Symptoms
Colorectal cancer can remain asymptomatic for many years, so it is often diagnosed at a late stage.
A timely visit to a specialist will help prevent the progression of the disease and limit yourself to gentle treatment methods. The main sign of cancer development is often occult bleeding accompanied by progressive anemia, or obvious bleeding from the lower GI tract and changes in bowel movements.
Other early symptoms of bowel cancer include:
- rectal bleeding;
- blood in stool
- anemia;
- persistent diarrhea or diarrhea and alternating constipation;
- change in the shape and consistency of stool;
- abdominal pain;
- constant urge to defecate.
- weight loss;
- weakness, fatigue;
- lack of appetite.
If symptoms in the form of blood in the stool and constant discomfort in the intestines do not go away within several weeks, it is recommended to immediately seek advice from a physician or gastroenterologist. If a malignant pathology is suspected, the patient will be referred to an oncologist.
Causes of the disease
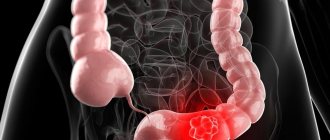
Colon cancer most often begins with benign polyps (adenomas). Oncology can develop both inside the intestine and spread beyond it, affecting surrounding tissues.
Risk factors for developing colorectal cancer:
- Age—the risk of developing the disease increases with age. Before age 40, a diagnosis of colorectal cancer is very rare. The risk increases after age 50, with peak incidence occurring in the eighth decade of life.
- Obesity (in people with a body mass index (BMI) greater than 30, the risk of developing the disease increases by 50-100 percent compared with people of the same weight, that is, a BMI below 24.99);
- Unhealthy diet high in animal fats, red meat and processed foods and low in vegetables, fruits and dietary fibre;
- Low physical activity;
- Smoking (it is estimated that up to 20% of colorectal cancer cases are related to smoking);
- Previous radiation therapy to the abdomen;
- Taking immunosuppressants after organ transplantation;
- Alcohol abuse;
- Previous gallbladder removal;
- HPV (human papillomavirus) infections;
- A history of cervical, vulvar, or vaginal cancer.
A tendency to intestinal cancer can be inherited. Yes, genes, along with a poor lifestyle, are the most common cause of colon cancer. It is estimated that 15-30% of colorectal cancer cases are genetic.
However, genetic factors are not just the fact that someone in the family previously suffered from colorectal cancer and could pass on the defective gene to their descendants.
Genetic factors also include:
- familial adenomatous polyposis syndrome, which is considered a so-called precancerous condition (colorectal cancer develops in 75-95% of patients with familial adenomatous polyposis);
- Lynch syndrome (formerly called hereditary nonpolyposis colorectal cancer). This is the most common cause of genetically determined colorectal cancer, accounting for 1-3% of cases;
- inflammatory bowel diseases (for example, ulcerative colitis increases the risk of colon cancer by 20 times).
IMPORTANT:
Patients with a family history of colorectal cancer, especially those over the age of 40, should undergo annual medical examination and genetic testing.
Virtual colonoscopy
Early diagnosis of colon cancer is also carried out using virtual colonoscopy, which is performed using MRI or CT. A special contrast agent is injected into the patient’s body, which is evenly distributed throughout the blood and is displayed on the screen with a bright glow.
During a CT or MRI scan, the specialist takes a series of images in which clusters of light are visible at the sites of tumor formations.
Despite its high productivity, the method has (your doctor will tell you a list of contraindications under which the procedure cannot be performed).
Treatment for different stages
Early stages of colon cancer are highly treatable. The survival rate is more than 40%. However, even with an advanced form of cancer, there is a possibility of a successful outcome. It all depends on the treatment tactics chosen by the doctor and the body’s overall resistance to the disease.
- Stage 0 is a non-invasive type of cancer that can be removed without consequences to the body using polypectomy.
- Stage 1 - the tumor begins to grow deeper into the intestinal wall, the lymph nodes and nearby organs are not affected by tumor cells. The main treatment is anterior rectal resection. Additionally, radiation or chemotherapy may be prescribed.
- Stage 2 - cancer affects all layers of the intestinal mucosa and begins to gradually spread to nearby tissues. A cancer patient is shown two stages of radiation and/or chemotherapy in combination with surgery.
- Stage 3 - the disease metastasizes to regional lymph nodes, but there is no damage to neighboring organs. Combination therapy is indicated, combining preoperative chemotherapy, surgery and a postoperative course of chemotherapy.
- Stage 4 - there is extensive damage to other organs by malignant cells. Treatment involves resection of the intestine and subsequent partial removal of the organ affected by cancer. Next, the patient is prescribed an intensive course of chemotherapy. The oncologist, monitoring the patient’s condition and the dynamics of the disease, can prescribe additional treatment (chemotherapy, radiation therapy).
IMPORTANT:
If the tumor is not operable, the patient is prescribed only chemotherapy.
Kinds
Based on histological characteristics, intestinal cancer is divided into:
- adenocarcinoma - a formation of malignantly changed glandular cells and occurs in 95% of all cases of the disease;
- lymphoma - a tumor formed from fibrous tissue of the intestinal wall;
- carcinoma - a formation consisting of epithelial cells;
- sarcoma is a malignant tumor that forms mainly on the outer wall of the intestine from connective tissue cells;
- melanoma - the basis are skin cells called melanocytes.
Tumors are classified according to the type of growth:
- exophytic - growing on the inner wall in the intestinal lumen, as a result of which obstruction of the organ gradually develops;
- endophytic – growing into the intestinal wall with subsequent formation of ulcers and a high risk of metastases upon contact with healthy tissues;
- diffuse – tumors growing to the sides from the focus without narrowing the intestinal lumen;
- mixed - having characteristics of two or three of the listed types.
Diagnostic methods
Fortunately, bowel cancer can be detected early. Genetic tests are used for this. They allow you to confirm or refute the presence of gene mutations in cells. And if colorectal cancer does develop, the patient will know about it earlier and, therefore, will have a chance for a full recovery.
What screenings for colorectal cancer should be performed in patients who have warning signs?
- blood tests (general, biochemistry, CEA);
- stool occult blood test;
- examination of the rectum (through the anus);
- Colonoscopy - an alternative to stool occult blood testing (examination with a camera inserted into the intestines through the anus) - every 10 years as a preventive measure in all men and women over 50 years of age. In patients over 65 years of age, the frequency of colonoscopy depends on the individual decision of the physician;
- rectoscopy (examination of the final section of the rectum about 30 cm long through a special mirror);
- virtual colonoscopy, that is, colonography (study of a three-dimensional image of the intestine using images obtained using a computed tomograph);
- biopsy - taking a tissue sample to study the degree of malignancy of the tumor;
- PET/CT/MRI - helps determine the location and size of the tumor.
- determination of the concentration of marker 5 CEA in the blood.
Colonoscopy and stool occult blood testing are preventive tests recommended for early detection of the disease. They are usually performed on people without symptoms.
Rectoscopy, examination of tumor markers for intestinal cancer, virtual colonoscopy and a number of other additional diagnostic tests useful for making a diagnosis are performed as part of an in-depth diagnosis of patients, whose attending physician decides on the need for them based on the medical history and the results of previous examinations.
All of the above studies can lead to a diagnosis, but do not give a clear answer as to whether it is colorectal cancer. A definite diagnosis can only be made by histopathological examination, that is, taking a sample of the affected tissue, such as a tumor or polyp, and analyzing it.
Recovery after chemotherapy
Most chemotherapy side effects go away fairly quickly after treatment is completed. But some last a long time. This depends on the type of chemotherapy drugs used, their dosages and course duration, the presence of concomitant health problems in the patient, and the body’s individual reaction to the drugs.
You will receive detailed recommendations from your doctor on how to eat properly and organize your lifestyle as soon as possible, when you can return to work and physical activity.
Many chemotherapy drugs have a strong effect on the reproductive system, so if you are planning a child, you will have to wait. The doctor will tell you when you can plan to conceive and what contraceptives are best to use before that.
Chemotherapy weakens the immune system. At the first signs of infection (fever, cough, shortness of breath, diarrhea, skin rash), you should immediately consult a doctor.
Treatment methods
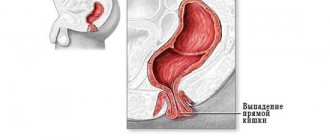
The main treatment method for rectal cancer is surgery (removal of the malignant tumor). Surgery may be preceded by radiation therapy. The malignant tumor is excised along with the surrounding healthy portion of the intestine and, most often, the surrounding lymph nodes.
If possible, the remaining sections of the intestine are stitched together. However, it may be that suturing is impossible, then an artificial anus is formed, that is, a stoma is an opening in the abdominal wall into which the end of the large intestine is placed. Outside the opening there is a plastic container into which feces fall. For some patients, this condition can cause a decrease in quality of life, but the stoma may allow you to function normally for several years. In some cases, removal of the so-called artificial anus is necessary for life, but sometimes only until the intestinal anastomosis heals.
If the diagnosis of colorectal cancer is confirmed, surgery on multiple organs may be required. Not only a fragment of the intestine is cut out, but also other organs affected by cancer, for example, a fragment of the liver, stomach, kidneys, abdominal wall or ovary.
Additional radiation and chemotherapy may be required after surgery. Postoperative rehabilitation is required.
Treatment survival statistics
The prognosis for bowel cancer depends on a number of factors, so it is impossible to predict the success of therapy with certainty. Unfortunately, 80% of patients with colorectal cancer are diagnosed with advanced stage disease. About 40% of cases are inoperable. There is no cure for them, and the only thing patients can count on is relief of symptoms and slowing down the progression of the disease.
What about the other 60% of patients? If the disease is diagnosed at stage I, the 5-year survival rate reaches 90%. This does not mean that the patient will live only 5 years. On the contrary, it means that the disease is under control and the risk of cancer recurrence after 5 years is low.
If colorectal cancer is detected at the last stage, when metastases have already appeared in other organs and their removal is impossible, the 5-year survival rate is only 7%. If metastases are surgically removed - 25-35%. The average survival rate of patients with colorectal cancer is 40%.
Most often, cancer metastases affect the liver through the blood and lymphatic vessels, less often the lungs, ovaries, adrenal glands, brain and bones.
What is different about colon cancer treatment at the 21st Century Oncology Clinic?
- Low-traumatic laparoscopic operations, including the use of an ultrasonic scalpel and electroligating devices.
- At the initial stages, we use endoscopic operations without incisions with tumor removal under the control of a colonoscope.
- Colonoscopy using the latest optical equipment, can be performed under sedation.
- A cold helmet is available under compulsory medical insurance -
a procedure that prevents hair loss after chemotherapy. Chemotherapy with modern drugs with low toxic effect.