Proper preparation for a colonoscopy is a guarantee of obtaining a reliable and clear assessment of the condition of the intestines. Its goal is to cleanse the rectum of accumulated feces using medications, enemas and a special diet.
Diet 1-2 days before colonoscopy
Allowed | Forbidden |
All protein foods:
Liquids:
| All plant foods:
Liquids:
|
Taking FORTRANS®
HOW TO PREPARATE FORTRANS® SOLUTION
- Dissolve the contents of each Fortrans package in 1 liter of high-quality drinking water at room temperature until completely dissolved
RECOMMENDATIONS FOR TAKING FORTRANS®
- Drink the FORTRANS® solution in small sips, 250 ml every 15 minutes (do not drink in one gulp). At the beginning of taking the drug solution or when taking it quickly in a large volume, nausea/vomiting may occur.
- It is forbidden to reduce the volume of liquid to prepare the FORTRANS® solution.
- To make it easier to tolerate the taste of FORTRANS®, you can add lemon juice to the solution to improve its taste. Persons sensitive to large volumes of liquid (nausea, belching, etc.) are recommended to take 1 tablet of Motilium 1 hour before the start of preparation. It is not recommended to take the drug quickly. Otherwise, bowel cleansing will be incomplete. With rapid use, there is also a high probability of side effects in the form of nausea and vomiting.
- You should not eat solid food from the start of taking FORTRANS® until the end of the examination.
- If intravenous anesthesia (sedation) is not expected, then on the day of the examination after preparation, you can drink sweet tea and permitted liquids. You should stop taking all liquids no later than 2 hours before the examination.
- If the examination is to be performed under intravenous anesthesia (sedation), then eating is prohibited on the day of the examination.
- While taking FORTRANS®, it is recommended to maintain physical activity (walk around the apartment, perform circular movements with the body, bending to the sides, back and forth, squats).
- The onset of action of the drug develops on average 1-1.5 hours from the start of taking FORTRANS®. The active effect of the drug lasts on average 1.5–2 hours after administration - during this time there will be intense loose stools on average 12–15 times (depending on the individual characteristics of the patient). At the end of taking the drug, the stool should change to a clear, colorless liquid, which indicates the patient’s readiness for examination.
- At least 4 hours must pass from the end of taking Fortrans to the examination. Patients need to consider the appropriate time slot for traveling to the clinic.
- It is not necessary to additionally (or instead) carry out the procedure of cleansing the colon with enemas.
- It is not recommended to take petroleum jelly. RECOMMENDATIONS FOR RELATED DISEASES:
- Accelerated transit of intestinal contents leads to a sharp decrease or complete absence of the therapeutic effect of other drugs taken before or during the preparation and examination. This should be taken into account if the patient is constantly taking hormonal, cardiac, antihypertensive and other vital drugs, the use of which should not be interrupted.
- It is recommended to discontinue iron supplements 2–3 days before the examination.
- For chronic constipation, 3–5 days (depending on the severity of constipation) before the examination, start or continue taking non-herbal laxatives on the recommendation of a gastroenterologist. The diet should be started no earlier than 5 days before the examination.
- If the patient is taking antiglycemic drugs, it is recommended to refrain from taking them in preparation for the examination and return to taking them after the start of normal nutrition. There is no need for the patient to fast (especially with diabetes) on the day of the examination. Immediately before a colonoscopy, it is permissible to drink tea with sugar/honey if sedation is not planned.
- If the patient is taking medications that normalize blood pressure, heart rate, etc., they must be taken as standard! It is recommended to take these medications no earlier than 1 hour after finishing FORTRANS®! If the patient is taking blood thinning medications, the endoscopist should be informed about this before the examination.
- If an examination is to be carried out under intravenous anesthesia, it is not recommended to drive a car, operate any machinery, or make important decisions on this day. It is advisable that the patient be met and escorted home.
Preparation for colonoscopy using the drug "Moviprep" or "Fortrans"
| Colonoscopy time | Diet | Dosage regimen |
| 08:00 — 10:00 | Until 09:00 breakfast: according to the list of permitted products. Lunch and dinner: only permitted liquids. | One-stage evening scheme. the day before the colonoscopy: 19:00-20:00 take the first liter of the drug solution. 21:00-22:00 take the second liter of the drug solution. After each liter of the drug taken, do not forget to drink 500 ml of the approved liquid. |
| 10:00 — 14:00 | Breakfast: according to the list of permitted products. Until 13:00 light lunch: according to the list of permitted products. Dinner: only permitted liquids. | Two-stage scheme. the day before the colonoscopy: 20:00 - 21:00 take the first liter of the drug solution. Day of colonoscopy: 06:00-07:00 take the second liter of the drug solution. After each liter of the drug taken, do not forget to drink 500 ml of the approved liquid. |
| 14:00 — 19:00 | Breakfast and lunch: according to the list of permitted products. Until 18:00 light dinner: according to the list of permitted products. On the day of colonoscopy in the morning: only permitted liquids. | One-step morning routine. Day of colonoscopy: 08:00-09:00 take the first liter of the drug solution. 10:00-11:00 take the second liter of the drug solution. After each liter of the drug taken, do not forget to drink 500 ml of the approved liquid. |
Enema before colonoscopy
A traditional enema is used before surgery, diagnostic procedures, and as preparation for nutritional cleansing. Enema is also used for endoscopic examination of the intestines, including colonoscopy. How to do an enema before a colonoscopy? You can read about this in our article.
Preparing for a colonoscopy at home
After ordering an examination, the attending physician usually gives the patient recommendations on what to do at home before a colonoscopy.
To obtain reliable information, speed up the procedure and avoid repeated manipulations, the patient must be well prepared at home.
To achieve this, a whole range of measures are determined, including observing a certain week without silk for three to four days and carrying out colon cleansing the day before the examination.
Full preparation for the exam is possible with a planned procedure. In the event of an emergency or a quick intervention in an emergency, a colonoscopy can be arranged as soon as possible. For example, if a colonoscopy is scheduled for the morning, it also needs to be prepared. With the exception of food, only small amounts of water can be consumed.
Before going to bed, you should take a standard dose of the drug for constipation, do physiological recovery in the morning, and before the manipulation do a cleansing enema.
This tactic will clear out the rectum, sigmoid colon, and colon as quickly as possible.
Usually, a colonoscopy is not performed without preparation; even in the case of organ failure, at least a siphon enema must be done before receiving clean water. Otherwise, the examination does not provide a complete picture of the pathology.
In case of constipation, the examination is carried out after a diet for at least three to four days. Bowel cleansing actions are performed before virtual colonoscopy.
Is it possible to do an enema before a colonoscopy - indications and limitations
The most important enema cleansing recipes are constipation, surgical procedures, preparation for the birth process. The need for an enema also arises in cases of poisoning, chronic poisoning of any origin, or before the introduction of special nutrients.
The main indications for enemas before colonoscopy are:
- Long-term constipation;
- Unstable stool frequency:
- Pain on the right side of a vague nature;
- Poor breathing, acid belching;
- Fatigue and weakness;
- Apathy;
- Allergic reactions to drug cleansing.
Note
Indications
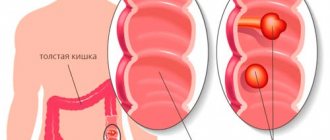
A colonoscopy is required if the patient is concerned about the following problems:
- Inflammatory processes in the rectum: a feeling of fullness in the intestines, pain in the perineum, the left side of the abdomen, mucus discharge from the anus, itching of the anus, a false urge to defecate (a constant feeling that you need to go to the toilet for a long time).
- Inflammation of the sigmoid colon. The pathology is accompanied by rumbling, bloating, and the presence of impurities in fecal matter.
- Chronic constipation.
- Constant sensation of a foreign body in the anal area.
- Prolonged diarrhea in the absence of signs of intoxication.
- Fast weight loss.
For preventive purposes, colonoscopy is also recommended for everyone over 55 years of age, with a family history (proctitis, sigmoiditis, cancer pathology and immediate family members), as well as for people who have previously undergone intestinal surgery.
Contraindications
Colonoscopy is a low-traumatic (non-invasive) procedure. Meanwhile, a number of cases are contraindications to its implementation:
- Thrombosis of hemorrhoids, accompanied by the formation of blood clots in the plexuses, vessels of the rectum,
- Severe anal fissures,
- Just undergone surgery in the gastrointestinal tract. Rectosigmocolonoscopy is important not only as a diagnostic, but also as a control procedure, but if the patient has undergone gastrectomy or colon surgery, at least half a month must pass between the operation and diagnosis through a colonoscope.
- Exacerbation of Corona disease: severe frequent bowel movements, constant abdominal pain, protein disturbances, progressive anemia, fever, chills.
- A state of shock accompanied by extremely low blood pressure (upper - systolic - below 70 mm Hg)
- Peritonitis is a purulent-inflammatory process in the abdominal cavity.
- Heart failure in the stage of decompensation, acute cardiac ischemia and myocardial infarction.
- Perforation (perforation changes - the formation of through holes) in the intestinal wall and the release of blood into the abdominal cavity.
How is the procedure done?
- For diagnostics, a thin probe is used, at the end of which there is a video camera.
- The probe is inserted through the anus.
- The patient lies on his left side, knees bent.
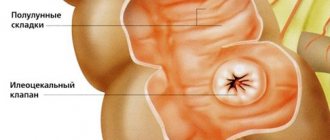
- The doctor inserts the colonoscope through the anus into the rectum and uses the system to supply air. This is important for expanding the intestinal lumen. The enlarged image is displayed on the monitor. Gradually advancing and turning the endoscope, the doctor examines the inner surface of the rectum and all parts of the colon.
- If neoplasms are visible on the screen, then biopsy tests are immediately taken to deny/confirm cancer.
Important! After the diagnosis, you need to fully launch the digestive system. For several days after colonoscopy, it is recommended to refrain from fatty foods, and give preference to boiled beef or chicken, steamed vegetables, and low-fat kefir.