Entire site Library Scientific articles Consilium Medicum
Kucheryavyi Yu.A.
In the structure of morbidity of the gastrointestinal tract, chronic pancreatitis (CP) ranges from 5.1 to 9%, and in general clinical practice - from 0.2 to 0.6%. Over the past 30 years, there has been a worldwide trend towards an increase in the incidence of acute and chronic pancreatitis by more than 2 times. If in the 80s the incidence of CP was 3.5-4.0 per 100 thousand population per year, then in the last decade there has been a steady increase in the incidence of pancreatic diseases, affecting 8.2-10 people per 100 thousand annually .of the Earth's population. In Russia, a more intense increase in the incidence of CP has been noted among both adults and children. The prevalence of CP in children is 9-25 cases, in adults - 27.4-50 cases per 100 thousand population.
In developed countries, CP has become noticeably “younger”: the average age since diagnosis has decreased from 50 to 39 years, and the proportion of women among those affected has increased by 30%. primary disability of patients reaches 15%. It is believed that this trend is associated with the deterioration of the environmental situation in the region, an increase in alcohol consumption, including low quality, a decrease in the quality of food and the general standard of living. The incidence rate is constantly growing due to improved diagnostic methods and the recent emergence of new methods of imaging the pancreas with high resolution, which makes it possible to detect CP at earlier stages of disease development.
Important clinically and socially are such features of CP as a progressive course with a gradual increase in exocrine insufficiency, persistence of pain and dyspeptic syndrome, the need to follow a diet, and constant, even lifelong, intake of enzyme preparations. Chronic pancreatitis is characterized by a significant impairment of the quality of life and social status of a large number of young and middle-aged patients of the most working age. In the recurrent course of CP, early complications develop in 30% of cases (purulent-septic, bleeding from ulcerations of the mucous membrane of the gastroduodenal zone, thrombosis in the portal vein system, duodenal stenosis, etc.), with mortality reaching 5.1-11.9% . 15-20% of patients with CP die from complications associated with attacks of pancreatitis, others - due to secondary digestive disorders and infectious complications.
One of the first cases of alcoholic pancreatitis was described by Cawley in 1788, who observed a young, “carelessly living” man who died from exhaustion and diabetes. An autopsy revealed numerous stones in the pancreas.
Currently, alcoholism among the many causes of CP, according to both foreign and domestic authors, accounts for 40-80% of cases. To date, it has been established that alcohol abuse is the main cause of the development of CP in industrialized countries. There is a linear relationship between alcohol consumption and the logarithmic risk of developing CP. There was a direct correlation between the incidence of pancreatitis and alcohol consumption in men aged 20-39 years.
Content:
- Information about the disease
- Causes
- How does the disease develop?
- Types of disease
- How it manifests itself
- Establishing diagnosis
- Treatment
- Forecast
Due to regular intake of high doses of alcohol, inflammation of the pancreas often develops - alcoholic pancreatitis.
In rare cases, this diagnosis is given to people who do not suffer from alcoholism, but have a gastrointestinal disease and at some event they took strong alcohol along with fatty foods. Review the symptoms and treatment of alcoholic pancreatitis.
What are the symptoms of pancreatitis?
The most important symptom is pain; it is localized in the left hypochondrium or has a girdling character. Their intensity is related to the severity of the inflammatory process: the more pronounced the process, the stronger the pain.
Pain has several variants, which depend on the localization of the inflammatory process and the presence of concomitant diseases of the gastrointestinal tract:
- the ulcer-like variant is characterized by hunger or night pain;
- according to the type of left-sided renal colic - when the process is localized in the tail of the pancreas;
- according to the type of biliary colic (right hypochondrium syndrome) - with inflammation in the head of the pancreas;
- dyspeptic or dysmotor combined with a feeling of heaviness after eating and vomiting;
- widespread - without clear localization.
Most often, it is pain that forces patients to seek medical help. The pain is persistent, debilitating and can last for several weeks.
How does your stomach hurt with pancreatitis?
- Pain may occur 4–48 hours after the last drink.
- Not every alcohol intake can cause pain.
- Exacerbation is most often provoked by prolonged and heavy intake of alcoholic beverages (binge drinking).
- Atypical localization of pain is possible: in the right hypochondrium, in the groin, in the heart area, etc.
- Approximately 15% have no pain syndrome, and pancreatitis manifests itself with other symptoms.
What other symptoms are there?
Pancreatitis is also characterized by dyspeptic complaints:
- loosening of stool. Stool occurs 3–5 times a day, more often occurs after meals, is mushy, greasy, difficult to flush from the walls of the toilet and smelly;
- flatulence, rumbling in the stomach are caused by impaired digestion of food due to a lack of pancreatic enzymes; nausea and vomiting occur due to impaired motility of the upper gastrointestinal tract;
- weight loss. Occurs due to impaired digestion of food and absorption of nutrients due to a lack of enzymes;
- belching;
- decreased appetite;
- due to digestion disorders, hypovitaminosis develops.
An expert on the website Pokhmelye.rf, gastroenterologist Daniela Purgina, warns against a common mistake.
Don't ignore your doctor's orders. Recovery from pancreatitis can take several months, and one of the components of successful recovery is following all the recommendations of your doctor.
The highest incidence of complications occurs with pancreatitis of alcoholic etiology. Complications of pancreatitis are:
- cysts,
- pseudocysts,
- thrombosis of the splenic vein,
- exudative pleurisy,
- ascites,
- pancreatic calcification,
- pseudotumorous pancreatitis.
Alcoholic pancreatitis in 18% of cases is complicated by diabetes mellitus, which is a very dangerous disease if ignored, not following a special diet and not taking medications.
Information about the disease
Acute alcoholic pancreatitis is a dangerous disease. When it develops, the patient complains of discomfort in the upper abdomen, frequent vomiting and severe nausea, diarrhea. His body temperature may rise.
According to statistics, about half of alcoholics who are diagnosed die within twenty years. But it is important to understand that inflammation of the pancreas, the treatment of which has not received due attention, does not necessarily lead to death. Indeed, with chronic alcoholism, other internal organs also suffer greatly.
Causes
The main cause of the pathology is toxic damage to pancreatic cells from toxic metabolites of ethanol. The type and strength of the drinks used are not decisive. The pathology is equally likely to appear in a person who regularly drinks vodka and an adult who is a heavy beer drinker.
Moreover, research in the field of gastroenterology has led to the conclusion that people with a genetic predisposition to it are more likely to experience the disease. The situation is aggravated if a person smokes, eats poorly, or does not have enough protein in their diet.
How does alcohol affect the pancreas?
Strong alcohol-containing drinks have a detrimental effect on the condition of the pancreas. According to statistics, mortality from irreversible damage to the gastrointestinal tract is growing all the time. The number of deaths from drinking reaches the level of deaths from road accidents. Changes in the tissues of internal organs occur gradually over several years. With regular consumption of large doses of alcohol, pancreatitis can develop in 3-4 years; with small amounts, the period can increase to 5-7 years. But toxic shock can be caused even by one-time abuse, especially if you drink low-quality alcohol of unknown origin. Internal organ failure may occur.
The composition of strong alcohol - whiskey, vodka, rum, gin and other drinks includes pure ethanol, which is processed by the liver into acetaldehyde. This organic compound has a detrimental effect even on a completely healthy body, and with pancreatitis, the effect of alcohol on the human pancreas can manifest itself in the form of serious complications. But wine, beer, and liquor also contain ethanol, as well as a large percentage of sugar, which causes active production of insulin by the pancreas. Champagne and beer are carbonated drinks that contain carbon dioxide, which irritates the gastric mucosa and accelerates the absorption of ethanol.
How does the disease develop?
The mechanism of development and progression of acute and chronic alcoholic pancreatitis is quite complex. As a result of drinking alcohol, pancreatic cells are damaged. As a result, the iron begins to digest itself. Its tissues die - necrosis is observed. The next stage is swelling and increase in size of the organ. He begins to put increased pressure on his “neighbors.” Hence the severe abdominal pain that patients complain about. The inflammatory reaction is aggravated by the formation of pseudocysts, which contain dead tissue and liquid exudate.
Gradually, the process of fibrosis is activated in the pancreatic tissues. Dense connective tissue begins to form there. Afterwards it is transformed into stroma and ducts. Because of this, the secretion of the gland is retained and corrodes its walls even more.
All these changes contribute to the emergence of characteristic dyspeptic symptoms of alcoholic pancreatitis. Finally, normal healthy pancreatic tissue is completely replaced by connective tissue and fat. Irreversible changes occur in the activity of the endocrine system. The likelihood of developing diabetes mellitus increases.
How to diagnose pancreatitis?
X-ray examination: a survey image of the abdominal cavity can reveal the presence of calcifications in the pancreas.
Fibrogastroduodenoscopy allows you to identify indirect signs of pancreatitis:
- duodeno-gastric reflux;
- semolina symptom;
- changes in the major duodenal papilla.
Ultrasound and endoscopic ultrasound examinations can reveal the following changes:
- enlarged pancreas;
- unclear contours of the organ;
- increased echostructure of the pancreas;
- dilatation of the pancreatic duct;
- the presence of cysts in the pancreas.
Computed tomography or magnetic resonance imaging: the signs are the same as with ultrasound, only more pronounced.
Endoscopic retrograde cholangiopancreatography is the “gold standard” for diagnosing chronic pancreatitis; thanks to it, changes in the pancreatic ducts can be detected.
Laboratory research methods include:
- biochemical blood test with determination of amylase, lipase and liver enzymes;
- coprogram;
- determination of fecal elastase and urine diastase activity.
Types of disease
Doctors classify the disease into two forms - acute and chronic. The first, as a rule, occurs when a large amount of alcohol and fatty foods are taken simultaneously. It is difficult. It has been noticed that young men are more likely to experience it.
Chronic alcoholic pancreatitis is a consequence of advanced acute pancreatitis. It can also act as an independent pathology. To deal with its symptoms, you should take twenty grams of strong alcohol every day for about two years and eat poorly. But more often it is alcoholism that leads to chronic pathology.
Who develops the disease?
Alcoholics' disease - this is how the type of disorder presented in the article can be called. Its main cause is alcohol consumption. To make it clearer, it is a precursor of the disease state in 40-95%. The male gender most often falls under its influence.
Why such a significant difference? It is very difficult to find out the root cause of the disorder in patients. No one ever admits to abusing. After all, this is the same as equating yourself to the rank of “alcohol addict”.
Yes, we understand that there is nothing wrong with this. This is the same as the others, a malaise. But the reality is that our society is not aware of this issue. Refers to alcohol dependence as weakness, a sign of lower mental development. This environment is demotivating. The person cannot admit that she is in trouble. No one wants to be an outcast, not accepted...
But still... If this damage is noticed and the patient says that he “drinks a little” - this is not true. In order for the disease to develop, you need to consume drinks containing ethyl alcohol in quantities greater than the limits of doctors. And in general, it doesn’t matter what it will be - vodka or beer, whiskey or wine...
According to statistics, the timing of the formation of the disease:
- For men, 17-18 years after they started drinking regularly.
- For women – 10-12.
How it manifests itself
Usually the disease begins with the appearance of severe girdling pain. But sometimes it occurs without acute pain symptoms. Discomfortable sensations are localized in the upper abdomen and radiate to the back, under the ribs. They can be unexpected, sudden or constant.
The patient's health worsens when he sits down, leans forward, or eats food. Symptoms become very pronounced after drinking alcohol, smoking, or eating fatty foods.
The sick person feels sick and vomits. He complains of bloating, frequent belching, and loose, foul gray stools with pieces of undigested food. Since the disease disrupts metabolic processes, it becomes impossible to fully break down and absorb proteins, fats, and carbohydrates, and the patient quickly loses weight.
Establishing diagnosis
To make a correct diagnosis and select effective treatment for alcoholic pancreatitis, a comprehensive diagnosis is carried out. At the very beginning of the disease, typical ultrasound signs are absent. Characteristic changes cannot be tracked using laboratory tests. Only when the walls of the pancreas swell and begin to die can the doctor confidently confirm the presence of an inflammatory process.
When collecting a medical history, the doctor takes into account how long ago and in what quantity alcohol was taken. He can make a preliminary diagnosis based on the following signs:
elevated white blood cells;- serious changes in the leukoformula;
- high level of ESR;
- changes in enzyme activity in blood biochemistry;
- high levels of gamma-glutamyl transpeptidase;
- increased levels of glucose, albumin and transferrin in the urine;
- the presence of neutral fat, fatty acids and undigested dietary fiber in the coprogram.
If a disease is suspected, samples of intestinal juice are taken from the duodenum. This test makes it possible to examine the digestive function of the pancreas.
The patient is also required to undergo an ultrasound of the abdominal cavity. It allows you to identify whether there are cysts, dilated ducts, or calcifications. Important diagnostic techniques are CT, MRI, ERCP.
Thus, diagnosis is quite difficult. The patient must undergo a comprehensive examination, based on the results of which the gastroenterologist will be able to draw certain conclusions.
Alcoholic pancreatitis
After suffering from alcoholic pancreatitis, with abstinence from alcohol, the functions of the pancreas, as a rule, return to normal, and pancreatitis becomes chronic. But with the resumption of alcoholism, the disease worsens.
As I said above, the main factor in the development of pancreatitis is alcohol and fatty foods. Alcohol increases the tone and resistance of the sphincter, through which digestive enzymes come from the pancreas. As a result, there is difficulty in the outflow of pancreatic secretions and increased pressure in the small ducts.
It has been experimentally proven that it is alcohol that increases the pressure in the pancreatic ducts and increases the permeability of the walls of small ducts for pancreatic juice molecules.
The process goes like this:
Alcohol, entering the stomach, increases the secretion of gastric juice and the production of hydrochloric acid, which, in turn, stimulates the production of secretin (this is a protein hormone that is involved in the regulation of the secretory activity of the pancreas). This hormone causes hypersecretion of the pancreas, creating the preconditions for increased pressure in the pancreatic ducts. Thus, conditions are created for the penetration of digestive enzymes into the parenchyma and autolysis of pancreatic cells.
Alcoholic pancreatitis accounts for up to 90% of all pancreatitis.
The classification of pancreatitis is varied.
Firstly, it can be acute and chronic. The classification is further divided as follows:
Based on the nature of changes in the pancreas, the following are distinguished:
- edematous pancreatitis
- fatty pancreatic necrosis
- hemorrhagic pancreatic necrosis.
Depending on the extent of the process, focal, subtotal and total pancreatic necrosis are distinguished.
According to the clinical course, abortive is distinguished, that is, without severe clinical manifestations that resolve either spontaneously or with short therapy and a progressive course of the disease.
According to the phases of the course of severe forms of acute pancreatitis, a period of hemodynamic disturbances is distinguished - pancreatogenic shock, functional failure of internal organs and a period of purulent complications, which occurs after 10-15 days.
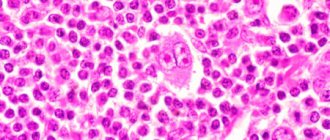
In the edematous form of pancreatitis, microscopic foci of necrosis are detected in the pancreas. Due to swelling, it increases in volume. For most people, as I said above up to 80%, the development of the pathological process stops at this stage.
With progressive pancreatitis, macroscopically noticeable fat necrosis develops. The pancreas in these cases becomes dense with multiple foci of necrosis. The cellular elements in these foci do not differentiate; leukocyte infiltration of tissues and aseptic inflammation are observed around them.
There is a dense infiltrate around the pancreas, which often involves the stomach, omentum, mesentery of the transverse colon, and retroperitoneal tissue. A cloudy serous effusion usually appears in the abdominal cavity, and sympathetic pleurisy with a small amount of serous fluid appears in the pleural cavities.
With hemorrhagic pancreatic necrosis, the pancreas is sharply enlarged, dense, with foci of hemorrhage around small vessels; due to the abundance of hemorrhages, it becomes purple-black. There is hemorrhagic effusion in the abdominal cavity. The small and large intestines are distended with gas and accumulated fluid. With such changes, the protective barrier of the intestinal mucosa is disrupted. The walls become permeable to bacteria and toxins, which leads to the development of purulent peritonitis.
Clinical symptoms of acute pancreatitis depend on the morphological form, period of development and severity of the systemic response to inflammation syndrome. In the initial period of the disease (days 1-3), both with the edematous form of pancreatitis and with progressive pancreatitis, patients complain of sharp, constant pain in the upper abdomen of a girdling nature, nausea, and repeated vomiting.
Sometimes the pain spreads throughout the abdomen. With alcoholic pancreatitis, pain occurs 12-48 hours after intoxication. In rare cases, acute pancreatitis occurs without pain, but with a pronounced systemic reaction syndrome, manifested by hypotension, severe hypoxia, tachycardia, respiratory failure, and impaired consciousness. With this course of the disease, acute pancreatitis can be diagnosed using ultrasound, computed tomography and laboratory tests.
In the early stages of the onset of the disease, objective data are very scarce, especially in the edematous form: pallor of the skin, there may be slight yellowing of the sclera. The pulse may be normal or rapid, body temperature is normal. After infection of foci of necrosis, it increases, as with any purulent process.
With severe pancreatitis, a systemic response syndrome to inflammation develops, the functions of vital organs are disrupted, respiratory failure occurs, manifested by an increase in respiratory rate, cardiovascular failure, liver and kidney failure, and signs of intestinal obstruction appear.
Most patients experience a mental disorder: agitation and confusion.
Acute alcoholic pancreatitis can be accompanied by numerous complications. The most severe of them are:
- hypovolemic shock;
- multiple organ failure, including acute renal failure, resulting from the progression of the systemic response syndrome to inflammation and the development of shock;
- pleuropulmonary complications, manifested by respiratory failure due to the development of shock lung, exudative pleurisy;
- liver failure (from mild jaundice to severe acute toxic hepatitis, developing as a result of shock and the influence of toxic enzymes and protein substances);
- abscesses of the pancreas and in the retroperitoneal tissue, the appearance of which is caused by an infection that easily develops in foci of necrosis;
- external pancreatic fistulas, which often form at the site of drainage or a postoperative wound; internal fistulas usually open into the stomach, duodenum, small and large intestine;
- widespread purulent peritonitis occurs when a pancreatic abscess ruptures into the free abdominal cavity or bacteria leak from the intestines into the free abdominal cavity;
- bleeding resulting from corrosion of blood vessels.
Treatment of pancreatitis is mandatory and immediate. In mild cases, taking conventional analgesics and antispasmodics may help. As the disease progresses, mandatory hospitalization in a hospital is necessary, where the patient needs to be monitored by a surgeon and a resuscitator, who together decide treatment issues based on the examination results.
The primary goal is to relieve pain and spasm of the sphincter in order to create a normal outflow of digestive enzymes. Symptomatic treatment and massive infusion therapy, as well as antibacterial therapy, are carried out.
One of the main tasks in the complex treatment of acute pancreatitis is inhibition of the digestive function of the pancreas. For this, complete fasting is indicated, which can last for several days.
Treatment
The pathology is treated by a gastroenterologist. The patient may also require consultations with an endocrinologist, surgeon, endoscopist, narcologist and doctors of other specialized specialties. A mandatory requirement is a complete abstinence from drinking alcoholic beverages. If the patient continues to drink, therapy will not allow him to recover.
The treatment course begins with general health measures. Sometimes the sick person has to fast for several days. In the future, you must strictly follow a special diet and stop smoking.
Replacement enzyme medications, antiemetics, analgesics, and a vitamin-mineral complex can improve the condition. Blood sugar levels are constantly monitored. If necessary, this indicator is adjusted.
In advanced cases, surgery may be required. It is aimed at opening and removing cysts, resection of the pancreas, eliminating adhesions, and closing formed fistula tracts. Surgical therapy significantly increases the risk of developing diabetes mellitus in the future.
Surgery
Endoscopic treatment is indicated for patients with obstructive forms of CP. It consists, as a rule, of endoscopic papillosphincterotomy, less often in the additional installation of a stent in the main pancreatic duct in order to more adequately drain pancreatic secretions.
Indications for surgical treatment are standard. They include: abdominal pain syndrome that cannot be relieved by other means; pancreatic cysts and abscesses, strictures or obstruction of the bile ducts, unresolved endoscopically, duodenal stenosis, splenic vein occlusion and bleeding from varices, pancreatic fistulas with the development of ascites or pleural effusion; suspected development of pancreatic cancer, not confirmed histologically (cytologically).
As described above, the inflammatory process and ductal hypertension in patients with CP can decrease as atrophy of the pancreatic parenchyma progresses, sometimes accompanied by relief of abdominal pain syndrome. This development of atrophy of the pancreatic parenchyma, accompanied by a reduction in abdominal pain syndrome, takes 10 years or more, and during this period of time the exocrine and endocrine function of the pancreas can be completely lost with the development of severe complications: diabetes mellitus and trophological insufficiency.
It is possible that timely surgical treatment aimed at relieving abdominal pain syndrome, if conservative measures are ineffective, can prevent or slow down the progression of the disease and the development of severe functional disorders. However, this method of treatment is not recognized by everyone, largely due to the fact that surgery can accelerate the development of functional disorders, especially in patients with alcoholic CP. On the other hand, the ability of the pancreas to functional regeneration was demonstrated both in experiments on animals and in patients with CP. However, even after longitudinal pancreatojejunostomy or after economical pancreaticoduodenectomy, part of the pancreatic parenchyma is lost and/or the sequence of physiological processes of the digestive transport conveyor is significantly disrupted due to postoperative modifications of the anatomy of the upper gastrointestinal tract.
The type of surgery is selected according to the established or suspected mechanism of abdominal pain. With diagnosed pancreatic hypertension and dilatation of the main pancreatic duct, it can be assumed that there is an obstruction to the outflow of pancreatic secretions and it is ductal hypertension that is the cause of pain. Therefore, preference is given to methods of surgical decompression (drainage), the use of which should lead to a reduction or relief of abdominal pain. The most commonly performed pancreaticojejunostomy according to Partington-Rochelle, in some cases with resection of the pancreas. For pancreatic cysts, cystojejunostomy or pancreatocystojejunostomy is performed.
In patients with CP with persistent abdominal pain syndrome without signs of pancreatic hypertension, options for resection operations are considered. When choosing resection operations, the surgeon must assess the severity of endo- and exocrine insufficiency of the pancreas in order to try to preserve the maximum possible volume of pancreatic parenchyma. The most commonly performed is subtotal pancreatectomy or pancreaticoduodenectomy (Whipple operation), the scope of which, in addition to pancreatic resection, includes gastric resection and duodenectomy. The main disadvantage of the technique is a significant aggravation of endocrine and exocrine pancreatic insufficiency due to the removal of a significant part of the pancreatic parenchyma. A change in the anatomy of the upper gastrointestinal tract will undoubtedly lead to secondary exocrine pancreatic insufficiency due to disruption of adequate mixing of chyme with pancreatic secretions and bile and bacterial contamination of the small intestine. In general, according to a number of studies, the effectiveness of various methods of surgical treatment in patients with painful forms of CP exceeds 70% over a five-year observation period, but the question of which method is more effective and safe has not yet been resolved.
Forecast
The prognosis, unfortunately, is unfavorable. Often the pathology leads to severe necrosis. Then the probability of death is high.
To avoid possible complications, the patient must follow all medical prescriptions and diet, and be examined annually by a gastroenterologist.
Pancreatitis is not a disease that can be ignored. If left untreated, you can die.