Gastrointestinal diseases: causes
In order of importance, we list the causes of gastrointestinal diseases in this order: 1. Poor nutrition. This is the main cause of all pathologies of our gastrointestinal tract, and this cause has the following aspects: insufficient or excessive food consumption; improper diet; improper diet; deficiency of nutrients in food; a huge amount of preservatives and various artificial substances in food; a small amount of plant fiber in food... 2. Chronic and acute stress and long-term depressive states. This cause of gastrointestinal diseases is in second place in importance, although many scientists put it in first place. 3. Smoking and alcohol abuse. These bad habits disrupt the normal microflora of the gastrointestinal tract and thereby harm the digestive processes. Among other things, nicotine and alcohol are toxins for our body and negatively affect the functionality of our immune and endocrine systems. 4. Obesity. Excess weight of a person is a consequence of a violation of his metabolic processes and “slagging” of the body, which, in turn, negatively affects the functionality of the gastrointestinal tract. 5. Unfavorable ecology. This cause of gastrointestinal diseases has recently become the most important. Disgusting ecology affects many things: the food we eat, the air we breathe, the water we drink - this contributes to the occurrence of gastrointestinal pathologies. 6. Genetic predisposition to gastrointestinal diseases. Heredity also plays a huge role, and through the mother’s side these diseases (of a chronic nature) are often passed on to children. It is for this reason, first of all, that it is extremely important for girls who are preparing to become mothers to lead a healthy lifestyle, giving up all bad habits, and remember their responsibility for the health of their future children. 7. Insufficient physical activity 8. Failure to comply with personal hygiene rules.
Gastrointestinal diseases: symptoms
Manifestations of diseases of the gastrointestinal tract are varied and depend on the location of the pathological processes. All their symptoms are in a special group and are called dyspeptic. Common symptoms of gastrointestinal disease include: - heartburn; - belching; - nausea and vomiting; - flatulence; - stool disorder; - sharp weight loss; - sudden weight gain; - lack of appetite; - huge appetite; - abdominal pain of varying localization and intensity; - general weakness... Basically, these symptoms of gastrointestinal disease do not pose a danger, but if you do not pay attention to them and do not treat them, then they are fraught with unpleasant complications in various systems of the body. It is for this reason that diagnosis of the gastrointestinal tract is of great importance: identifying the disease at an early stage of its development is a guarantee of successful therapy.
What's happening?
From the mouth, microbes enter the stomach, and then into the intestines, where they begin to multiply intensively. After microbes enter the body, an asymptomatic incubation period begins, lasting, in most cases, 6-48 hours.
Symptoms of the disease are caused by both the microbes themselves and the toxins they produce. Intestinal infections can occur in the form of acute gastritis (with vomiting and pain in the pit of the stomach), enteritis (with diarrhea), gastroenteritis (with vomiting and diarrhea), colitis (with blood in the excrement and stool disorders), enterocolitis (with damage to the entire intestine).
One of the most unpleasant consequences that occurs with intestinal infections is dehydration due to vomiting and/or diarrhea. These diseases are especially severe in early childhood and in older people. Severe dehydration can result in kidney failure and other serious complications, in particular dehydration shock (associated with fluid loss).
Gastrointestinal diseases: diagnosis
Diagnosis of pathologies of the gastrointestinal tract begins with collecting an anamnesis - interviewing the patient. The patient informs the doctor about his life: his regime and diet, the presence of any diseases (particular attention is paid to chronic ones), about the problems that bother him and about his symptoms. If there is a suspicion of gastrointestinal disease, modern gastroenterology uses instrumental diagnostic methods: - Ultrasound (ultrasound examinations); — pH-metry (intragastric); — manometry of the gastrointestinal tract; — endoscopy of the gastrointestinal tract; — electrogastroenterography; - biopsy; - radiology diagnostics...
Diagnosis and treatment
It is very important to distinguish an intestinal infection from other diseases with similar symptoms: non-bacterial food poisoning (for example, drugs), acute appendicitis, myocardial infarction, pneumonia, ectopic pregnancy, etc.
If symptoms resembling an acute intestinal infection appear, you should contact an infectious disease specialist. In order to make a correct diagnosis, the doctor will prescribe a bacteriological examination of stool or vomit. Additionally, serological diagnostic methods can be used (to detect antibodies to infectious agents).
If the patient’s condition quickly deteriorates, immediately call an ambulance, and before it arrives, provide first aid to the victim.
Treatment of intestinal infections is complex and includes: combating microbial poisons, the microbes themselves, as well as dehydration. In addition, patients must follow a proper diet and, with the help of special medications, restore normal intestinal microflora.
Treatment of gastrointestinal diseases
The main methods of treating gastrointestinal diseases: - drug therapy; — diet therapy; — physiotherapy; - surgical intervention; - therapeutic therapy. Perhaps the most effective method of treating gastrointestinal diseases is complex therapy of pathologies using probiotic and prebiotic drugs with the immunomodulator Transfer Factor (TF). Diseases of the gastrointestinal tract, as a rule, are a consequence of a violation of its beneficial microflora, which leads to the predominance of pathogenic and opportunistic microorganisms, which, in turn, cause various diseases of the gastrointestinal tract, and then the immune, endocrine, nervous, cardiovascular and others body systems. Probiotics with prebiotics with the immunomodulator TF restore the normal flora of the gastrointestinal tract. Here are the most effective of these drugs: - Unibacter; — Santa Rus-B; — Vetom (its entire line); — Lactis; — Inulin (prebiotic); - Acidophilus...
Transfer factor is an immunomodulator, which is based on molecules of the same name - components of our immune system. Once in the body, this drug: - restores immunity and the normal course of metabolic processes in the body; — enhances the therapeutic effect of the drugs used, helping to normalize the microflora of the gastrointestinal tract; — neutralizes possible side effects from the therapy used (no matter what). It remains to be said that the listed drugs for the treatment of gastrointestinal diseases have no contraindications, do not cause any side effects, are not addictive and overdose is impossible, these are 100% natural drugs that we recommend using not only in the complex treatment of gastrointestinal pathologies, but and for their prevention.
Intestinal infection
Acute intestinal infection
Intestinal infections are one of the most common diseases in the world. Their prevalence among the population is extremely high, both in the children's age group and in adults. When we talk about intestinal infection, we mean acute intestinal disease.
Acute intestinal infections (AI) are a group of acute human infectious diseases caused by various infectious agents (mainly bacteria), with a nutritional mechanism of infection, manifested by fever and intestinal syndrome with the possible development of dehydration and severe course in children and the elderly.
The incidence of intestinal infections in the world, and in particular in Russia, is quite high. Every year more than 500 million people get sick on the planet. The incidence rate in Russia reaches 400 or more cases per 100 thousand population. The structure of childhood morbidity and mortality suggests that acute intestinal diseases are in third place.
Causes of intestinal infections
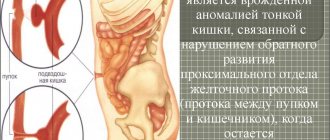
The digestive tract consists of the oral cavity, pharynx, esophagus, stomach, small intestine (including the duodenum, jejunum, ileum), and large intestine. In the saliva of the oral cavity there is a substance - lysozyme, which has a bacteriostatic effect. This is the first protective barrier. The mucous membrane of the stomach has glands that produce gastric juice (consisting of hydrochloric acid and pepsin). Hydrochloric acid is the second barrier for pathogenic microorganisms that can die in it (however, this does not always happen). The mucous membrane of the small intestine is covered with numerous villi that participate in parietal digestion and perform protective and transport functions. In addition, the intestinal mucosa contains secretory immunoglobulin - IgA, which plays a role in the immunity of the human body.
The microflora inhabiting the intestines is divided into obligate (mandatory for presence in the intestines), which includes bifidobacteria, lactobacilli, E. coli, bacteroides, fusobacteria, peptococci. Obligate flora makes up 95-98% of all representatives. The function of obligate flora is protective due to competitive presence and participation in digestive processes. Another group of microorganisms inhabiting the intestines is called facultative (additional) flora, which includes staphylococci, fungi, opportunistic microorganisms (Klebsiella, streptococci, Proteus, Pseudomonas aeruginosa, clostridia and others). Additional flora can also participate in the digestion process through the production of certain enzymes, however, opportunistic flora with a certain growth can cause the development of intestinal syndrome. All other flora that enters from the outside is called pathogenic and causes an acute intestinal infection.
What pathogens can cause acute intestinal infection?
There are several types of intestinal infections depending on the etiology:
- Intestinal bacterial infection: salmonellosis (Salmonellae enteritidis et spp.), dysentery (Shigellae sonnae et spp.), yersiniosis (Iersiniae spp.), escherichiosis (Esherihiae coli enteroinvasive strains), campylobacteriosis (enteritis caused by Campylobacter), acute intestinal infection caused by Pseudomonas aeruginosa (Pseudomonas aeruginosa), clostridia (Clostridium), Klebsiellae (Klebsiellae), Proteus spp., staphylococcal food poisoning (Staphilococcus spp.), typhoid fever (Salmonellae typhi), cholera (Vibrio cholerae), botulism (botulinum toxin poisoning ) and others.
- NCI of viral etiology (rotaviruses, Norfolk group viruses, enteroviruses, coronaviruses, adenoviruses, reoviruses).
- Fungal intestinal infections (usually fungi of the genus Candida).
- Protozoal intestinal infections (giardiasis, amoebiasis).
Causes of intestinal infections
The source of infection is a patient with a clinically pronounced or erased form of intestinal infection, as well as a carrier. The contagious period is from the moment the first symptoms of the disease appear and the entire period of symptoms, and for a viral infection - up to 2 weeks after recovery. Patients release pathogens into the environment with feces, vomit, and less often with urine.
The mechanism of infection is nutritional (that is, through the mouth). The routes of infection are fecal-oral (food or water), household, and for some viral infections - airborne. Most pathogens of acute intestinal infection are highly resistant in the external environment and retain their pathogenic properties well in the cold (in the refrigerator, for example). Transmission factors are food products (water, milk, eggs, cakes, meat, depending on the type of intestinal infection), household items (dishes, towels, dirty hands, toys, door handles), swimming in open water. The main role in the spread of infection is given to compliance or non-compliance with personal hygiene standards (washing hands after using the toilet, caring for the sick, before eating, disinfecting household items, allocating personal utensils and towels to the sick person, reducing contact to a minimum). Susceptibility to intestinal infections is universal, regardless of age and gender. The most susceptible to intestinal pathogens are children and the elderly, people with diseases of the stomach and intestines, and people suffering from alcoholism.
Factors predisposing to the development of intestinal infection in children: bottle-fed children, premature babies; violation of the rules for introducing complementary foods without the necessary heat treatment; warm season (usually summer); various types of immunodeficiencies in children; pathology of the nervous system in the perinatal period.
Immunity after an infection is unstable and strictly type-specific.
General symptoms of acute intestinal infections
The incubation period (from the moment the pathogen enters until the first signs of the disease appear) lasts from 6 hours to 2 days, rarely longer. Almost any intestinal infection is characterized by the development of 2 main syndromes, but to varying degrees of severity:
- Infectious-toxic syndrome (ITS), which is manifested by a temperature ranging from subfebrile numbers (37º and above) to febrile fever (38º and above). In some infections there is no temperature at all (for example, cholera), and the absence of temperature or a slight short-term rise is typical for food poisoning (staphylococcal, for example). Fever may be accompanied by symptoms of intoxication (weakness, dizziness, body aches, nausea, and sometimes vomiting due to high fever). Often, an infectious-toxic syndrome is the beginning of an acute intestinal infection, lasting until the appearance of the second syndrome from several hours to a day, rarely longer.
- Intestinal syndrome. Manifestations of intestinal syndrome may be different, but there are similarities in symptoms. This syndrome can manifest itself as a syndrome of gastritis, gastroenteritis, enteritis, gastroenterocolitis, enterocolitis, colitis.
Gastritis syndrome is characterized by the appearance of pain in the stomach (epigastric region), constant nausea, vomiting after eating and drinking water, and even a sip of liquid can cause it. Vomiting can be repeated, bringing short-term relief. It is possible to liquefy the stool over a short period of time, sometimes once.
Gastroenteritis syndrome is accompanied by abdominal pain in the stomach and umbilical region, vomiting, and the appearance of frequent stools, first mushy in nature, and then with a watery component. Depending on the cause of the occurrence, the color of the stool may change (greenish with salmonellosis, light brown with escherichiosis, for example), as well as mucus and undigested food debris may appear.
Enteritis syndrome is characterized by the appearance of only stool disorders in the form of frequent watery stools. The frequency depends on the type of pathogen and the degree of its infectious dose reaching a particular patient.
Gastroenterocolitis syndrome is manifested by vomiting and frequent loose stools, abdominal pain becomes widespread and almost constant, bowel movements become painful and do not bring relief, and there is often blood and mucus in the stool. Some acts of defecation with scanty mucous discharge.
Enterocolitis syndrome is characterized only by severe pain along the entire perimeter of the abdomen, frequent stool mixed with scanty discharge.
Colitis syndrome is manifested by fights in the lower abdomen, mainly on the left, acts of defecation are painful, the contents are scanty with an admixture of mucus and blood, false urge to stool, lack of relief at the end of defecation.
Syndromes such as gastroenteritis, gastroenterocolitis and enterocolitis are characteristic of salmonellosis, enterocolitis and colitis are characteristic of dysentery, escherichiosis is accompanied by the development of gastroenteritis, enteritis is the leading syndrome of cholera, gastritis syndrome can accompany food poisoning, but it can also be gastroenteritis, viral intestinal infections occur more often in form of gastroenteritis.
Features of acute intestinal infection in children
- more severe course of acute intestinal infection,
- rapid development of symptoms of dehydration,
- a higher proportion of viral intestinal damage than in the adult age group.
When an acute intestinal infection occurs, a child quickly develops dehydration and desalination of the body, resulting in high mortality; In addition, even opportunistic microorganisms are characterized by the ability to cause a severe process in the intestines of children.
Complications of acute intestinal infections
- Dehydration (dehydration) is a pathological loss of water and salts in an unnatural way (vomiting, loose stools). There are 4 degrees of dehydration in adults: - 1 degree (compensated) - loss of body weight up to 3% of the original; 2nd degree (transitional) – loss of body weight 4-6% of the original; 3rd degree (subcompensated) – 7-9% of the original; 4th degree (decompensated) – more than 10% loss of body weight from the initial one. In children, grade 3: 1 degree (weight loss up to 5% of the original), 2 degree (6-9%), 3 degree (algid) - more than 10% loss of body weight from the original. In addition to weight loss, concerns about dry skin and mucous membranes, thirst, decreased skin elasticity, and hemodynamic disturbances (increased heart rate, decreased blood pressure). Thirst does not always happen: if there is a salt-deficient type of dehydration (this happens more often with repeated vomiting), then there may not be thirst. If the water deficiency type of dehydration is present, then thirst is the main symptom.
- One of the manifestations of fulminant dehydration: dehydration shock with a possible fatal outcome. There is severe dehydration and hemodynamic disorders (critical drop in blood pressure).
- Infectious-toxic shock : occurs against a background of high temperature, often at the onset of the disease and is accompanied by high toxinemia (high concentration of bacterial toxins in the blood), serious hemodynamic disturbances and possible death.
- Pneumonia (pneumonia).
- Acute renal failure.
Differential diagnosis (non-infectious “masks” of intestinal infections)
At the stage of making a preliminary diagnosis of an acute intestinal infection, the doctor has to differentiate the intestinal infection from other conditions and diseases, the symptoms of which may also include vomiting and diarrhea (loose stools). An important role is played by a correctly collected medical history (medical history), in which it is necessary to describe in as much detail as possible the symptoms and the timing of their onset, the severity of complaints and their duration.
Gastroenteritis syndrome can accompany poisoning with mushrooms, heavy metal salts, and fish and shellfish poisons. Unlike infectious diarrhea, with the above poisonings there will be no ITS (infectious toxic syndrome) - neither fever nor symptoms of intoxication.
The syndrome of enterocolitis or colitis (with blood in the stool) occurs with UC (nonspecific ulcerative colitis), intestinal neoplasms, Crohn's disease, diverticular disease and others. Each of these conditions has other specific symptoms that characterize the disease. In particular, with Crohn's disease, diarrhea will be chronic, prolonged, cramping abdominal pain, weight loss, anemia. With UC - prolonged low-grade fever, prolonged diarrhea with blood, weight loss, pain in the lower left abdominal region, and others.
Most often, a practitioner must differentiate an acute intestinal infection from mushroom poisoning, ulcerative colitis, acute appendicitis, rectal cancer, thrombosis of mesenteric vessels, and acute intestinal obstruction.
If there is significant abdominal pain, especially in children, the first step should be to visit an emergency surgeon to rule out surgical pathology.
It is no secret that the appearance of frequent loose stools for most people is not a reason to see a doctor. Most try to use various drugs and methods to stop diarrhea and restore impaired health. At the same time, a simple (as it seems at first glance) intestinal infection can turn into a serious problem with long-term disability.
Symptoms that require you to see a doctor immediately:
- early childhood (up to 3 years) and preschool age of the child;
- elderly people (over 65 years old);
- frequent loose stools more than 5 times a day in an adult;
- repeated vomiting;
- high fever with diarrhea and vomiting;
- blood in stool;
- cramping abdominal pain of any localization;
- severe weakness and thirst;
- the presence of chronic concomitant diseases.
What absolutely cannot be done if you suspect an acute intestinal infection: If frequent loose stools appear, accompanied by abdominal pain and fever, then:
- Painkillers should not be used. In the case of hidden symptoms of any surgical pathology (cholecystitis, appendicitis, intestinal obstruction and others), pain relief can complicate the diagnosis and delay the provision of timely specialized care.
- You cannot independently use fixing agents (astringents) - such as immodium or loperamide, lopedium and others. In acute intestinal infection, the bulk of pathogen toxins are concentrated in the intestines, and the use of such drugs contributes to their accumulation, which will aggravate the patient’s condition. The course of intestinal infection will be favorable with timely emptying of intestinal contents along with pathogen toxins.
- You cannot do enemas yourself, especially with hot water.
- You cannot use heating procedures on the abdomen (a heating pad with hot water, for example), which certainly increases the inflammatory process, which will aggravate the patient’s condition.
- If you have symptoms of an acute intestinal infection and suspect a surgical pathology, you should not hesitate and try to treat with improvised means (folk, homeopathic and others). The consequences of delaying seeking medical help can be very serious.
Laboratory diagnosis of acute intestinal infection
A preliminary diagnosis is made after a clinical and epidemiological examination, which includes contact with the patient, possible cases of intestinal infection among the immediate environment, consumption of poor quality products, products without water treatment and heat treatment, failure to comply with personal hygiene rules, as well as symptoms of the disease ( the onset of the disease, the main symptoms characteristic of a particular infection).
Already at this stage, an unmistakable diagnosis is possible (for example, in the case of the outbreak nature of the disease and the presence of similar patients in the infectious diseases clinic, in the presence of specific symptoms - blood in the stool, false urge to stool, temperature during dysentery, for example; copious watery stools without odor or impurities , without fever - with cholera), due to which in some cases, after collecting all materials for laboratory testing, specific treatment is prescribed already at the stage of preliminary diagnosis.
An experienced doctor, in the presence of obvious symptoms, may suspect a certain intestinal infection and prescribe adequate treatment.
The final diagnosis is made after laboratory confirmation:
- Bacteriological methods (seeding materials for research on special media and growing bacterial colonies). Materials can be feces, vomit, gastric lavage, food debris, water samples. Preliminary sowing and the result can be issued on the 2nd-3rd day.
- Serological methods (detection of specific antibodies in the blood) ELISA, RNGA - paired blood sera are necessarily taken with an interval of 10-14 days.
- PCR diagnostics in biological fluids (for example, L-form salmonella). The result is issued on the same day.
Instrumental diagnostic methods: sigmoidoscopy, colonoscopy, irigoscopy.
Treatment for acute intestinal infection 1. Organizational and routine measures. All young children with any severity of intestinal infection are subject to hospitalization due to the risk of rapid development of dehydration syndrome. Adults are hospitalized for moderate and severe forms of acute intestinal infection, as well as when it is impossible to isolate the patient (living in small families with a shared toilet, dormitories, closed organized institutions - orphanages, etc.). For the entire period of fever, bed rest, then semi-bed rest until the loose stools stop. Diet therapy (table No. 4 according to Pevzder). In the acute period of the disease - slimy soups, weak meat broths, pureed lean meat, boiled lean fish, scrambled eggs, cereals, white stale bread and crackers, dry uneaten cookies, baked apples without peel. Excluded: milk, seasonings, spices, smoked meats, canned food, garlic, green onions, radishes, alcohol. They are transferred to the general table carefully and gradually over 3-4 weeks. Products such as milk and refractory fats are poorly digested for another 3 months.
2. Drug treatment of acute intestinal infection.
- Rehydration therapy (replenishment of fluid losses and detoxification of the body). It is carried out for any acute intestinal infection in 2 stages: elimination of symptoms of dehydration at the moment,
- replenishing ongoing losses.
You can take the liquid orally (drinking regimen in the absence of vomiting and the urge to do so), as well as parenterally (intravenous infusions of solutions). How to calculate the volume of oral rehydration at home with 1 degree of dehydration and outpatient treatment: this is 30 ml/kg of body weight per day in an adult, and 30-50 ml/kg/day in children. You need to drink the liquid in small portions every 5-10-15 minutes, warm. These are solutions of rehydron, citroglucosolan, enterodez. Intravenous rehydration is carried out only in a hospital setting under strict control of water-salt metabolism indicators.
- Antidiarrheal drugs: enterosorbents (polyphepam, white coal, Filtrum, Laktofiltrum, Enterosgel and others), smecta, bactisubtil, Helac-Forte,
Rehydration therapy should be carried out at the first symptoms of an intestinal infection, and treatment with enterosorbents should also be started at the first symptoms.
Intestinal antiseptics and antibacterial agents will not help with a viral infection, but they can be prescribed by a doctor until a definitive diagnosis is confirmed or to prevent a secondary bacterial infection. On the third day of treatment with antibacterial agents, be sure to start taking probiotics to restore intestinal microflora. Prognosis of acute intestinal infection
The outcomes can be both favorable (recovery) and unfavorable (formation of chronic forms, carriage). In the children's age group, in 25% of cases, the outcome of intestinal infection can be the formation of gastrointestinal tract pathology in the form of pancreatic dysfunction, biliary tract disorders, intestinal dysbiosis, and functional dyspepsia.
Prevention of acute intestinal infection comes down to the following measures:
- compliance with personal hygiene rules;
- drinking boiled or bottled water;
- washing vegetables and fruits before consumption with running water, and for small children - with boiled water;
- thorough heat treatment of necessary food before consumption;
- short-term storage of perishable foods in the refrigerator;
- do not accumulate garbage;
- monitor the cleanliness of the home and sanitary maintenance of the toilet room and bathroom.
Prevention of gastrointestinal diseases
1. Eat right. This point in the prevention of gastrointestinal diseases includes adherence to the diet and regimen. Eat more often, but eat in small quantities. Eat 5-6 times a day, but don't overeat. Limit your consumption of fried, smoked, fatty and salty foods. Increase your fiber intake (vegetables, fruits, cereals, bran bread). 2. Control your weight. Calculate your body mass index and stick to it, fight obesity, lose excess weight, but do it correctly (!!!). 3. Minimize your alcohol consumption. And if you have a gastrointestinal disease, give it up (and urgently). 4. Quit smoking. 5. Avoid stressful situations. Review your life and understand one thing: there is nothing more valuable for you and your loved ones than your health in this life, and no problems are worth your nervous costs. 6. Lead an active lifestyle. Gastrointestinal diseases are caused by low physical activity of a person (including). And to prevent these diseases, do exercises in the morning, jogging in the evenings, and if you have a “sedentary” job, try to do warm-up exercises for 5-10 minutes after an hour or two. 7. Take probiotic and prebiotic supplements on a regular basis. Our gastrointestinal tract needs a constant supply of beneficial microorganisms.