Laparoscopy is a method of visual examination of the abdominal and pelvic organs using a miniature video camera-laparoscope, which is inserted inside through a small puncture of soft tissue.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
Diagnostic laparoscopy is a minimally invasive examination method. At the same time, it provides significant advantages, since the doctor can visually examine the internal organs and examine them in detail.
In some cases, visual examination of organs through laparoscopy provides more valuable information than x-rays, ultrasound, CT or MRI. The laparoscope video camera has a high resolution; the image from it is transmitted to the monitor and can be enlarged many times. This makes it possible to detect tumors of the smallest size at an early stage of the development of cancer.
What organs can be examined by laparoscopy?
Diagnostic laparoscopy is used to examine the abdominal organs, as well as in gynecology, to examine the pelvic organs and female reproductive system.
In recent decades, the use of this method has become increasingly widespread. Doctors are fully appreciating its benefits and are using it more and more often.
At the Medicine 24/7 clinic, laparoscopy is used to examine:
- liver,
- gallbladder,
- stomach,
- spleen,
- intestinal loops,
- greater omentum,
- diaphragm,
- Bladder,
- fallopian tubes,
- uterus,
- ovaries.
Advantages
Diagnostic laparoscopy is actively used in the Medicine 24/7 clinic due to its advantages:
Maximum information content
During laparoscopy, the doctor can not only examine the internal organs in detail, but also take a tissue sample from a suspicious area or tumor.
The procedure for collecting a tissue sample is called a biopsy, and the tissue sample itself is called a biopsy. After receiving the biopsy, it is sent for histological examination. In the laboratory of the Medicine 24/7 clinic, a doctor examines the cellular structure of tissue under a microscope.
This allows us to make an unambiguous conclusion about the benign or malignant nature of the neoplasm.
In the second case, histological examination shows the degree of malignancy of the tumor (differentiation of cancer cells), its type. This is invaluable for choosing treatment tactics for cancer.
During a histological examination of a biopsy obtained during pelvic laparoscopy, the doctor examines the sensitivity of the tumor to hormones (estrogens, progesterone), as well as the presence of HER2 protein receptors. Sensitivity to various chemotherapy drugs is studied. The tactics of chemotherapy, immunotherapy, targeted therapy, and the decision to use certain drugs depend on this.
The risk of relapse after removal of the tumor, and therefore the extent of surgical intervention, depends on the degree of malignancy of the tumor (differentiation of tumor cells).
Thus, diagnostic laparoscopy is not only a visual examination of the internal organs of the abdominal cavity and pelvis, but also a way of taking tissue samples (biopsies), examining them and obtaining information that cannot be obtained by any other means.
Minimal invasiveness
The laparoscope and biopsy instruments are inserted into the abdominal cavity or pelvic area through small punctures. The procedure does not require incisions like open surgery. After it there are no scars left, there is no need for stitches.
The traumatic effect on soft tissues during diagnostic laparoscopy is minimal. Therefore, it does not produce side effects, complications and is highly safe.
Fast rehabilitation
After laparoscopy, a long rehabilitation period is not required, which also distinguishes it favorably from open surgical interventions.
In general, laparoscopy helps the doctor obtain maximum diagnostic information with minimal surgical intervention. This determines its widespread use in the diagnosis of cancer and other diseases.
Request a call back. We work around the clock
UDC 616.37-002-036.11-08
A.M. ZAINUTDINOV, I.S. MALKOV
Kazan State Medical Academy, 420012, Kazan, st. Butlerova, 36
Zainutdinov Azat Minvagizovich - Candidate of Medical Sciences, Associate Professor of the Department of Surgery, Head of the Department of Surgery of the Republican Clinical Hospital No. 2, tel. +7-917-268-25-34, e-mail: ru
Malkov Igor Sergeevich - Doctor of Medical Sciences, Professor, Head of the Department of Surgery, tel. +7-965-594-40-07, e-mail:
The article defines indications and contraindications for laparoscopy in acute pancreatitis. The morphological picture of various forms of acute pancreatitis, the main surgical procedures during laparoscopy and indications for them are described. The use of laparoscopy in acute pancreatitis in 291 patients was analyzed. The use of laparoscopy in the treatment of patients with acute pancreatitis has increased surgical activity and reduced overall postoperative mortality to 13.4%.
Key words: acute pancreatitis, treatment, laparoscopy.
AM ZAINUTDINOV, IS MALKOV
Kazan State Medical Academy, 36 Butlerov Str., Kazan, Russian Federation, 420012
Therapeutic and diagnostic laparoscopy in the treatment of patients with acute destructive pancreatitis
Zainutdinov AM - Cand. Med. Sc., Associate Professor of the Department of Surgery, Head of the Department of Surgery of Republican Clinical Hospital No. 2, tel. +7-917-268-25-34, e-mail:
Malkov IS - D. Med. Sc., Professor, Head of the Department of Surgery, tel. +7-965-594-40-07, e-mail:
The article gives indications and contraindications for laparoscopy in acute pancreatitis. The morphological features of various forms of acute pancreatitis are described, as well as the basic surgical procedures for laparoscopy and indications for them. Analysis is given of laparoscopy of 291 patients with acute pancreatitis. Using laparoscopy in treatment of acute pancreatitis allowed to increase the surgical activity and reduce the overall postoperative mortality rate to 13.4%.
Key words : acute pancreatitis, treatment, laparoscopy.
The mortality rate for infected pancreatic necrosis ranges from 20 to 80%, especially with traditional surgical approaches [1-7]. The most effective methods of treating patients with acute destructive pancreatitis are minimally invasive surgical interventions [8-12]. The use of laparoscopic technologies in the abdominal cavity and retroperitoneal space for pancreatic necrosis is finding more and more supporters and has further development prospects [13, 14]. In connection with the above, we set a goal - to improve the use of laparoscopic technologies in the treatment of patients with acute pancreatitis.
Material and research methods
Of the 291 patients with acute pancreatitis who were treated in the clinics of the Department of Surgery of the KSMA, therapeutic and diagnostic laparoscopy was performed in 256 (88%) men, 35 (12%) women aged 17 to 84 years. The average age was 42.4 years. Indications for laparoscopy were progression of pancreatogenic peritonitis, a combination of acute pancreatitis with destructive cholecystitis, obstructive jaundice, and differential diagnosis with other acute surgical diseases. An absolute contraindication is the terminal condition of the patient. Relative contraindications were considered unstable hemodynamics, previous operations on the stomach and pancreas, and large postoperative ventral hernias.
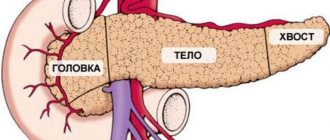
The objectives of laparoscopy at the diagnostic stage were: confirmation of the diagnosis and morphological form of the disease (presence of edema, exudate with high amylase activity, areas of steatonecrosis), identification of signs of severe pancreatitis (hemorrhagic effusion, widespread steatonecrosis, extensive hemorrhagic soaking), at the treatment stage - removal of peritoneal exudate , decompression of retroperitoneal tissue, biliary tract.
Criteria for the severity of pancreatic necrosis, according to laparoscopy, are the nature of the exudate, damage to the retroperitoneal tissue, and area of the lesion. Endosurgical interventions were performed under general anesthesia with pneumoperitoneum corresponding to 9-11 mm Hg. Art.
The optimal placement of instruments in the abdominal cavity was as follows. During the work, 4 trocars were used. The first 10 mm trocar for the laparoscope was inserted 1 cm above the umbilicus along the midline of the abdomen. The second 10 mm trocar for retracting the liver and, if necessary, the stomach is located to the right of the xiphoid process. The third trocar (5 mm) for work in the right paracolic space and omental bursa was placed along the midclavicular line at the level of the umbilicus on the right. The fourth trocar (5 mm) for work in the left paracolic space, manipulations in the omental bursa is located 2 transverse fingers above the navel on the left along the midclavicular line. The points of trocar insertion during diagnostic and treatment laparoscopy in patients with acute destructive pancreatitis are presented in Figure 1.
Picture 1.
Points of insertion of trocars during therapeutic and diagnostic laparoscopy in patients with acute pancreatitis
results
Therapeutic and diagnostic laparoscopy for pancreatogenic peritonitis in 63% of cases was performed on the first day after hospitalization, 29% - after 48 hours, 8% - at a later date. The performance of laparoscopy at different periods of hospitalization depended on the presence of pancreatogenic peritonitis and the effectiveness of conservative therapy. For differential diagnosis, laparoscopy was performed in 97% of cases on the first day of hospitalization. Laparoscopy was performed according to absolute indications, mainly in the clinical picture of pancreatogenic peritonitis - 49% and during differential diagnosis - 43%. At the same time, laparoscopy was performed in 63% of cases on the first day, in 29% on the second day, and in 85 cases on the third day. For the purpose of differential diagnosis, laparoscopy was performed on day 1 in 97% of patients. Laparoscopy initially required the installation of 1 and 3 trocars to examine the abdominal cavity. The examination was carried out in accordance with the protocol: the abdominal cavity was examined to identify effusion, assess its nature and take fluid for amylase activity or the Actim-Pancreatitis test to confirm the diagnosis or for the purpose of differential diagnosis. The abdominal cavity was washed with various antiseptics, including a 0.05% aqueous solution of chlorhexidine gluconate, saturated with carbon dioxide until amylase activity decreased or the Actim-Pancreatitis test was negative using the Brusan apparatus [15, 16].
Next, the gastrocolic ligament, lesser omentum, and lig. mesocolon, paracolic spaces on the left and right. To carry out these manipulations, a change in the patient's position was required: raising the head end, turning the body and using additional trocars 2 and 4. In the case of a large amount of effusion in the retroperitoneal space, lig. mesocolon, omental bursa, mobilization of paracolic spaces, dissection of the colic-splenic ligament, and opening of the peritoneum lig. mesocolon, through drainage of the omental bursa at the lowest point; in case of local accumulation of fluid, normal drainage was performed. Drainage of the gallbladder was carried out according to indications: for hypertension of the biliary tract, obstructive jaundice. The round ligament of the liver was drained for lymphotropic therapy. The operation ended with drainage of the abdominal cavity, and, if necessary, the retroperitoneal space with traditional drainages and drainages of an original design.
In 21 patients, with an increase in endotoxicosis and enzymatic peritonitis, despite primary diagnostic and therapeutic laparoscopy or in case of discrepancy between the clinical picture of endotoxic shock and the pathomorphological picture in the form of vitreous edema and the absence of steatonecrosis and hemorrhagic effusion, programmed laparoscopic sanitation of the abdominal cavity was performed. Moreover, in 13 patients it was performed as a programmed sanitation, when the morphological picture determined the indications for repeated laparoscopic treatment of the abdominal cavity. In 8 patients, forced repeat laparoscopy was performed due to the lack of clinical effect from the sanitation. Repeated laparoscopic sanitation in 64% of cases required the introduction of all trocars (1, 2, 3, 4) (Fig. 2) and compliance with the manipulation protocol outlined during the “primary” laparoscopy. During programmed sanitation, a 0.05% aqueous solution of chlorhexidine gluconate, saturated with carbon dioxide, was used, which showed effectiveness compared to traditional antiseptics (0.05% aqueous solution of chlorhexidine gluconate, ozonated NaCl solution 0.9%) against nosocomial strains in the experiment and in the clinic . The operation also ended with drainage of the abdominal cavity, if necessary, the retroperitoneal space, and the omental bursa.
Sanitation of purulent-inflammatory formations in the retroperitoneal space and abdominal cavity, if necessary, was carried out in two sessions per day for 10-20 minutes, depending on the stage of the wound process, which does not require drainage. The antiseptic solution was prepared by bubbling carbon dioxide into 500 ml of a hermetically sealed 0.05% aqueous chlorhexidine solution for 5 minutes until a fine fraction of the antiseptic solution was formed.
The use of laparoscopy made it possible to increase surgical activity and reduce overall postoperative mortality to 13.4%, for moderate pancreatic necrosis to 5%, and for severe pancreatic necrosis to 26%.
Discussion
The use of laparoscopy in the treatment of patients with acute pancreatitis has increased surgical activity and reduced overall postoperative mortality to 13.4%. Depending on the severity of the disease, mortality for moderate pancreatic necrosis was 5%, and for severe pancreatic necrosis - 26%. When studying the results of surgical treatment of patients with acute destructive pancreatitis, it was found that therapeutic and diagnostic laparoscopy is most effective in patients with aseptic and infected pancreatic necrosis of moderate severity. The use of laparoscopy in retroperitoneal surgery in patients with destructive pancreatitis is very interesting and promising.
LITERATURE
- Beburishvili A.G., Burchuladze N.Sh., Mandrikov V.V. Staged treatment of acute pancreatitis and its outcomes / 9th All-Russian Congress of Surgeons, 1999. - P. 15-16
- Galperin E.I., Dyuzheva T.G., Dokuchaev K.V. Minimally invasive interventions on the omental bursa and retroperitoneal tissue in the prevention and treatment of infected pancreatic necrosis // International Surgical Congress, 2003. - P. 56.
- Krasilnikov D.M. et al. Surgical tactics in patients with destructive pancreatitis // Practical Medicine. - 2008. - No. 5. - pp. 16-18.
- Savelyev V.S., Filimonov M.I., Gelfand B.R., Burnevich S.Z. Destructive pancreatitis: algorithm for diagnosis and treatment // Consilium Medicum. ― ― T. 2, No. 6. - OnLine.
- Beger HG, Rau B., Mayer J., Pralle U. Natural course of acute pancreatitis // World J. Surg. - 1997. - Vol. 21, No. 3. - P. 130-135.
- Beger HG, Isenmann R. Surgical management of necrotizing pancreatitis // Surg. Clin. N. Amer. ― ― Vol. 79, no. 4. - P. 793-800.
- Frey CF, Brandley EL, Beger HG Progress in acute pancreatitis // Surg. Gynecol. Obstet. ― ― Vol. 167. ― P. 282-288.
- Freeny PC, Hauptmann E., Althaus SJ, et al. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: Techniques and results // Amer. J. of Roentgenology. ― ― No. 170. - P. 969-975.
- Lee MJ, Wittich GR, Mueller PR Percutaneous intervention in acute pancreatitis // Radiographics. ― ― No. 18. - P. 711-724.
- Carter CR, McKay CJ, Imrie CW Percutaneous necrosectomy and sinus tract endoscopy in the management of infected pancreatic necrosis: An initial experience // Ann. of Surg. ― ― No. 232. - P. 175-180.
- Cuschieri A. Pancreatic necrosis: pathogenesis and endoscopic management // Semin. Laparosc. Surg. ― 2002 Mar. - No. 9. - 54-63.
- Hamad GG, Broderick TJ Laparoscopic pancreatic necrosectomy // J. Laparoendosc. Adv. Surg. Tech. ― ― No. 10. - P. 115-118.
- Baron TH, Thaggard WG, Morgan DE, et al. Endoscopic therapy for organized pancreatic necrosis // Gastroenterology. ― ― No. 111. - P. 755-764.
- Malkov I.S., Shaimardanov R.Sh. Acute pancreatitis. - Kazan, 2001. - P. 60.
- Malkov I.S. et al. / Patent No. 2049401 RF, 2000.
- Malkov I.S. et al. / Patent No. 2153888 RF, 2000.
- Malkov I.S., Zainutdinov A.M. et al. / Patent No. 2257201 RF, 2003.
REFERENCES
- Beburishvili A.G., Burchuladze N.Sh., Mandrikov V.V. Etapnoe lechenie ostrogo pancreatita i ego iskhodov [Minimalnoinvazivnye intervention omental and retroperitoneal fat in the prevention and treatment of infected pancreatic necrosis]. 9-y vserossiyskiy s»ezd khirurgov, 1999. Pp. 15-16
- Gal'perin EI, Dyuzheva TG, Dokuchaev KV Choice of rational treatment strategies in patients with acute destructive pancreatitis. Mezhdunarodnyy khirurgicheskiy kongress, 2003. P. 56.
- Krasil'nikov DM et al. Comparative characteristics of different surgical approaches in the treatment of acute destructive pancreatitis. Prakticheskaya meditsina, 2008, no. 5, pp. 16-18 (in Russ.).
- Savel'ev VS, Filimonov MI, Gel'fand BR, Burnevich SZ Surgical tactics in patients with destructive pancreatitis. Consilium Medicum, 2000, vol. 2, no. 6, online.
- Beger HG, Rau B., Mayer J., Pralle U. Natural course of acute pancreatitis. World J. Surg, 1997, vol. 21, no. 3, pp. 130-135.
- Beger HG, Isenmann R. Surgical management of necrotizing pancreatitis. Surg. Clin. N. Amer, 1999, vol. 79, no. 4, pp. 793-800.
- Frey CF, Brandley EL, Beger HG Progress in acute pancreatitis. Surg. Gynecol. Obstet, 1988, vol. 167, pp. 282-288.
- Freeny PC, Hauptmann E., Althaus SJ et al. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: Techniques and results. Amer. J. of Roentgenology, 1998, no. 170, pp. 969-975.
- Lee MJ, Wittich GR, Mueller PR Percutaneous intervention in acute pancreatitis. Radiographics, 1998, no. 18, pp. 711-724.
- Carter CR, McKay CJ, Imrie CW Percutaneous necrosectomy and sinus tract endoscopy in the management of infected pancreatic necrosis: An initial experience. Ann. of Surg, 2000, no. 232, pp. 175-180.
- Cuschieri A. Pancreatic necrosis: pathogenesis and endoscopic management. Semin. Laparosc. Surg, 2002, Mar, no. 9, pp. 54-63.
- Hamad GG, Broderick TJ Laparoscopic pancreatic necrosectomy. J. Laparoendosc. Adv. Surg. Tech, 2000, no. 10, pp. 115-118.
- Baron TH, Thaggard WG, Morgan DE, et al. Endoscopic therapy for organized pancreatic necrosis. Gastroenterology, 1996, no. 111, pp. 755-764.
- Malkov I.S., Shaymardanov R.Sh. Ostry pancreatitis. Kazan, 2001. P. 60.
- Malkov IS et al. Patent no. 2049401 RF, 2000.
- Malkov IS et al. Patent no. 2153888 RF, 2000.
- Malkov IS, Zaynutdinov AM et al. Patent no. 2257201 RF, 2003.
Indications
Diagnostic laparoscopy at the Medicine 24/7 clinic is performed for:
- suspected internal bleeding in the abdominal cavity or pelvic area,
- ascites,
- benign or malignant neoplasms of the abdominal cavity and pelvic organs,
- jaundice of unknown cause,
- pain in the abdomen, pelvic area, when their cause is unknown,
- infertility, obstruction of the fallopian tubes,
- endometriosis,
- ectopic pregnancy or suspicion of it,
- adnexitis, oophoritis,
- uterine fibroids,
- ovarian cysts,
- pancreatitis,
- suspected appendicitis, peritonitis,
- closed abdominal injuries.
Preoperative preparation for laparoscopy for cysts and other neoplasms
- Visual diagnostics to determine the anatomical structure of the organ;
- Biochemical blood test - to identify the hormonal dependence of the tumor;
- CT scan of the pancreas – performed with 3-4 mm sections to determine the most optimal access to the organ;
- Ultrasound of the organ with targeted biopsy - performed on expert-class devices to accurately determine the sample taken;
- Tests for tumor markers - if there are indications such as suspected insulinoma (neuroendocrine tumor).
What does the doctor see during laparoscopy?
Using a visual examination with a video camera, the doctor can:
- detect the presence of fluid in the abdominal cavity and find out the cause of its accumulation,
- examine defects in the walls of hollow organs,
- detect even the smallest tumors at the initial stage of formation,
- find out the cause of fallopian tube obstruction, infertility,
- detect rupture, torsion of the ovarian cyst and other acute conditions requiring emergency intervention,
- investigate inflammatory processes in the pelvic area and abdominal cavity, differentiate them from tumor diseases.
The capabilities of visual examination in some cases significantly exceed the capabilities of ultrasound and other hardware diagnostic methods (CT, MRI).
How is the procedure performed?
Diagnostic laparoscopy at the Medicine 24/7 clinic is performed under local anesthesia in combination with sedation or general anesthesia.
When examining the abdominal cavity, a small puncture is made in the navel area, through which a cannula is inserted and carbon dioxide or nitrous oxide is injected. The gas lifts and expands the walls, filling the abdominal cavity for a better visual overview.
After this, a miniature video camera with illumination on a flexible fiber-optic cable is inserted into the abdominal cavity. With its help, the doctor examines the internal organs in detail.
If it is necessary to take samples of tumor tissue, additional punctures are made through which instruments are inserted. With their help, the doctor performs a biopsy.
As a rule, the procedure takes no more than 40 minutes. Upon completion, the gas is removed from the abdominal cavity, and a bandage is applied to the punctures.
Laparoscopy of the pelvic area for gynecological diseases is not fundamentally different from the examination of the abdominal organs.
Postoperative patient care
After completion of the operation, the patient is taken to the intensive care ward, and he is under the supervision of medical staff until his general condition stabilizes. After this, he can be transferred to the general or abdominal surgery department.
The patient's attending physician determines further treatment tactics for the patient depending on his diagnosis. After discharge, the patient is recommended to be observed and, if necessary, preventive treatment is prescribed, including diet, normalization of nutrition and lifestyle.
Preparation
Diagnostic laparoscopy is a minimally traumatic examination method. And yet, it requires short-term hospitalization in the hospital of the Medicine 24/7 clinic, where all conditions have been created to ensure that the stay is as comfortable as possible.
During laparoscopy, large incisions are not made as in open surgical interventions, however, before it is carried out, a mandatory set of examinations is performed:
- General blood analysis.
- Blood test for coagulation (coagulogram).
- Tests for HIV, syphilis, hepatitis B, C.
- General urine analysis.
- Ultrasound of the pelvis.
- ECG (electrocardiography).
- Fluorography (x-ray of the lungs).
Laparoscopy is performed on an empty stomach. For 8 - 10 hours you need to stop eating and smoking. If you are taking blood thinning medications, you should stop taking them 2 weeks before the procedure.
In 2 - 3 days you need to go on a diet, eliminate the consumption of foods that provoke gas formation (legumes, yeast bread, cabbage, raw vegetables and fruits, etc.).
If laparoscopy is scheduled for the morning, a light dinner is allowed the night before. You can't have breakfast. Before the procedure, as a rule, a cleansing enema is performed.
What diagnostic methods can be used to prescribe laparoscopy?
Before laparoscopy, the patient may be prescribed the following laboratory and instrumental diagnostic methods:
- General and biochemical blood tests;
- Ultrasound of the pancreas;
- CT and MRI;
- Angiography;
- Biopsy of pancreatic tissue.
After performing a certain set of these diagnostic procedures, the doctor makes a decision on the need to perform laparoscopic surgery and draws up a plan for further preparing the patient for the procedure.
Diagnostic laparoscopy is performed in rare cases. For example, if it is impossible to determine the location of the tumor process or the area of necrosis using ultrasound.
Contraindications
Diagnostic laparoscopy is not performed for:
- the presence of adhesions in the abdominal cavity,
- extensive blood loss and hemorrhagic shock,
- liver or kidney failure,
- decompensated conditions in cardiovascular diseases,
- acute respiratory failure,
- intestinal colic,
- bloating,
- diffuse peritonitis,
- large fibroids,
- acute infectious diseases,
- obesity 4 degrees,
- as well as in the 2nd - 3rd trimesters of pregnancy (for periods greater than 16 weeks).
The material was prepared by oncologist, chief surgeon of the Medicine 24/7 clinic, Konstantin Yuryevich Ryabov.