Dyspepsia
(
dyspepsia
; Greek dys- + pepsis digestion) is a disease of the gastrointestinal tract of functional origin in children. Dyspepsia occurs as a result of a discrepancy between the demands placed on the body in the form of volume or composition of food and the ability to digest this food with the normal amount of appropriate enzymes of the digestive tract. There is ch. arr. in children up to 8-9 months.
The term "dyspepsia" was introduced at the end of the 19th century. Viennese pediatrician H. Widerhofer to designate a disease of young children with clinical manifestations in the form of vomiting and diarrhea, not accompanied by pathomorphological changes. Thus, the purely functional nature of Dyspepsia was emphasized. In the clinic of internal diseases of adults, the term “dyspepsia” is not used; this concept is identical to various gastrointestinal tracts. disorders that occur in a number of diseases. In pediatrics, it is used to designate individual clinical forms.
The main forms of Dyspepsia are: 1) simple; 2) toxic; 3) parenteral.
In the first days of a newborn’s life, physiological, or transitional, dyspepsia is often observed.
Its occurrence is based on the process of adaptation of the child’s body to new nutritional conditions and the still unestablished secretory-motor function of the gastrointestinal tract. tract. The increased sensitivity of some children to the fat of human milk, as well as lactose intolerance, due to a decrease in the activity of lactase in the child’s intestinal mucosa, is important. The role of physiological changes in the bacterial flora of the newborn’s intestine cannot be excluded: at birth, the sterile intestine is populated by various bacteria from the environment. With the transition to breastfeeding, this flora is replaced by Bact. bifidus. When bacteria die, a certain amount of toxins are released that contribute to the development of phenomena D. Klin, manifestations of physiol. D. scanty - frequent, liquid greenish squirting stools, bloating, some restlessness, mild diaper rash on the buttocks. No special treatment is required; when lactation is established (see), these symptoms disappear.
Causes
Symptoms of dyspepsia can occur in anyone and at any age. If the disease is not treated, a chronic form may develop. There are several main reasons that provoke the development of functional dyspepsia:
- psycho-emotional stress (pathology of neurotic origin develops);
- taking certain groups of medications (antibiotics, antitumor drugs, hormonal drugs);
- errors in nutrition, consumption of large amounts of nutrients (carbohydrates, proteins and fats). This is the main reason for the development of putrefactive, fatty and fermentative dyspepsia;
- intoxication of the body due to household poisoning, viral infections and purulent diseases;
- increased secretion of hydrochloric acid;
- motility disorders of the gastrointestinal tract.
The main causes of functional dyspepsia include psychological trauma and stress.
general description
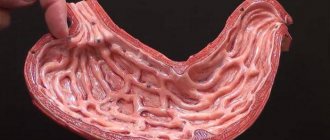
Dyspepsia is a digestive disorder caused by functional or organic causes.
Signs of dyspepsia are pain of unclear localization in the upper third of the abdomen, heartburn, nausea, a feeling of fullness in the stomach, and abnormal bowel movements. The diagnosis is made on the basis of endoscopy of the upper gastrointestinal tract, after differential diagnosis from other diseases of the digestive tract.
Treatment of dyspepsia is symptomatic and includes taking medications to improve the functioning of the gastrointestinal tract, enzyme preparations, and so on. Psychotherapeutic measures are of great importance. Almost all patients note a decrease in the severity of dyspepsia symptoms after undergoing a course of treatment with a psychologist.
Types of dyspepsia
Nutritional or functional dyspepsia is of the following types:
- Putrid dyspepsia. Occurs with excessive consumption of protein products, especially those that require a long time to digest. Toxic substances formed during the breakdown of proteins cause intoxication of the patient's body. This mainly applies to red meats (lamb, pork, beef) and their derivatives (sausages and other meat products), the abuse of which stimulates the development of putrefactive intestinal microflora.
- Fatty (soapy) dyspepsia. Caused by eating too much refractory fats, such as lamb and lard and their derivatives.
- Fermentative dyspepsia. It is caused by the predominance in the diet of foods high in carbohydrates that cause fermentation (sweet and flour products, honey, fruits, peas, cabbage, legumes, etc.), as well as fermentation products (kvass, mash, pickled vegetables, etc.). At the same time, fermentative microflora develops in the intestines.
Dyspepsia, which is a consequence of enzyme deficiency, is of the following types:
- Pancreatogenic (lack of pancreatic enzymes);
- Gastrogenic (caused by disruption of the secretory function of the stomach);
- Enterogenous (disturbed secretion of intestinal juice);
- Hepatogenic (liver origin);
- Cholecystogenic (caused by impaired bile secretion);
- Mixed dyspepsia.
Causes of dyspepsia
Most often, dyspepsia is caused by a lack of digestive enzymes, as well as poor nutrition.
The development of this pathological condition of the body can also be caused by:
- frequent stress;
- neurological diseases;
- binge eating;
- improper eating.
In addition, dyspepsia may develop after the following organic diseases:
- gastritis;
- diseases of endocrine organs;
- stomach or duodenal ulcer;
- uncontrolled use of medications;
- stomach tumors;
- pancreatic pathology;
- gallbladder diseases.
In children, the cause of the disease is usually a discrepancy between the composition and quantity of food consumed and the capabilities of their digestive system. In other words, careless introduction of new foods into the baby’s diet and overfeeding lead to the development of the disease.
The development of dyspepsia syndrome in young children is facilitated by the immaturity of the digestive tract. In older children, dyspepsia most often occurs against the background of hormonal imbalance during puberty.
Symptoms of different types of dyspepsia
Symptoms of dyspepsia can manifest themselves in different ways, since they directly depend on the specific type of pathology. However, all types and subtypes of dyspepsia are characterized by a number of similar symptoms:
- Unpleasant sensations in the epigastric region (upper abdomen): a feeling of heaviness, fullness, sometimes pain of varying intensity;
- Nausea;
- Belching. Single belchings may not be a sign of a disorder, but constant ones indicate dyspepsia;
- Heartburn. A burning sensation in the epigastric and retrosternal region that occurs when aggressive gastric contents enter the esophagus, which should not normally occur;
- Flatulence. A feeling of fullness in the abdomen caused by increased gas formation in the intestines, as well as increased gas production;
- Stool disorder. A characteristic symptom of dyspepsia is irregular bowel movements, usually frequent.
Symptoms of fermentative dyspepsia:
- bloating in the lower abdomen, and excessive gas;
- frequent bowel movements (loose, foamy stools, light in color and sour odor).
Symptoms of organic (enzymatic) dyspepsia:
- rumbling and transfusion in the abdomen;
- frequent passing of gas;
- nausea without vomiting;
- unpleasant taste in the mouth;
- frequent bowel movements (loose stools);
- the presence of food residues in the stool;
- fatigue and weakness;
- headaches and poor sleep.
Symptoms of putrefactive dyspepsia:
- signs of intoxication;
- nausea and vomiting (see also - how to get rid of nausea);
- headaches, dizziness;
- weakness and malaise;
- frequent loose stools (stools are dark and have a strong odor).
Symptoms of fatty dyspepsia:
- noticeable pain 30 minutes after eating;
- feeling of heaviness in the stomach and fullness;
- belching and flatulence;
- copious stools (stools are whitish and greasy).
1.What is dyspepsia and its symptoms?
Dyspepsia
is a general condition, and this word usually describes a group of symptoms, rather than one pronounced symptom of a disease of the gastrointestinal tract.
Symptoms of dyspepsia may include:
- abdominal pain or discomfort;
- Bloating;
- Discomfort and feeling of fullness in the stomach after eating;
- Nausea;
- Loss of appetite;
- Heartburn;
- Belching food or liquid.
Most people experience some of the symptoms of dyspepsia occasionally throughout their lives, and this is often not a cause for serious concern.
A must read! Help with treatment and hospitalization!
Diagnosis of dyspepsia
In order to identify a patient with dyspepsia of one type or another, comprehensive measures are taken. You will need to consult doctors such as a gastroenterologist, an infectious disease specialist and a therapist. Depending on the symptoms of the disease, the following procedures may be prescribed:
- Ultrasound examination makes it possible to identify chronic pancreatitis and gallstone disease.
- Esophagogastroduodenoscopy - allows you to detect reflux esophagitis, gastric ulcers, stomach tumors and other organic diseases.
- X-ray examination.
- Electrogastroenterography - allows you to identify gastroduodenal motility disorders.
- Clinical blood test.
- Blood chemistry.
- General stool analysis, stool occult blood test.
- Stomach scintigraphy helps detect gastroparesis.
- Antroduodenal manometry - allows you to examine the motility of the stomach and duodenum.
- Esophagomanometry - which allows you to evaluate the contractile activity of the esophagus, the coordination of its peristalsis with the work of the lower and upper esophageal sphincters (LES and UES)
- Daily pH-metry allows you to exclude gastroesophageal reflux disease.
- Determination of infection of the gastric mucosa by the bacterium Helicobacter pylori.
Prevention of dyspepsia
The main measures to prevent the disease are:
- proper nutrition;
- treatment of pathological conditions that can lead to the development of dyspepsia;
- avoidance of stress and other psycho-emotional disorders;
- regular sanitation of foci of chronic infection in the body;
- cessation of alcohol abuse and smoking;
- giving up a sedentary lifestyle - daily walks in the fresh air, physical education;
- weight control, preventing the development of obesity;
- refusal of uncontrolled use of medications;
- strengthening immune defense;
- avoiding constant increased stress on the abdominal muscles;
- Regularly undergoing preventive examinations - this will help to identify pathological changes in the body at an early stage, which will allow for effective corrective therapy and prevent the development of complications.
Good health to you!
Treatment of dyspepsia
Treatment of patients with dyspepsia should be comprehensive and include not only the prescription of medications, but also measures to normalize lifestyle, diet and diet.
Functional dyspepsia
Treatment of functional dyspepsia is general. The patient is advised to exclude salty, spicy and fatty foods from the diet. Eat small portions, but often (from 6 times a day). If necessary, you can additionally assign:
- Antacids (Gaviscon, Almagel);
- H+-pump inhibitors (Omeprazole, Rabeprazole, Lansoprazole);
- Sedatives (Phenazepam, Adaptol, Grandaxin).
Fermentative dyspepsia
- For fermentative dyspepsia, treatment should begin with a diet low in carbohydrate foods. It is allowed to eat high-protein dishes (boiled meat, meat broth, butter, steamed chicken), it is necessary to reduce the amount of bread, potatoes, vegetables and fruits, baked goods, and cereals.
- Adsorbent substances (Smecta, Polysorb, Neosmectin), probiotics (Acipol, Laktofiltrum, Bifiform, Bifikol) and enzyme preparations for dyspepsia (Creon, Pancreatin) are used. As you recover, carbohydrate-containing foods are gradually introduced into the diet, but in limited quantities. The menu and allowed dishes are determined depending on the cause of the development of this syndrome.
Putrid dyspepsia
- Therapy is carried out similarly to the fermentation form. First of all, the patient is recommended to eat a diet that excludes protein (all types of meat and fish, dairy products, eggs, etc.). You should also use sorbents and probiotics. As a rule, enzyme preparations are not used during the treatment process. The need for antibiotic therapy is determined by the doctor.
Intestinal dyspepsia. First of all, it is necessary to treat the underlying disease:
- Intestinal infections - antibiotics;
- Food toxins – elimination of general intoxication and use of local local detoxicants (Enterodes, Polysorb MP);
- Crohn's disease - prescription of hormonal therapy.
If you have any of these conditions, you should not eat foods high in fiber. It is important to take sorbents (Smecta, Smectin, activated carbon, etc.), which are quite effective in eliminating the syndrome. To reduce pain, it is possible to prescribe antispasmodics (Drotaverine, Kellin, etc.).
Gastric dyspepsia
To eliminate this syndrome, the underlying disease should be treated. Depending on this, medical tactics will change. If the cause of dyspepsia is gastritis or peptic ulcer, the following therapeutic measures are recommended:
- If the role of Helicobacter is proven, the doctor prescribes complex antimicrobial therapy, which necessarily includes 2 antibiotics;
- A diet excluding fatty, salty and spicy foods. You should also not eat foods enriched with fiber (rye bread, fruits, vegetables, juices, etc.), as they can increase pain;
- It is possible to prescribe medications that create a protective membrane for the gastric mucosa (De-Nol, Sucralfate, etc.).
- Acidity should be normalized to treat dyspepsia. Increased secretion of hydrochloric acid can be eliminated with “H+-pump inhibitors” (Omeprazole, Rabeprazole, Lansoprazole) and antacids (Gaviscon, Almagel). With low acidity, you can stimulate acid-forming cells with Pentaglucide or plantain juice;
The discovery of an open ulcer or tumor is often an indication for surgery. If a patient has a hormonal disease, treatment can only be determined by an endocrinologist.
Toxic dyspepsia
Toxic dyspepsia occurs as a result of the same reasons as simple dyspepsia, but differs significantly from it in the presence of toxic syndrome (see). It can develop as a result of a gross nutritional error or be a further stage in the development of simple D. under the influence of unfavorable endogenous and exogenous factors. The transition of simple D. to toxic can occur from untimely and insufficient measures in relation to simple D. - too short a hungry pause, insufficient fluid supply, etc. Toxic D. often develops in children with reduced or altered reactivity: in premature infants, children suffering from dystrophy, patients with rickets, exudative diathesis, in children during the period of convalescence after any illness. Exogenous factors include: gross errors in diet, rapid transition to regular food, irrational feeding, especially artificial feeding; unfavorable environmental conditions - hot season, gross deficiencies in care, etc.
Pathogenesis
The main links in the pathogenesis of toxic D. are toxemia (see), exicosis, acidosis (see). The development of toxemia is preceded by deeper disturbances than with simple D., disturbances of the enzymatic function of digestion (see), gastric and intestinal motility, as well as the detoxification function of the liver. Changes in digestive conditions favor the increased proliferation of microbes in the intestines and their participation in the decomposition of food debris. The resulting toxic products, including waste products of microbes, enter the blood. They initially cause short-term irritation of the cerebral cortex; The first phase of toxicosis develops (irritative), accompanied by a short-term mobilization of some protective reactions of the body: increased acidity of gastric juice, increased motility and separation of intestinal juice, vomiting, frequent loose stools. The second phase of toxicosis (suporous-adynamic) is characterized by a deep inhibition of all regulatory functions of the body, a decrease in the excitability of the cerebral cortex, up to diffuse cortical inhibition. Due to the increased frequency of vomiting and the appearance of watery stools, dehydration of the body occurs (see), which in this phase of toxicosis reaches a pronounced degree - the isotonic type of dehydration is replaced by water-deficient and salt-deficient. Exicosis develops. The acid-base balance shifts towards acidosis, water-electrolyte metabolism is disrupted, and hypokalemia develops (see). Increasing intoxication contributes to the distortion of the function of internal organs, an increase in acidosis and causes severe metabolic disorders. Violation of the vital functions of the body sharply reduces immunity and favors the development of septic complications.
With toxic D., the whole organism is involved in the process: the activity of the c is disrupted. n. pp., cardiovascular, respiratory, excretory, endocrine systems; Not only water-salt metabolism is disrupted, but also other types of metabolism (see Metabolism and energy in children), and vitamin deficiency occurs (see Vitamin deficiency). Due to the activation of the body’s own microflora, various complications develop; Thus, despite the absence of inflammatory changes in the intestine, bacteria play a large role in the pathogenesis of toxic D.
Pathological anatomy
The nature of morphol changes in those who died from toxic D. mainly corresponds to the idea of toxicosis. An external examination reveals a greater or lesser degree of exhaustion, a significant loss of skin turgor, and sometimes hemorrhages in it. The abdomen, as a rule, is swollen due to flatulence of the small intestines and stomach, and therefore a high position of the diaphragm is often noted. In the mucous membrane of the stomach and intestines there are vascular disorders in the form of stasis and plethora. Due to pronounced intoxication, mucous degeneration of the columnar epithelium of the small intestine is often observed with the death of a number of cells, as well as massive desquamation of the epithelium into the intestinal lumen (this can be considered reliable only with an early autopsy of the deceased). On the part of the internal organs - vascular and dystrophic changes. Fatty infiltration of the liver and the epithelium of the convoluted tubules of the kidney is observed. Changes noted in the lungs (focal atelectasis, distelectasis, edema, plethora; lymphohistiocytic infiltration, sometimes with the presence of segmented leukocytes) indicate a violation of the immunological state of the child’s body and can be the cause of death.
Clinical picture
The clinical picture of toxic D. depends on the phase of toxicosis and the degree of dehydration. In the first phase, there is general motor and mental restlessness, shallow and rapid breathing. There is vomiting, diarrhea, and bloating. The temperature remains normal, the mucous membranes become less moist. The second phase of toxicosis is characterized by lethargy, adynamia, pronounced symptoms of dehydration: weight loss, dry skin and mucous membranes, a sharp decrease in tissue turgor; facial features are pointed, the large fontanel is somewhat sunken, breathing is deep, without. pauses (breathing of a “hunted animal”); Heart sounds are muffled, the boundaries of the heart are changed. There may be an increase in temperature to 38-39°. Oliguria is observed, in the urine there is protein, leukocytes, and casts. The amount of hemoglobin, leukocytes and erythrocytes in the blood is increased, ROE is low. Biochemical blood parameters are similar to those observed in toxic syndrome with dehydration of the body (see Toxic syndrome). With toxic D. of nutritional origin, such severe manifestations of toxicosis are rarely observed. Typically, toxicosis begins to quickly decrease under the influence of therapeutic measures, which once again confirms the functional nature of toxic D.
Treatment
Treatment in a hospital setting is aimed simultaneously against all three main links of the pathogenetic chain, as well as at restoring the secretory and motor activity of the gastrointestinal tract. tract. If there are indications, measures should be taken to improve cardiac activity by administering cardiac glycosides (strophanthin or corglycone) in a 20% glucose solution; At the same time, cocarboxylase and 5% sodium ascorbate solution can be administered. It is also advisable to inhale humidified oxygen. To combat intoxication, neocompensan, hemodez, polyglucin are used, as well as 5% glucose solution, Ringer's solution, isotonic sodium chloride solution, which are administered intravenously, drip-wise at the rate of 120-180 ml of liquid per 1 kg of child's weight. day. According to indications, plasma and its substitutes (albumin, protein) are prescribed. To eliminate acidosis, intravenous drip infusions of 4 and 5% sodium bicarbonate solutions are used (3-5 ml per 1 kg of weight). You can administer sodium bicarbonate in drip enemas in the form of a 4% solution. Detoxification therapy must be carried out under the supervision of a study of acid-base and water-electrolyte balance. At the same time, the child is given fluids in fractional doses, as with simple D. Considering that toxic D. is difficult to differentiate from an intestinal infection, it is recommended to carry out antibacterial therapy, mainly with broad-spectrum antibiotics. It is advisable to combine antibiotics administered enterally and parenterally, as well as antibiotics and nitrofuran drugs (eg, furazolidone).
Much attention should be paid to the nutrition and care of a sick child. The water-tea diet for toxic D. is longer - 18-24 hours. After this time, feeding begins according to the principle of maximum sparing, i.e., nutrition must correspond to the enzymatic capabilities of the gastrointestinal tract. tract and at the same time must be complete in terms of the content of food ingredients. In the first days of treatment, all these requirements are most fully met by human milk (see Breast milk), which can be recommended after a water-tea diet for all children, regardless of the nature of feeding. The amount of milk on the first day should be 100-200 ml, 10-20 ml should be given every 2 hours. Subsequently, the volume of food increases by 100-200 ml daily. From the 3rd day, the child is put to the breast for 1-2 feedings, and then the diet is expanded depending on age due to the introduction of fermented milk products (see Lactic acid products in children's nutrition) diluted with rice water 2:1, from 4-5 On the day porridge and other types of food previously received by the child are prescribed. It is necessary to expand the diet gradually, but systematically, which helps to increase reactivity and prevent complications.
At later stages, agents are used that help normalize the intestinal microflora and improve enzymatic activity (bifidumbacterin, colibacterin, enzyme preparations). Vitamins are prescribed: ascorbic acid, rosehip preparations, vitamin A in the form of carotoline, etc. The use of stimulants is justified - gamma globulin, prodigiosan, metacil, pentoxyl, etc.
Forecast
with timely treatment, it is favorable in most cases.
Folk remedies
In folk medicine, there are many recipes that are used for stomach dyspepsia. But before starting such treatment, you need to visit a doctor.
The most effective recipes:
- Fennel. To prepare the medicine, you need to take 10 g of fennel berries, pour 200 ml of boiling water and heat until boiling (over low heat for about 15 minutes). Then cool the broth, strain and add boiled water to it so that the result is the original volume. The entire amount of the medicine should be drunk throughout the day in small portions.
- Cumin/marjoram. Prepare a healing drink: place crushed cumin and marjoram seeds in 200 ml of boiling water and leave for 15 minutes. This remedy should be taken twice a day at a dose of 100 ml per dose.
- Grind the roots of elecampane. Take 1 teaspoon of raw material and pour 200 ml of cold boiled water. Do not heat or boil! The medicine is infused for 8 hours, then filtered and taken 1/3 cup three times a day before meals. Duration of treatment – 2 weeks.
- Prepare 375 g aloe, 625 g honey and 675 ml red wine. Wash and finely chop the aloe leaves, mix with the rest of the ingredients. You need to take the medicine 1 teaspoon before meals - this is the dosage for the first 5 doses. In the future, it is recommended to take 2 teaspoons twice a day before meals. The duration of treatment with this medicine is a minimum of 2 weeks, the maximum period of use is 2 months.
You cannot decide on the treatment of gastric dyspepsia using traditional methods on your own. Only after consulting a doctor can you be sure that it is safe to use homemade decoctions/infusions.