Causes of blood in stool
Stool with blood visible to the naked eye is most often observed with hemorrhoids, anal fissure, colorectal cancer and colitis. It is noteworthy that the nature of rectal bleeding in each of the listed diseases has certain differences.
Haemorrhoids
Inflammatory disease of the hemorrhoidal veins of the rectum, accompanied by expansion and thrombosis of the hemorrhoids.
Bloody discharge is usually scanty, bright scarlet or bright red. In rare cases, dark-colored blood or bloody clots are observed. Distinctive feature: blood is not mixed with feces.
Other symptoms of hemorrhoids: pain, itching, a feeling of fullness in the rectum, prolapse of hemorrhoids outward.
Anal fissure
Rupture of the mucous membrane of the anal canal, most often of traumatic origin.
The pattern of bleeding resembles the symptoms of hemorrhoids: scarlet or red blood, not mixed with feces. The amount of blood is usually small, although with large cracks the blood loss can be significant.
Other symptoms of anal fissure: pain during bowel movements, quickly subsiding after bowel movement; occasionally, if the gap is inflamed, there is a feeling of fullness.
Colorectal cancer
Malignant tumor of one or more parts of the colon.
The blood may be red or distinctly black. A distinctive feature: blood is released at the beginning of the act of defecation, and not at the end, as with hemorrhoids or anal fissure. In some cases, all excreted feces may become bloody in color.
Other symptoms of colorectal cancer: the presence of a large amount of mucus or pus in the stool, a specific smell of stool, pain in the abdomen, stool disorders, a feeling of incomplete bowel movement, flatulence, constant weakness and fatigue, sudden weight loss.
Ulcerative colitis
Inflammation of the mucous membrane of the large intestine with the formation of ulcerations (wounds).
Blood is always mixed with feces, but more often in the form of subtle inclusions or bloody mucus. In the later stages of the disease, blood or bloody mucus may be released even outside of bowel movements.
Other symptoms of ulcerative colitis: frequent and liquid stools, with a foul odor, sometimes mixed with pus; frequent urge to defecate; cramping pain in the abdomen, often on the left side; constant flatulence; general weakness and severe emaciation.
Other reasons
The presence of blood in the stool can also be observed in some other diseases:
- stomach and duodenal ulcers;
- Crohn's disease;
- intestinal polyps;
- syphilitic ulcers of the rectum;
- gonorrheal proctitis, etc.
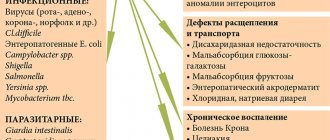
A separate group of causes of bloody impurities in the stool includes various intestinal infectious diseases of a viral, bacterial or protozoal (parasitic) nature: dysentery, salmonellosis, botulism, enterovirus, rotavirus, cytomegalovirus, amoebiasis, etc. Each intestinal infection has its own specific clinical picture, but in general terms the course of development of most intestinal infections resembles ulcerative colitis.
Intestinal bleeding
To accurately establish the fact of intestinal bleeding, it is necessary not only to consult a gastroenterologist, but also an endoscopist. To establish the severity and risk of an unfavorable outcome in case of intestinal bleeding, a clinical blood test is performed on an emergency basis (the level of hemoglobin, red blood cells, normocytes, hematocrit is determined), a stool test for occult blood, and a coagulogram. During the examination, the gastroenterologist pays attention to the pulse rate and blood pressure level. It is imperative to find out whether the patient has a history of episodes of loss of consciousness.
If there is scarlet blood in the stool, a digital examination of the rectum is performed to determine the presence of hemorrhoids and polyps. However, it should be remembered that confirming the diagnosis of hemorrhoidal dilatation of the rectal veins does not exclude intestinal bleeding from other parts of the digestive tube.
The simplest and most accessible method to identify the source of intestinal bleeding is endoscopic. To establish a diagnosis, colonoscopy (examination of the upper parts of the colon), sigmoidoscopy (visualization of the sigmoid and rectum) can be performed. An endoscopic examination allows one to identify the cause of intestinal bleeding in 90% of cases and carry out simultaneous endoscopic treatment (polypectomy, electrocoagulation of a bleeding vessel). Close attention is paid to the description of bleeding (stopped or ongoing, presence of a blood clot and its characteristics).
If bleeding continues and its source cannot be identified, mesentericography and scintigraphy of mesenteric vessels using labeled erythrocytes are performed. Mesentericography allows identifying the source of intestinal bleeding in 85% of cases, but only when its intensity is more than 0.5 ml/min. The contrast injected into the mesenteric vessels exits with the blood flow into the intestinal lumen, which is visible on an x-ray. In this case, a catheter located in the mesenteric vessels can be used to sclerosis them or administer vasopressin (it will cause vasoconstriction and stop bleeding). This method is most relevant for detecting intestinal bleeding against the background of intestinal diverticulosis and angiodysplasia.
If the intensity of intestinal bleeding is low (0.1 ml/min.), scintigraphy with labeled red blood cells will help identify its source. This technique requires some time and preparation, but with high accuracy it allows you to diagnose low-intensity intestinal bleeding. Unlike mesentericography, scintigraphy allows you to identify the source of bleeding, but not its cause.
X-ray examinations of the intestine with the introduction of a barium suspension are recommended to be carried out last, since they are the least informative and can distort the results of other methods (endoscopic and angiographic examination). Typically, assessment of the passage of contents through the intestines is carried out no earlier than 48 hours after stopping intestinal bleeding.
What to do if there is blood in the stool
There can be only one correct decision in such a situation - to immediately visit a proctologist, who will conduct an examination, prescribe the necessary laboratory or instrumental tests, after which he will make an accurate diagnosis and prescribe the appropriate treatment. Statistics show that about 60-70% of rectal bleeding is caused by hemorrhoids, which can be successfully treated with modern medicine, and therefore one should not immediately suspect cancer and delay a visit to the doctor for fear of “hearing a bad diagnosis.”
Attention: any attempts to determine the cause of stool with blood on your own (so to speak, “by symptoms”), followed by self-medication, will only lead to aggravation of the disease and a worsening of the overall clinical prognosis, and therefore the medical doctor strongly does not recommend postponing a visit to the doctor if there is stool after bowel movements. Blood began to be observed, even in the smallest quantities.
Introduction
The gastrointestinal (GI) tract originates in the mouth, travels through the esophagus, stomach, small intestine, large intestine, and ends at the anus.
Bleeding anywhere along this pathway can be acute or chronic and result from a variety of factors.
Gastrointestinal bleeding can be completely painless or cause some physical discomfort to the patient, including epigastric and diffuse abdominal pain, shortness of breath and dizziness.
Bleeding in the gastrointestinal tract in itself is not a disease, but rather a symptom of it. Bleeding of this kind can be divided into upper and lower.
- The upper gastrointestinal tract consists of the mouth, esophagus, stomach, and the first part of the small intestine, the duodenum.
- The lower part of the gastrointestinal tract includes everything else, that is, two-thirds of the small intestine, the entire large intestine, and the anus.
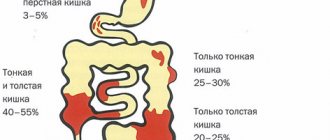
Lower gastrointestinal bleeding
Bleeding in this segment of the gastrointestinal tract can be divided into 3 categories: massive bleeding, moderate bleeding and occult (hidden) bleeding.
Massive bleeding is a potentially life-threatening condition that requires immediate blood transfusion. Occult bleeding most often occurs with colorectal cancer or mild inflammatory bowel disease.
Diverticulosis
Approximately 6 out of 10 cases of “lower” bleeding are due to diverticular disease, which includes diverticulitis of the small intestine and colon.
Constipation, lack of fiber in the diet, adolescence and the use of drugs such as aspirin and NSAIDs are risk factors for the development of diverticular disease.
The pathology is characterized by small pouches (diverticula) protruding from the intestinal wall. In general, diverticulosis is more common in older people and is thought to result from the wall of the large intestine weakening over time due to frequent constipation or excessively hard stool. Diverticulosis is usually asymptomatic, but the diverticula themselves can sometimes bleed. About 15% of people with this condition find blood in their stool. However, even in the presence of bleeding, patients do not experience pain. Also, diverticulosis in 80% of cases goes away on its own, without any treatment. It is worth noting that even in the absence of visible blood in the stool, it would not be superfluous to have stool tested to identify hidden bleeding and timely prevent anemia.
Anal fissure
An anal fissure is a small “cut” in the anus, often caused by the passage of hard and/or too large stool. It is usually characterized by sharp pain during bowel movements and bleeding. Most anal fissures disappear without any treatment, especially if the patient adjusts his diet to include fiber and a sufficient amount of clean water. However, in some cases it is still necessary to resort to drug therapy or even surgery.
Ulcerative colitis
Ulcerative colitis is an autoimmune inflammatory bowel disease characterized by chronic inflammation and ulceration of the colon mucosa. Symptoms develop gradually and can reach such an extent that they literally threaten the patient’s life.
At the moment, total colectomy is a 100% cure for ulcerative colitis. However, in the vast majority of cases, conservative treatment methods can be used.
Intestinal angioplasty
This condition is characterized by changes in the blood vessels in the colon, which become fragile, swell and break with age, leading to bleeding.
Upper gastrointestinal bleeding
Upper gastrointestinal bleeding is much more common and more likely to cause death than lower gastrointestinal bleeding.
It is important to note that mortality associated with upper GI bleeding often results from underlying medical conditions rather than from actual blood loss. The most common cause of upper gastrointestinal bleeding is peptic ulcer disease.
Peptic ulcer disease is a pathology characterized by the formation of ulcers in the stomach and/or duodenum. Risk factors include excessive drinking, abuse of nonsteroidal anti-inflammatory drugs (NSAIDs), and chronic renal failure. In many cases of peptic ulcer, Helicobacter pylori can be detected in the patient.
This bacterium is responsible for destroying the protective mechanisms in the stomach and duodenum, leading to damage to the composition of gastric juice.
Erosive esophagitis and erosive gastritis are the second most “popular” causes of bleeding in the upper gastrointestinal tract. The most common cause of inflammation of the esophagus is acid reflux.
The next cause of “upper” bleeding is esophageal varices (abnormally dilated vessels). Typically seen in patients with portal hypertension and chronic liver disease.
Tears in the esophagus (Boerhaave syndrome) can also lead to bleeding.