General information
Aerophagia is a functional disorder of the gastrointestinal tract without visible morphological changes, which manifests itself in the form of systematic repeated swallowing of large volumes of air during meals or outside meals, followed by regurgitation ( regurgitation ).
Aerophagia can be natural (physiological) - resulting from the involuntary ingestion of a mixture of gases from the surrounding atmospheric environment during drowning, poor swimming skills, during breastfeeding of small children, as well as pathological, caused by psychogenic disorders. They cause organ neurosis of the stomach . This is due to the fact that the functioning of the digestive system is closely related to the mental state of a person. One of the sections IV of the Rome Criteria, adopted in 2014 at a consensus conference in Rome entitled “Biopsychosocial model of functional digestive disorders,” demonstrated that there is a connection between the development of functional disorders and the influence of genetic factors, the environment, psychoneurological disorders and changes in physiology Gastrointestinal tract.
Diagnostics
The fact of the disease is verified based on:
- Data from the patient, where the doctor clarifies: under what circumstances the first symptoms appeared (when they swallow saliva, when rushing while eating, etc.);
- A kind of belching, when the sick person pulls his head forward, squeezes his chin to his chest and makes swallowing movements;
- Radiographs. In the image you can see a large concentration of accumulated gas in the stomach, in some cases, a transformation of the configuration of the stomach.
To find out the causes of the pathology, the following is carried out:
- ECG;
- Ultrasound of the abdominal cavity;
- Endoscopy of the esophagus, stomach and duodenum.
Sometimes a consultation with a psychiatrist is necessary.
Pathogenesis
In the development of aerophagia, an important role is played by the increased content of serotonin in restless gastroenterological patients, which leads to an increase in the air bubble in the stomach and subsequent irritation of the receptors that cause the act of belching .
Normally, swallowing small volumes of air does not cause regurgitation, but nervous belching caused by aerophagia occurs regularly, systematically and can last for a long time - several hours or even days. This process usually does not cause nausea or vomiting, because regurgitation brings relief, so many patients adapt to induce it artificially. There are cases when in women with hysterical neurosis , belching was accompanied by loud convulsive screams.
Excessive burping in people with gaseous reflux from the stomach into the esophagus and pharynx usually does not occur more often than in healthy people, it is simply that the reason for their belching lies in the air that has not reached the stomach. However, aerophagia can be constant and only occur during sleep.
Classification
Depending on the cause of occurrence, there are somatic, behavioral - caused by nutritional errors, and psychogenic forms of aerophagia - developed as a result of neurotic disorders.
Neurotic aerophagia
The pathology was assigned a code according to ICD-10 - F 45.3, it is designated as somatoform dysfunction of the autonomic nervous system, a psychogenic form of aerophagia.
The neurotic form of aerophagia is one of the clinical manifestations of neuroses. These also include IV Rome criteria: anorexia , regurgitation , gastralgia , aerophagic tics , psychogenic nausea and vomiting , diarrhea , halitosis , dysgeusia , glossodynia , intestinal crises , etc. These syndromes are the main symptoms of “gastric neurosis”.
Causes
Aerophagia, as one of the functional disorders of the stomach, can have different causes of development. Usually they become:
- neurosis, neurasthenia, hysteria and other emotional and affective disorders;
- dietary errors and unhealthy eating habits, such as overeating;
- poorly fitted dentures;
- hyperventilation syndrome;
- Rett syndrome;
- Cardiospasm is a spasm of the cardiac part of the esophagus, which makes it difficult for the food bolus to pass.
Causes of aerophagia
The causes of aerophagia are as follows:
- psychogenic factors, psycho-emotional stressful situations; in this case, aerophagia occurs as a reaction to various nervous shocks, fear, grief, etc. Often aerophagia is a manifestation of hysteria;
- respiratory tract diseases that make nasal breathing difficult;
- hasty fast eating, loud slurping while eating;
- hypersalivation (during smoking, sucking lollipops, chewing gum);
- organic or functional diseases, accompanied by a feeling of pressure and fullness in the epigastrium (for example, chronic gastritis with secretory insufficiency);
- diseases or operations that impair the function of the cardia (diaphragmatic hernia, etc.).
Symptoms of aerophagia
The entry of atmospheric air into the stomach causes unpleasant sensations of distension and discomfort in the epigastric region. The feeling of fullness and intestinal bloating may decrease to one degree or another after regurgitation - belching, as well as after a night's rest. May cause burning and hiccups.
Symptoms of neurotic aerophagia include:
- loud, repeated belching of air, which can occur after meals or regardless of it, several times a week and causes discomfort and difficulty breathing;
- pain in the heart area, reminiscent of angina pectoris ;
- a feeling of fullness, fullness, heaviness and discomfort in the epigastrium;
- As a result, the penetration of gases through the pylorus results in bloating and increased release of gases from the intestines.
Aerophagia may accompany asthma . This functional psychosomatic disorder can significantly disrupt social life - a person is uncomfortable in society and over time he becomes increasingly withdrawn and avoids people.
About the mechanisms of gas production and intestinal peristaltic activity
In healthy people, intestinal gases are mainly produced when the body processes in the large intestine:
- fructosaccharides;
- polysaccharides;
- oligosaccharides.
The processing of saccharides in the small intestine, which have short chains, provides a minimum of gases. The body removes excess gases using:
- belching;
- exhaled air;
- anus.
There is a constant circulation of methane, nitrogen, hydrogen and oxygen in the intestinal contents and bloodstream. If the small intestine does not have pathological changes, it contains no more than 20% of gases of bacterial origin. As for the large intestine, the gases that are found in it are waste products of various microorganisms.
The large intestine (namely, its proximal and ileal parts) contains chyme, which is in a liquid state. The surface of dietary fiber, in turn, is enriched with small gas bubbles. Probably, their formation would occur at high speed, but due to the fact that the intestine rhythmically contracts and its wall is under tension, this slows down the processes of gas formation.
Contractile activity of the intestines begins to increase after eating. The denser the contents become, the less intense the diffusion of gases into the bloodstream. The bubbles become larger, and the intensity of phase contractions is most pronounced in the following parts of the intestine:
- ileum (its terminal section);
- colon.
Phase contractions become pendulum-like. It is on them that the speed at which the intestinal contents move along its course, as well as the distribution of gases in the gastrointestinal tract, depends. Thanks to large propulsive contractions, the contents actively move towards the rectum, irritating the sphincters. At the same time, regulation of the flow of gases into the lower sections and their emission to the outside occurs.
It is still unknown exactly by what mechanisms peristalsis is ensured. However, it is clear that parasympathetic (or vagal) innervation plays a large role in intestinal peristaltic activity. It is controlled by local enterohormones in the form of:
- YY-peptide;
- cholecystokinin.
Researchers know the so-called “clock genes” that depend on circadian rhythms. It is thanks to them that propulsive intestinal contractions occur, the frequency of which is significantly reduced at night and increases after a person eats food.
In healthy people, the movement of gases always occurs distally, even if intestinal motility is not very pronounced. The processes of distribution of gas formations within the gastrointestinal tract regulate local reflex reactions and humoral functions. In particular, cholecystokin plays a big role here.
Often, patients, when describing the symptoms of their diseases to the doctor, talk about a subjective feeling of “bloating” in the abdomen and that it seems to be “bursting from the inside.” This is due to irritation of certain receptors responsible for stretching the stomach and intestinal walls. Their locations are mainly two layers of organ walls:
- subserous;
- muscular.
Subjective perception of unpleasant impulses from the nervous system should also be taken into account during diagnosis. The feeling of “bloating” becomes more intense when gases begin to stretch the small intestine. During examination of the patient, the abdomen does not always look swollen or enlarged in size, but sometimes this symptom can still be detected during an objective examination. In English there is a word distension, which is used to denote this sensation. Its translation sounds something like “stretching” rather than “enlargement” due to excess gas. It is due to the fact that gases are unevenly distributed throughout the gastrointestinal tract and that the tone of the abdominal muscles is impaired.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!
You can confirm a real increase in abdominal volume, as well as assess the state of gases in the intestinal tract:
- measuring abdominal circumference;
- plain radiographic examination.
There are also a number of more complex methods in the form of plethysmography, MRI, CT and xenon scintigraphy. There is also a special breathing test called hydrogen-methane. It uses saccharides to help diagnose bacterial overgrowth in the intestines. The hydrogen-methane test should be considered as a secondary test, indirectly confirming the high level of gases in the intestines.
In order to more clearly differentiate the subjective sensation of “bloating,” the 4th Rome Consensus recommends that clinicians use special illustrated manuals. In addition, questioning the doctor will help clarify the etiology of unpleasant symptoms:
- about the severity of manifestations;
- about the exact localization of sensations;
- about the connection between bloating and food intake;
- about the nature of intestinal emptying (constipation, diarrhea).
It is also necessary to take into account other pathologies, if any.
Tests and diagnostics
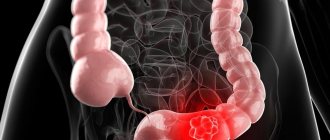
It is important to undergo a thorough examination to exclude intestinal pseudo-obstruction, GERD and malabsorption syndrome . Thanks to breath tests, it is possible to differentiate between carbohydrate metabolism disorders and bacterial overgrowth syndrome in the small intestine. X-ray studies can reveal a gas bubble in the stomach, sometimes of quite impressive size.
The gastroenterologist can also refer the patient to FGDS - fibrogastroduodenoscopy to detect inflammation of the mucous membranes or diaphragmatic hernia .
In children
Aerophagia in infants is a common phenomenon, because an unformed esophagus, large volumes of nutrition, weakness of the cardiac sphincter and the process of breastfeeding itself contribute to the swallowing or suction of excessively large portions of air. This is not a pathological process, but it can lead to frequent intestinal colic in infants. Therefore, experience and dexterity in breastfeeding and bottle feeding is very important; a young mother may be advised to follow the rules:
- postural therapy - positioning the child lying at an angle of 45-60°;
- control that the child grasps the entire nipple and the isola, and does not take breaks during feeding;
- You should not forget to hold the baby in an upright position for 10–15 minutes after feeding, allowing the air that entered the baby’s stomach during feeding to escape;
- for bottle-fed children, it is necessary to choose the right formula; it may be better to switch to NAN Comfort or Nutrilon Comfort.;
- To remove gases from the baby's intestines, you can use gas tubes or enemas, but we must not forget that they may be unsafe for premature babies and children with easily vulnerable intestinal mucosa.
Aerophagia is also characteristic of children suffering from gastroenterological diseases, hyperexcitable children, as well as mentally retarded children. This problem is quite difficult for parents to recognize on their own, so it is important to undergo an examination by a qualified specialist.
Acute dilatation and volvulus of the stomach
A special place among mechanical obstructions is occupied by acute dilatation and volvulus of the stomach.
Gastric dilatation-volvulus is a complex veterinary and surgical problem requiring emergency intervention. The disease develops very quickly and leads to damage to almost all systems and organs of the animal.
This problem occurs in dogs, regardless of size or breed, and also in cats. However, it is most typical for dogs of large breeds, and among breeds of dogs of medium and small sizes, dachshunds are most often susceptible to gastric dilatation and volvulus. A low-set chest can increase the likelihood of gastric volvulus. The likelihood of this pathology increases with age, most often animals aged 7-10 years are susceptible to it.
The cause of the disease is not fully understood. Slow gastric emptying, pyloric blockage, aerophagia can contribute to gastric dilation, and volvulus occurs as a consequence. At the same time, the reasons why the stomach can rotate around its axis are not yet clear.
Physical activity after a heavy meal, blunt trauma to the abdomen, and prolonged lying down can cause stomach dilatation in dogs.
Clinical symptoms.
As a rule, the first signs of the disease appear either during the process of eating food, or in the next few hours after that. Suddenly, the animal develops an increase in abdominal volume, which is accompanied by severe nausea, belching, vomiting, characterized by a small release of gastric contents. This type of vomiting is the first sign of gastric dilation.
If you notice these signs in your dog, take him to a veterinarian immediately. You should not feed your dog activated charcoal or laxatives.
Diagnosis.
The diagnosis of gastric dilatation-volvulus is obvious in the presence of clinical signs. If necessary, X-rays are taken. When x-rayed, the animal must stand on all fours or be supported in a similar position by the owners. X-ray allows you to differentiate gastric volvulus from its dilatation.
An additional differential diagnostic method is gastric probing. When a torsion occurs, the esophagus becomes blocked and passing the tube into the stomach becomes impossible. Probing of the stomach is carried out only after a complex of resuscitation measures.
Treatment.
If emergency resuscitation and surgical care is not provided to the animal, death may occur within 4-6 hours from the onset of the disease. Gastric volvulus is an acute surgical pathology that requires resuscitation services and surgical intervention in the first hours from the onset of the disease.
Prevention.
Large breed dogs should be fed at least twice a day and only after physical activity (after walking). You cannot feed your dog bread, rolled oats, pearl barley or easily fermented food.
You can have different attitudes towards ready-made industrial food, but the existing fact is that in dogs undergoing surgery for gastric volvulus, the presence of oatmeal is most often found in the stomach.
Bibliography:
R. Kirk, D. Bonagura “Kirk’s modern course of veterinary medicine” M. 2005
Glikman L., “Epidemiology of gastric dilatation with simultaneous volvulus in dogs”, Focus, 1997, T.1, No. 1, P.9-11
To prepare this work, materials from the sites were used
https://www.zoosite.ru
www.biblioFond.ru/vien.aspx&id=55099
Diet for aerophagia
Diet for the gastrointestinal tract
- Efficacy: therapeutic effect after 21 days
- Terms: from 3 months to permanent use
- Cost of products: 1400-1600 rubles. in Week
To prevent the development of aerophagia, you must adhere to a healthy diet and lifestyle, give preference to comfortable clothing, and also follow a few simple rules:
- You should eat food slowly, without talking and chewing thoroughly;
- do not overeat, eat in small portions;
- reduce fat intake;
- Avoid chewing gum and carbonated drinks.
In addition, the success of treating aerophagia lies in the calculation of foods and drinks, individual eating habits that provoke swallowing and regurgitation of air. These most often include sweets, coffee, fatty foods, tea with milk, some fruits, grapes, curd cheeses and sweet alcohol-containing drinks.
Causes of the symptom
There is a conditional division of these reasons into at least several categories. First of all, there are reasons that are caused by accommodative disorders of the stomach or failures of its evacuation functions. Next consider:
- aerophagia;
- carbohydrate malabsorption;
- excess intestinal bacteria;
- overeating foods containing fast carbohydrates;
- visceral sensitivity;
- peristaltic changes, as a result of which gases are unevenly distributed in the intestinal cavity;
- impaired tone in the abdominal muscles.
If the patient has impaired gastric accommodation, this may be a sign of functional dyspeptic disorders. As a result, the patient complains of bloating and a feeling of “fullness” in the upper part of the abdomen, associating the onset of symptoms with food intake. Organic diseases also have similar signs - such as stenosis of the gastric outlet as a result of a tumor or scar, intestinal obstruction, gastroparesis. They must be excluded before definitively diagnosing functional dyspepsia in a patient. Also, in case of gastric accommodation disorders, the most important differential diagnostic criteria can be:
- feeling full too early when eating;
- feeling that the stomach is full;
- epigastric pain after eating.
Aerophagia is understood as excess air that automatically enters the body when swallowed. The causes of aerophagia may lie in certain human behavioral attitudes. For example, there are people who constantly chew chewing gum, talk while eating, or eat in the wrong position (lying down or in too much of a hurry). A drinking straw can also provoke the phenomenon of aerophagia. Some anxiety disorders are sometimes accompanied by excessive swallowing.
With visceral sensitivity (hypersensitivity), the patient complains of bloating, which is often a subjective sensation. This is typical for diseases of the digestive system caused by disruptions in the connections between the brain and the gastrointestinal tract:
- functional dyspepsia, bloating or constipation;
- IBS;
- Gastroesophageal reflux disease (GERD).
Such conditions are not life-threatening, but they negatively affect the quality of life of patients. When presenting complaints, the doctor should assess their severity as carefully as possible, not excluding the presence of somatoform disorders in the patient: depression or anxiety.
With an uneven distribution of gases in the intestines (especially with IBS with constant constipation), bloating is often accompanied by its objective increase, fluctuating from 3 to 4 cm daily. The stomach begins to stretch almost immediately after eating (2nd half of the day). This phenomenon is called postprandial bloating. The main cause of discomfort in this case is areas of high intestinal muscle tone that cause resistance. In this case, the promotion of intestinal gases is due precisely to segmental, and not propulsive intestinal activity, which is responsible for the promotion of denser structures.
The results of a xenon scintigraphic study show delayed passage in the jejunum area. After eating, in patients suffering from IBS, the volume of gas in the intestines increases by about one and a half times or more. The place of accumulation of gases is mainly the distal part of the colon. It should be noted that this fact is very poorly comparable with the symptom of “bloating”.
Practical experience shows: if a patient with IBS is introduced a small amount of gases into the small intestine, he begins to experience those same sensations of “bloating” and “bloating,” while healthy people do not experience these sensations during similar experiments. The experiment showed that when a person suffering from IBS was administered 200 ml of gas, he experienced an increase in abdominal circumference by 3-4 cm. The maximum increase was in people with IBS with constipation. As for the healthy participants in the experiment, their abdomen was enlarged by no more than 2 cm. Such symptoms are due to visceral hypersensitivity, while patients with various forms of IBS demonstrated symptoms of varying intensity, for example:
- in case of IBS accompanied by diarrhea, discomfort during gas administration was very pronounced, even painful;
- a feeling of “bloating,” “bloating,” or other discomfort has been observed in virtually all forms of IBS.
The quality and type of nutrition play a big role in how and to what volume gases are distributed in the intestinal cavity. If the duodenum contains too many fats, they retain gas. In this case, the place of its localization and “delay” is the small intestine (proximal section). As a result, the stomach stretches. When a person eats too many foods containing plant fiber, peristalsis in the small intestine becomes much slower, which helps to increase the volume of its contents and, as a result, retain gases.
There is another reason that contributes to bloating. Sometimes people, due to certain factors, deliberately restrain bowel movements. As a result, the distal intestine suffers because gases are distributed unevenly in it.
With a pronounced change in the functional state of the abdominal muscles, bloating often occurs. If a person is healthy, his digestive organs enlarge due to:
- food that enters the body;
- physiological gas formation;
- secretory functions.
The tone of the peritoneal muscles is changed. This leads to the fact that the volume of the abdominal cavity increases in size. Viscero-somatic reflexes relax the diaphragm, and the rectus and oblique abdominal muscles, located closer to the skin layer, tense. The chest expands, compensating for the elevated position of the diaphragm.
MRI shows a number of pathological changes occurring in some patients suffering from functional pathologies of the gastrointestinal tract. Studies have shown that postprandial abdominal distension occurs due to:
- impaired coordination of the muscles of the abdominal wall;
- pathological (or paradoxical) relaxation of the oblique abdominal muscles;
- constant diaphragm voltage.
It is important to keep in mind that bloating can occur when patients have affected intercostal nerves. This happens after laparoscopy or surgery on the chest.
The gut microbiota can change greatly as a result of dietary patterns. Even healthy people are not immune to bloating, especially when eating ingredients rich in saccharides. It is known that their absorption and processing by intestinal enzymes occurs to a small extent, but they are very quickly processed by the microbiota. In English, there is an abbreviation FODMAPs, which refers to substances fermented by the intestines in the form of:
- oligosaccharides;
- polysaccharides;
- disaccharides;
- polyol
Bacteria ferment them less quickly, and if these substances are contained in moderate quantities in the intestines, there will be no excess gases. However, symptoms of bloating may occur if intestinal contents increase in volume (for example, bran).
A number of experiments have shown that there is a clear connection between microbiotic composition and fatty acids contained in feces with the formation of gases in IBS. Acetic and propionic acids can also cause abdominal pain, especially when they are found in high levels in foods.
To conclude this section, mention should be made of malabsorption and bacterial overgrowth in the intestinal cavity. First of all, they occur in chronic pathologies accompanied by carbohydrate malabsorption. Natural clearance in the intestines is also impaired, which is often accompanied by:
- motor impairment;
- anatomical defects (for example, “blind loops”, postoperative anastomosis after resection, etc.).
The cause of bloating can be an excess of bacteria or intense fermentation of saccharides if they enter the small intestine too quickly. An objective examination of patients shows that the abdomen is indeed swollen, and in the area of the small intestine one can feel the so-called “splashing” effect with a concomitant weakening of peristalsis. The stool may be unformed, and the symptoms of a deficiency of vitamins and other useful substances appear especially clearly.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!