In what clinical situations is bougienage necessary?
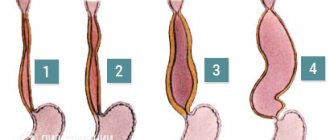
Narrowing of the cervical canal can be either congenital or acquired. Injuries to the cervix during childbirth, accompanied by extensive ruptures, lead to disruption of the patency of the cervical canal. Curettage of the uterus during abortion and diagnostic curettage of the canal itself, complicated by infection, can also lead to scarring.
This type of complication can occur a long time after cauterization and excision of pathological changes in the cervical mucosa, when scars that deform the canal form at the site of exposure.
Severe chronic inflammatory processes of the vagina or endometrium cause swelling and sticking of the canal walls, followed by scar tissue.
Age-related changes in structure and dry tissue with prolapse of the genital organs also deform and narrow the passage.
Stomach
Considering the emergence of highly effective antiulcer therapy and a significant reduction in the frequency of ulcer recurrences after successful HP eradication, balloon dilatation can be successfully used for cicatricial narrowing of the pylorus and duodenum as an alternative to surgical intervention. Of course, there is no point in dilation with decompensated stenosis. Dilatation is also possible for malignant ones, as palliative treatment, and after burn strictures, anastomotic strictures. Solt J., et al., published long-term results of dilatation in patients with benign gastric outlet stenosis (after surgery, peptic, corrosive and post-vagotomy strictures) [15]. He performed 117 balloon dilations on 72 patients and had a mean follow-up of 98 months. The average diameter of the stenosis was 6 mm before treatment and 16 mm after it. Reduction and disappearance of symptoms was observed in 80% immediately after the procedure and in 70% after three months. In 16 patients, restenosis was observed within 1-18 months after the intervention. Complications included one case of arterial bleeding and two perforations. Boylan JJ, and Gradzka MI, emphasize that proper antiulcer treatment, especially HP eradication and cessation of NSAIDs, is necessary to maintain the result of successful dilatation for gastric outlet stricture of peptic nature [2]. Anastomotic strictures and strictures of a malignant nature are more prone to rapid recurrence [11].
How is the procedure performed?
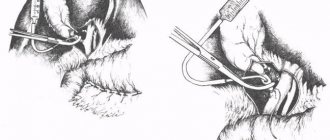
The essence of the method: with the help of a special instrument - a bougie, inserted into the cervical canal, it expands to normal patency. Bougies have different diameters and are selected individually depending on the anatomical features of the patient. As a rule, if a woman does not have concomitant severe pathology from the cardiovascular and hematopoietic systems, bougienage of the cervical canal is performed on an outpatient basis.
If the cervical canal is narrowed, but not completely closed, then the manipulation can be performed under local anesthesia. In the case of complete fusion, atresia is treated with intravenous anesthesia. Through the vagina, under visual control, bougies are inserted alternately into the cervical canal, the diameter of each subsequent instrument being larger than the previous one. There is a gradual mechanical expansion of the cervical canal with restoration of its patency. After the procedure and recovery from anesthesia, the woman is allowed to go home.
Technical aspects
The advantage, at least theoretically, of balloon dilatation over bougienage is its uniform impact throughout the stricture and the virtual absence of axial load on the tissue.
Currently, there are three types of balloons: those installed along a guide under X-ray control, those installed through an endoscope channel under visual control, and a combination of the first and second types (balloons for dilatation of biliary strictures). Balloons for endoscopic dilatation of strictures are shown in Fig. 1.
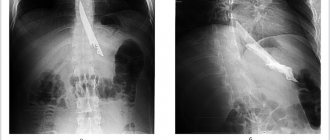
When using a guide, it is passed through the stricture (using an endoscope or X-ray control), a balloon (with X-ray contrast marks) is passed through it, which is installed so that the stricture falls on its central part, then using a special inflating device the balloon is filled with water-soluble contrast up to a certain pressure (specified by the manufacturer for each cylinder of a specific diameter). Initially, a “waist” is clearly visualized on the balloon in the area of narrowing, which disappears with successful dilatation.
Balloons designed to be passed through an endoscope can be installed in two ways:
- If the device can be passed through the stricture, which happens, however, relatively rarely. Then, after overcoming it, the balloon is completely removed from the canal and then the device begins to be removed along with the balloon until its correct location in the stricture is achieved.
- If the stricture is insurmountable, the device attempts to “cannulate” the area of stenosis with a balloon.
Successful dilatation is judged by the ability of the inflated balloon to move back and forth across the stricture.
In our work, we use a combination of endoscopic and radiological control for balloon installation and dilatation. The dilator is passed through the endoscope channel and, under X-ray control, is installed in the center of the narrowing. Inflation is carried out under X-ray control until the “waist” disappears, but without exceeding the maximum recommended pressure.
We usually keep the balloon inflated in the area of the stricture for 2-3 minutes. Then the balloon is deflated and removed from the canal. The area of the eliminated stricture and previously inaccessible areas of the gastrointestinal tract due to it, for example, the stomach and duodenum with esophageal strictures, are examined endoscopically.
The question that remains quite difficult to resolve is: to what diameter should dilatation be carried out? On the one hand, there is evidence that perforation occurs more often when using a balloon with a diameter of 18 mm, at least when it is used to treat stenoses of the gastric outlet [5], on the other hand, clinical symptoms are closely related to the diameter of the narrowing. When using balloons (or bougies) to dilate esophageal strictures, it is recommended to dilate the stricture in one session by 6-10 F compared to its initial diameter [19]. This approach seems to us to be reasonably cautious; we try not to dilate strictures, regardless of their location, by more than 10 F during a single procedure. For esophageal strictures, some authors recommend dilatation to achieve a lumen of 14-15 mm (42-45 F) [13]. As for colonic strictures, there is evidence that after dilation of colonic anastomotic strictures to 40 F, symptoms of obstruction disappeared in 90% of patients [4]. In our work, in the vast majority of cases, we use a balloon with a diameter of no more than 16 mm due to the increased risk of perforation and virtually no difference in symptoms in patients with strictures extended to 16 and 18-20 mm.
It is necessary to adequately prepare the patient for dilatation - with severe strictures of the esophagus and gastric outlet, the overlying sections may contain a large amount of fluid and remnants of food eaten the day before. It is necessary to wash the contents through the probe. Adequate preparation is also extremely important to eliminate colonic strictures.
Like other therapeutic endoscopic interventions, dilatation should be performed only with adequate sedation of the patient.
Before the procedure, an endoscopic examination of the stricture with a biopsy and an X-ray examination with barium are required. A study with water-soluble contrast is also performed after dilatation to exclude perforation. Repeated endoscopic examination is also recommended to exclude complications. Sometimes it is reasonable to take a second biopsy from the area of narrowing to rule out a malignant nature of the lesion.
Indications for dilatation are only strictures with obvious clinical symptoms and sometimes the need to exclude its malignant nature, such as strictures arising against the background of ulcerative colitis.
Expected Consequences
Complications after bougienage are extremely rare; antibacterial treatment is prescribed to prevent inflammation. It is not recommended to engage in heavy work for some time. Given the inflammatory nature of the infection, the likelihood of adhesions forming in the future cannot be ruled out. In case of relapse, you can repeat the procedure.
For any gynecological disease, the specialists of the Medicine 24/7 Clinic will do everything possible that is known to healthcare and is in the annals of medical science, so that the patient feels like a full-fledged woman, to whom all the joys of a healthy person are available. Sign up for a consultation: +7 (495) 230-00-01.
The material was prepared by gynecologist, oncologist at the Medicine 24/7 clinic, candidate of medical sciences Alimardonov Murad Bekmurotovich.
Esophagus
The main indications for dilatation are peptic and caustic strictures. Dilatation of tumor narrowings and anastomotic strictures is also possible. Dilatation is also successfully used for achalasia cardia. In our experience, the most rewarding are short narrowings of the lumen of a peptic nature. When adequate antisecretory therapy is prescribed, such strictures rarely recur.
Dilatation in strictures resulting from burns of the esophagus with acid or alkali is the most difficult (due to the often high extent, tortuosity and density of the narrowing). Often a series of dilations with balloons of different diameters (from small to large) is used over 3-7 days. The recurrence rate of such strictures is high.
Tumor stenoses are, as a rule, easy to dilate, but the elimination of dysphagia is rather short-term. In a series of 39 patients with esophageal cancer, dilation reduced dysphagia in 90% of patients; complications included one perforation [12]. Dilations for tumor strictures can be performed repeatedly, with repeated appearances of dysphagia. According to one study, patients with this pathology typically required repeat dilatation every 4 weeks [10]. After eliminating the tumor stenosis, it is necessary to perform stenting with a self-expanding metal stent, which, however, in Russia is not always possible for financial reasons. There are reports of the successful combination of dilatation with chemotherapy as a palliative treatment for inoperable tumors of the cardia [7].
When dilating strictures of esophageal anastomoses, the results are more favorable for short strictures (if their length is more than 12 mm, balloon dilatation is generally ineffective), but the result does not depend on the diameter of the narrowing. The results are worse with manual anastomoses and with a history of their failure [6].
Small and large intestine
The main indications for dilatation are strictures due to Crohn's disease or UC and anastomotic strictures. Although there are reports of the use of this method for diverticular, tumor and ischemic strictures [8]. A retrospective analysis of balloon dilatation of strictures through a colonoscope in 59 patients with Crohn's disease (53 with anastomotic strictures and 6 with primary strictures) showed that a long-term positive result was achieved in 41% of patients, and in 17% after one dilation. However, in 59% of patients during the observation period, there was a need for surgical treatment as a result of stricture recurrence. Complications included two perforations [17]. Brooker JC, et al., reported the combination of balloon dilatation with the administration of long-acting steroids for strictures resulting from Crohn's disease [3]. In 50% of patients, remission was achieved after one dilatation with the introduction of steroids, in 28.5% several interventions were required, and, finally, in 21.4% of cases dilation was not effective.
When dilating colonic anastomotic strictures, balloon dilatation has proven to be more effective than bougienage [14]. Virgilio C., et al., using a balloon intended for the treatment of achalasia to dilate anastomotic strictures with a diameter of 2 mm or less, achieved results in 94% of cases [18].
Tumor strictures of the colon are dilated both for the purpose of emergency decompression [1] and for better preoperative preparation [16] or palliative treatment, in the latter case the installation of metal self-expanding stents is preferable.