
With dysbacteriosis, stool disorder (diarrhea) may alternate with constipation.
Flatulence
Violation of the intestinal microflora leads to increased gas formation, manifested by bloating, sudden rumbling in the abdomen and involuntary passage of gas.
More about the symptom
Belching
With the help of belching, the body tries to get rid of excess gases.
More about the symptom
Heartburn
Heartburn with bacteriosis is associated with frequent belching: along with air, the acidic contents of the stomach enter the esophagus.
More about the symptom
Smell from the mouth
With bacteriosis, bad breath is possible, since gases from the intestines, entering the oral cavity through the esophagus, disrupt the purity of breathing.
More about the symptom
Bad taste in the mouth
Together with belching, particles of stomach contents enter the oral cavity, affecting the taste buds.
Abdominal pain
Abdominal pain can be caused by a sharp contraction of muscles: with dysbiosis, the intestines work unstable, the smoothness of its work is disrupted. Dysbacteriosis is also characterized by nagging pain that occurs as a result of tension, including as a result of gas pressure. The pain may worsen with changes in position, exercise, or bowel movements.
Kinds
The division of dysbiosis into types is not entirely correct. This condition is classified according to severity according to the criteria proposed by Doctor of Biological Sciences I.B. Kuvaeva and Doctor of Medical Sciences K.S. Ladodo.
Stage 1: the titer of lactic acid flora is reduced by no more than 20% of the norm. The number of bacteroides, as well as lacto- and bifidobacteria, decreases. In some cases, there is an increase in various representatives of opportunistic flora. As a rule, there are no noticeable disturbances in the gastrointestinal tract, which is why this stage is also called latent.
Stage 2: the so-called start-up phase. The proliferation of opportunistic microflora is increasing, the number of Proteus and Candida fungi is growing. At the same time, there is a pronounced tendency towards a decrease in bifidobacteria and other obligate microflora. The degree of intestinal dysfunction is assessed as mild.
Stage 3: aggression phase. Against the background of a rapid decrease in the number of lactobacilli and bifidobacteria, the growth of pathogenic gas-forming microflora progresses. There is an accelerated proliferation of Proteus, Staphylococcus aureus, as well as fungi of the genus Candida. Clinical manifestations are more pronounced.
Stage 4: phase of associated dysbacteriosis. Bifidobacteria at this stage may be completely absent, which leads to severe digestive disorders and the inability to absorb food normally.
The titer of opportunistic microflora reaches a high level, so much so that this essentially turns it into pathogenic. However, this phase occurs only in exceptional clinical situations (for example, while taking antibiotics in combination with hormonal and/or radiation therapy).
As for the classification of dysbiosis according to the localization of the pathological process, it is incorrect, since the process affects any segment of the large and small intestine.
Dysbacteriosis of the small intestine
As mentioned above, dysbiosis affects all parts of the intestine, so this definition is not entirely correct. However, there is a so-called small intestinal contamination syndrome. According to the concept of A. N. Mayansky, this syndrome is caused by the influence of pathogenic microflora on the absorption of fatty acids in the small intestine, which leads to impaired lipid absorption. This process, in turn, promotes the growth of pathogenic microflora, forming a vicious circle.
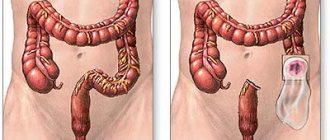
Dysbacteriosis of the large intestine
If in Soviet times some domestic doctors used such a definition, now, for the reasons described above, it is not considered correct. The most commonly used definition is “bacterial overgrowth syndrome.”
Dysbacteriosis
Intestinal dysbiosis (dysbiosis) is a disorder in the gastrointestinal tract of the relationships between microorganisms. This disorder causes changes in vital processes in the body: from digestion to immune changes, accompanied by manifestations of allergies or signs of chronic inflammation.
Recently, the term “intestinal dysbiosis” has been widely used, created from the Latin words “dis” - difficulty, disturbance, disorder, and “bios” - life.
Dysbiosis is a disruption of the functioning and mechanisms of interaction of the human body, its microflora and the environment. According to the Russian Academy of Medical Sciences, almost 90% of the Russian population experience various pathological changes in the microflora, indicating the presence of intestinal dysbiosis (dysbiosis).
The main causes of dysbiosis:
- uncontrolled use of antibiotics;
- malnutrition;
- disturbed ecology;
- state of chronic stress;
- existing functional or inflammatory diseases of the gastrointestinal tract;
- cancer therapy;
- immunity disorders.
The main manifestations of dysbiosis:
- diarrhea (or constipation);
- flatulence;
- bloating;
- stomach ache.
In most cases, patients experience intolerance to certain foods and experience general allergic reactions in the form of skin itching, urticaria, various skin rashes, and prolonged cough. Characteristic symptoms of intoxication (general malaise, lack of appetite, headaches). Patients with dysbiosis often get sick and often have recurrent upper respiratory tract infections.
The importance of normal flora for humans
Each person has an individual composition of normal flora, but the functions are always the same. The total number of microorganisms on the mucous membranes of an adult is 10 times greater than the number of his own cells.
This symbiosis of flora protects the mucous membranes from the invasion of pathogenic microbes, fungi, allergens and harmful substances through the walls of the mucous membranes into the human blood, thereby maintaining the constancy of its internal environment (homeostasis).
Normal flora forms bonds with secretory immunoglobulins (protective antibodies) and forms biofilms on the surface of mucous membranes.
Normoflora is involved in digestion and produces B vitamins and vitamin K.
The biomass of microorganisms populating the intestines of an adult healthy person is 2.5–3 kg (approximately 5% of its total weight) and includes up to 450–500 different types of microorganisms.
Age-related features of intestinal microflora
In a healthy child, from the moment of birth, the intestines are rapidly colonized by bacteria. Normal microflora should populate the newborn’s intestines on the 3rd–5th day of life. In children who are breastfed, by the 10th–21st day of life, a steady growth of lactobacteria, bifidobacteria, and lactic acid streptococcus is observed in the intestines.
Human milk contains a number of substances, so-called bifidus factors, which contribute to the colonization of the intestines by these types of microorganisms in adequate quantities.
The formation of normal microbial flora in a child may be disrupted if:
- use of antibacterial drugs during pregnancy and after childbirth;
- feeding with formula rather than breast milk;
- neurological disorders in the baby, in particular with perinatal damage to the child’s central nervous system.
Under the influence of all these factors, the timing of the formation of normal intestinal microflora, as well as its qualitative and quantitative composition, changes.
In a healthy child of the first year of life, 90–98% of the entire colon microbiocenosis should be bifid flora, which provides protection for the body from pathogenic microbes at this age.
In children older than one year, when their nutritional pattern approaches the usual diet of adults, the composition of the intestinal flora stabilizes, its quantitative indicators approach the norms of adults.
In elderly people, the composition of intestinal microbes also changes: the content of bifidobacteria and lactobacilli is reduced, the content of E. coli is increased, with a change in their enzymatic activity.
Laboratory diagnostic methods Laboratory methods can be direct (isolation of living microflora from a material) and indirect (determination of products associated with the vital activity of flora).
- Direct methods include stool cultures - Dysbacteriosis with determination of sensitivity to bacteriophages or Dysbacteriosis with determination of sensitivity to antibiotics and bacteriophages
- An indirect method is: biochemical analysis of feces - Biochemical study of the metabolic activity of intestinal microflora
When can dysbacteriosis be confirmed by laboratory analysis:
- Reduction or disappearance of bifidobacteria.
- Reducing the content of complete E. coli.
- Increased content of hemolytic Escherichia coli strains.
- Change in total E. coli count.
- Presence of opportunistic enterobacteria.
- Change in the number of enterococci.
Doctors assess the degree of imbalance of intestinal flora as follows:
First degree
Latent phase of dysbiosis: manifests itself only in a decrease by 1–2 orders of magnitude in the amount of protective microflora - bifidobacteria, lactobacilli, as well as full-fledged E. coli - up to 80% of the total amount. The remaining indicators correspond to the physiological norm (eubiosis). As a rule, the initial phase does not cause intestinal dysfunction and occurs as a reaction of the body of a practically healthy person to the influence of unfavorable factors, such as, for example, a violation of the diet and a change in the climatic zone (season of the year). In this phase, it is possible for a small number of individual representatives of the opportunistic flora to grow in the intestines. There are no clinical manifestations of dysbacteriosis in this phase.
Second degree
The starting phase of more serious disorders is characterized by a pronounced deficiency of bifidobacteria against the background of a normal or reduced number of lactobacilli or their reduced acid-forming activity, an imbalance in the quantity and quality of E. coli, among which the proportion of lactose-negative or citrate-assimilating variants is increasing. At the same time, against the background of a deficiency of protective components of the intestinal microbiocenosis, the proliferation of either plasma-coagulating staphylococci, or Proteus, or fungi of the genus Candida occurs. Vegetation in the intestines of Proteus or plasma-coagulating staphylococci in this phase of the development of dysbacteriosis is often transient rather than permanent. Functional digestive disorders are not clearly expressed - sporadically loose stools of a greenish color with an unpleasant odor, with a shift in pH to the alkaline side, sometimes, on the contrary, stool retention, sometimes nausea is noted.
Third degree
The phase of aggression of the aerobic flora is characterized by a clear increase in the content of aggressive microorganisms - at the same time, Staphylococcus aureus and Proteus, hemolytic enterococci multiply up to tens of millions in association, replacement of full-fledged Escherichia with bacteria of the genera Klebsiella, Enterobacter, etc. is observed. This phase of dysbiosis is manifested by intestinal dysfunctions with disorders of motility, secretion enzymes and absorption. Patients experience frequent, loose stools, often green in color, decreased appetite, deterioration in health, children become lethargic and moody.
Fourth degree
The phase of associative dysbiosis is characterized by a deep imbalance of the intestinal microbiocenosis with a change in the quantitative ratios of the main groups of microorganisms, a change in their biological properties, and the accumulation of toxic metabolites. Vegetation of enteropathogenic serotypes of E.coli, Salmonella, Shigella and other pathogens of acute intestinal infections is characteristic. Clostridia may multiply. This phase of dysbiosis is characterized by functional disorders of the digestive system and disturbances in general nutritional status, body weight deficiency, pale skin, decreased appetite, frequent stools mixed with mucus, greens, and sometimes blood, with a sharp putrid or sour odor.
According to I. B. Kuvaeva and K. S. Ladodo (1991)
If the study for dysbacteriosis does not reveal pathogens of dangerous intestinal infections, then to restore the normal balance of microflora, bacteriophages can be used, which are destructive to microbes, but safe for humans. The result form, which indicates the sensitivity of the identified pathogenic microorganism to bacteriophages, indicates the manufacturer of the drug and the batch.
Using these data, you can buy exactly the bacteriophage with which the testing was carried out.
Good health to you! Your KDL laboratory
Symptoms of intestinal dysbiosis
The severity of symptoms of intestinal dysbiosis largely depends on the stage of this condition.
Stage 1. Periodic alternation of diarrhea with stool retention, uneven coloring of stool, increased gas formation, decreased appetite.
Stage 2. Increased flatulence, constipation and diarrhea also become more pronounced. Belching, abdominal pain of undetermined localization, heartburn. Skin rashes may occur.
Stage 3. The listed dyspeptic disorders intensify, the frequency of episodes of diarrhea can reach 4-5 times a day. At this stage, non-healing skin ulcers appear.
Stage 4. The listed symptoms are accompanied by manifestations of intoxication: nausea, vomiting, increased body temperature and general weakness. Mucus may appear in the stool.
Figure 2. Memo - symptoms of dysbiosis. Source: MedPortal
When to see a doctor?
If digestive disorders do not go away within a few days, you should consult a gastroenterologist. Skin rashes or previously uncharacteristic allergic symptoms should cause particular concern. It is better not to delay a visit to the doctor, because the later the causes of this condition are identified, the more time it will take to eliminate it.
Treatment of intestinal dysbiosis
Since intestinal dysbiosis often accompanies the course of some diseases or is the result of previous diseases of other organs and systems of the body, the treatment of dysbiosis should be comprehensive and include methods for eliminating the underlying disease along with normalizing the intestinal microflora, otherwise the therapy will be ineffective.
Which doctor treats intestinal dysbiosis ? To treat dysbiosis, you may need to consult several specialists, depending on the pathology that caused or accompanied dysbiosis. But, mainly, a gastroenterologist deals with gastrointestinal disorders and dyspeptic manifestations.
Treatment of dysbiosis includes the following steps:
- correction of immunity;
- normalization of nutrition;
- elimination of pathogenic microorganisms;
- restoration of digestion;
- populating the headspace with beneficial bacteria;
- achieving a balance between beneficial and opportunistic bacteria.
The prescription of drugs should be carried out by a gastroenterologist after a preliminary examination and based on the test results, which will allow the microflora to be restored within several weeks.
Diagnosis of intestinal dysbiosis
The appearance of even 1-2 of the above symptoms should be a cause for concern and contact a gastroenterologist. It should be understood that diagnostics will be aimed not so much at identifying dysbiosis, but at searching for possible causes and complications of primary diseases that contributed to its development.
Typically, the doctor uses screening and differential diagnostics aimed at identifying diseases of the intestines and liver (nonspecific ulcerative colitis, irritable bowel syndrome, colon cancer, hepatitis of various origins).
Direct indications for studying the state of intestinal microflora are:
- Long-term course of intestinal disorders.
- Prolonged recovery period after infectious diseases or surgical interventions.
- Dyspeptic disorders due to the use of antibacterial drugs or regular contact with them (at work or among medical staff).
The following methods are used directly to diagnose dysbiosis:
- coprogram;
- bacteriological examination of biopsy or small intestinal juice;
- gas chromatography and mass spectrometry;
- breath test to determine hydrogen content.
During a coprological study, the number of bifidobacteria, lactobacilli, enterobacteria, E. coli, as well as representatives of opportunistic microflora (Staphylococcus aureus, Pseudomonas aeruginosa, Proteus, fungi of the genus Candida, etc.) is determined. However, the richness and variability of the composition of the intestinal microflora does not make it possible to obtain a complete picture of changes in the intestinal microbiocenosis. Therefore, from the point of view of modern medicine, stool analysis is considered an outdated method.
Usually preference is given to more modern diagnostic procedures—gas chromatography combined with mass spectrometry.
Causes of dysbiosis
The causes of dysbacteriosis can be:
- changes in acidity in the intestines. If the environment in which bacteria are found becomes overly acidic or overly alkaline, it can inhibit beneficial bacteria and promote the development of pathogenic microorganisms. Changes in acidity are usually a consequence of chronic diseases (cholecystitis, pancreatitis, gastritis, peptic ulcer, etc.);
- insufficient amount of enzymes necessary to ensure the digestive process. Undigested food remains create a favorable environment for the development of pathogenic microbes;
- disruption of the intestinal muscular system, resulting in food not moving through the intestines properly. Decreased tone or spasm of the intestinal muscles can be a consequence of surgery, stress, or caused by vegetative-vascular dystonia;
- intestinal parasites (worms), bacterial and viral infections;
- taking antibacterial drugs;
- poor nutrition (lack of dairy products and plant fiber in the menu, abuse of foods containing preservatives, etc.)
Treatment of intestinal dysbiosis in adults
Contrary to the stereotypes imposed by commercials, taking probiotics does not solve the problem at the root. It is necessary first of all to find and eliminate the cause of dysbiosis, since the phenomenon itself is secondary.
Treatment of intestinal dysbiosis should be based on the following principles:
- Elimination of external risk factors (correction of nutrition, drinking clean water, minimizing contact with harmful substances, and so on).
- Suppression of excessive growth of opportunistic microflora.
- Taking probiotics and prebiotics.
- Consolidating a positive result and achieving stable remission.
Let's take a closer look at all these principles.
Diet
Source: freepik.com/poringdown
Proper nutrition plays an important role in stabilizing the microbiocenosis of the intestinal microflora. Therefore, treatment should begin with diet correction. It is necessary to reduce the consumption of foods that cause fermentation processes (or even better, completely abandon them). This also applies to products that are not recommended for consumption for chronic gastrointestinal diseases. The reason for this is that, as we already know, dysbiosis is always secondary to the underlying disease, such as colitis, gastritis or hepatitis.
Improper nutrition provokes exacerbation of diseases of the liver and gastrointestinal tract, which will aggravate the imbalance of intestinal microflora. Therefore, without correcting the diet, all attempts to combat dysbiosis are doomed to failure.
| Unwanted Products | Recommended Products |
| Baking, confectionery Alcohol (especially beer and sweet wine) Beans and grapes Kvass Spicy seasonings Cheeses with fat content above 40% | Fermented milk products (kefir, yogurt, fermented baked milk) Sauerkraut Berries and fruits that reduce fermentation (apricots, black currants, cranberries) Porridge (except pearl barley) Soups with fresh broth Lean meat and fish Vegetables (carrots, pumpkin, zucchini, potatoes) |
Much attention should be paid to fiber - dietary fiber stimulates intestinal motility and absorbs toxins. In fact, fiber is a prebiotic, since the obligate intestinal microflora uses dietary fiber as a nutrient medium.
Medications
Before moving on to the description of medications used for dysbiosis, we emphasize that first of all it is necessary to treat the underlying disease. This is called etiological treatment - influencing the cause, not the effect, of the disease. As for drugs used directly to eliminate dysbiosis, they can be divided into several groups.
Antibiotics
The use of antibacterial drugs is advisable in case of excessive growth of pathogenic microflora in the intestine, which is accompanied by a deterioration in the functional state (impaired motility and absorption). The following groups of antibiotics are used:
- penicillins (amoxicillin);
- fluoroquinolones (ofloxacin, norfloxacin);
- tetracyclines (doxycycline);
- broad spectrum (rifaximin).
The average course of treatment is 7 days.
Probiotics
Expert opinions regarding the effectiveness of these drugs are contradictory. Many domestic gastroenterologists consider the administration of probiotics to be an integral part of the fight against dysbiosis, however, in foreign clinical practice, the advisability of using these drugs is now increasingly criticized. Opponents of the use of probiotics argue their position by the fact that most of it simply does not take root in the patient’s body. There are also opinions that the use of these drugs may contribute to the growth of fungal infections in the blood.
The basis of the composition of probiotics is represented by lacto- and bifidobacteria, but Escherichia, streptococci and enterococci can be used as a supplement. Probiotic release form:
- capsules;
- powders;
- drops;
- rectal suppositories (suppositories).
Drugs to improve digestion
This includes pancreatic enzymes (pancreatin and drugs containing it), as well as drugs to improve intestinal motility (domperidone, metoclopramide). In addition, to normalize the intestinal absorption function and improve the functional state of the liver, hepatoprotectors (phospholipids, preparations with milk thistle extract) are prescribed.
Folk remedies
Here it is important to determine the interpretation of this definition in the context of eliminating dysbiosis. For example, some consider the consumption of fermented milk products or sauerkraut as a folk method of treating dysbiosis, although in fact this is only one aspect of normalizing the diet.
As for decoctions of medicinal herbs or yeast infusions, which are used both for oral consumption and for microenemas, it is better not to use such methods without the consent of a doctor. Often such remedies do more harm than good.
Reasons for development
Dysbacteriosis is not a “classical” independent disease and does not occur on its own. Rather, it is a pathological condition that is activated under the influence of various unfavorable factors or diseases:
- The use of medications (usually antibiotics) and antiseptic rinsing solutions in the treatment of various diseases can lead to the emergence and development of pathogenic intestinal microflora. “Friendly” bacteria under the influence of these drugs die along with pathogenic microorganisms. Their concentration does not have time to be restored in the required quantity to participate in the metabolic processes of the body, including in the fight against various pathogens.
- A history of chronic diseases of the gastrointestinal tract (for example, gastritis, pancreatitis), causing functional disorders of the intestines and malfunctions of the digestive system.
- Infectious intestinal diseases caused by staphylococcus, enterovirus infection, salmonella, etc.
- Parasitosis.
- As a complication after surgical interventions on the abdominal organs.
- Wrong lifestyle: bad habits (alcohol abuse, smoking), poor diet, stressful situations that lead to a general weakening of the body.
- Immune system disorders, especially if there is a history of diseases associated with immunodeficiency. After treatment of oncological diseases with radiation therapy and various chemotherapy or hormonal therapy regimens.
Treatment prognosis
Microflora has a remarkable property: it recovers on its own even after taking antibiotics. Therefore, the most important thing is to create favorable conditions for its restoration (we talked about them in the previous sections of the article). Thus, the prognosis for dysbacteriosis is positive. At the same time, it is important to understand that under unfavorable circumstances (exacerbation of chronic diseases, poor lifestyle, violation of healthy eating rules, etc.), the re-development of dysbiosis cannot be ruled out.
Intestinal dysbiosis in children
The cause of the development of dysbacteriosis in children is poor nutrition and artificial feeding. It is also necessary to be careful when treating with antibiotics, since it is this therapy that causes a number of symptoms of dysbiosis. Signs of the disease are similar to the manifestation of the disease in adults. A pediatrician deals with the treatment of intestinal microflora disorders in children; in severe conditions, the help of a gastroenterologist and an infectious disease specialist is required (“BIOTA for the treatment of dysbiosis in children”).
Prevention of intestinal dysbiosis
To avoid excess microbial growth in the intestines, just follow a few simple recommendations.
- Observe hygiene rules when preparing and eating food. You should also avoid drinking poorly purified water.
- Maintain physical activity. A sedentary lifestyle has a bad effect on intestinal motility, and this, in turn, leads to constipation and the associated processes of fermentation and growth of pathogenic microflora. Any type of exercise is suitable - from walking to working out in the gym. The load should be selected in accordance with the age and functional capabilities of the body. The most important thing is to avoid physical inactivity.
- Watch your diet. It is important that the menu contains fiber and a sufficient amount of clean drinking water (you should drink based on your own thirst, but usually at least one and a half liters per day is recommended).
- Avoid bad habits and stress.
- Do not self-medicate with antibiotics. The prescription of antibacterial drugs should always be justified, and therefore is the prerogative of the attending physician.
Symptoms
Symptoms of dysbiosis are formed under the influence of disruption of normal intestinal function and are characteristic of most gastrointestinal diseases:
- Discomfort in the abdominal area, often turning into pain. They are usually uneven, spastic in nature, and their intensity may increase during meals.
- Dyspeptic disorders (constipation, diarrhea). Due to the fact that dysbacteriosis disrupts the normal process of digestion and assimilation of food.
- Bloating, feeling of heaviness in the epigastric region, flatulence. The causes of these unpleasant sensations are congestion caused by problems with intestinal motility. Intestinal masses that are not removed from the abdominal cavity are subject to processes of rotting and fermentation. The consequence of these processes is increased formation of gases.
- Nausea, loss of appetite, low-grade fever.
- General signs of intoxication (lethargy, drowsiness, low mood) and metabolic disorders (hair loss, skin rashes, irritability, etc.) with a long course of the disease. These symptoms are associated, first of all, with the body’s inability to absorb useful substances and elements in the required volume.
- The appearance of atypical allergic reactions: consuming neutral foods that were previously well digested can cause allergy attacks.
Important! It is necessary to take seriously the treatment of the underlying disease, identifying and eliminating the cause that caused dysbiosis. Entrust this issue to professionals. Only a little “help” is needed from you: be careful about taking medications that can cause inhibition of beneficial microorganisms (they must be taken against the background of correctors of the intestinal environment), lead a healthy lifestyle and maintain a proper diet. If symptoms appear that indicate the development of an imbalance of microflora, seek medical help: the general practitioner or specialist whom you are seeing for the “main” disease will adjust the treatment regimen or prescribe you adequate complex therapy. Be healthy.