Causes of intestinal obstruction
The causes of intestinal obstruction can be mechanical or non-mechanical.
Mechanical reason
- These are physical barriers that prevent or limit the passage of contents through the intestinal tract. These include:
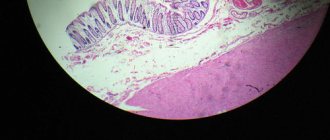
- adhesions or tissues (the structure of tissues of living organisms is studied by the science of histology)
that can develop after abdominal and pelvic operations; - foreign object if swallowed;
- gallstones;
- contagious disease;
- inflammatory diseases (disorders of normal functioning, performance)
of the intestine; - intussusception, when a sector of the intestine is pressed into the next sector, causing its crisis;
- meconium plug, which is the first stool encountered in newborns;
- tumors (Tumor (syn. neoplasm, neoplasia, neoplasm) is a pathological process represented by newly formed tissue)
; - intussusception (one segment of the intestine penetrates into the lumen of another);
Non-mechanical obstacles
- this is when the digestive system is disrupted. The narrow and large intestinal tracts contract (peristalsis) in concert. If something interrupts this process, a non-mechanical obstruction may appear.
The causes of non-mechanical intestinal obstructions include:
- abdominal or pelvic surgery;
- electrolyte imbalance;
- Hirschsprung's disease is a condition where nerve (related to bundles of nerves)
are absent at the end of the intestine; - infections (The term means various types of interaction of foreign microorganisms with the human body)
; - certain nerve (related to bundles of nerves)
and muscle disorders, such as Parkinson's disease; - opioid drugs.
Volvulus of the small intestine
Under normal conditions, the intestinal loops make significant movements and often make turns of up to 90° without causing any pathological disorders. When the intestine is rotated more than 180°, its lumen is blocked and the mesenteric vessels are compressed. Volvulus is promoted by intestinal overflow, increased peristalsis, and adhesions. Volvulus may involve several loops, and sometimes the entire intestine.
Clinical picture and diagnosis . Volvulus of the small intestine begins acutely. The disease occurs with severe general and local clinical symptoms characteristic of acute high strangulation obstruction.
In the first hours of the disease, against the background of constant pain, cramping pain periodically occurs, the intensity of which increases synchronously with peristalsis, reaching the character of unbearable. Often patients become restless, scream in pain, and take a forced position with their legs brought to their stomach. From the very beginning of the disease, repeated vomiting occurs, which does not bring relief, initially with unchanged gastric contents and bile, and then it becomes fecaloid. Retention of stool and gases is an unstable symptom of the disease: often at first there is a single stool due to emptying of the lower intestines, which does not bring relief.
The general condition of the patient is serious. Disorders of water-salt, protein and carbohydrate metabolism, microcirculatory and hemodynamic disorders, intoxication, and decreased diuresis quickly appear and increase. The abdomen is moderately swollen, sometimes the swelling is manifested only by smoothness of the subcostal areas.
A positive sign of Will is often detected - a balloon-shaped loop of jejunum stretched and fixed in the abdomen, over which a high tympanitis and splashing noise are detected.
During a survey fluoroscopy of the abdomen, Kloiber's cups are detected, which appear 1-2 hours after the onset of the disease and are localized in the left half of the epigastric region and in the mesogastric region.
Treatment is surgical. It involves detorsion or “untying” the nodule, removing intestinal contents through a long nasointestinal tube. If the viability of the intestines is beyond doubt, detorsion is limited. In case of intestinal necrosis, the non-viable loop is resected with end-to-end anastomosis. The line of intersection of the intestine should be 40-60 cm above the obstacle and 10-15 cm below it.
Causes of risk of intestinal obstruction
Certain conditions and diseases (disturbances in normal functioning, performance)
increase the risk of developing intestinal obstruction. If a person's intestinal tract is not properly developed, it is most susceptible to obstruction. Other reasons for the risk of developing digestive obstruction include:
- cancer, especially in the abdominal cavity;
- Crohn's disease or other diseases (disorders of normal functioning, performance)
of the intestine, which can cause thickening of the intestinal walls; - previous surgery on the abdominal cavity or pelvis, which increases the risk of adhesions.
Diagnostics
Diagnosis of intestinal obstruction is a comprehensive examination of the patient, which includes the following activities:
- examination - palpation of the abdomen, determination of skin color, monitoring of body temperature and blood pressure;
- X-ray of the large intestine - if there is a suspicion of an intermediate or late stage, the study is carried out immediately;
- blood test - general and biochemical;
- Ultrasound or CT scan of the abdominal cavity are methods that allow one to visualize the possible cause of obstruction.
In some cases, there are indications for laparoscopy. Most often, this measure is resorted to when external signs confirm the diagnosis, and the critical condition of the patient does not allow a full diagnosis. With laparoscopy, the doctor not only identifies the pathological area of the intestine, but can also immediately begin treatment.
If the patient is delivered at an early stage of the disease and the listed methods do not make it possible to establish a diagnosis, contrast radiography of the passage of barium through the intestines is indicated, with viewing every two hours. Until the circumstances are fully clarified, the patient remains in the hospital.
When to see a doctor
Vomiting (reflex eruption of stomach contents)
and diarrhea are early signs of intestinal obstruction. If a fever develops after these symptoms, you should urgently seek medical help.
For severe pain (an experience associated with actual or potential tissue damage)
in the tummy, you should immediately consult a doctor.
Intestinal obstruction can have severe consequences. It is especially important to consult a doctor if symptoms (Symptom from Greek - case, coincidence, sign - one separate sign, frequent manifestation of any disease, pathological condition or disorder of any vital process)
appear after surgery.
Types and reasons
Intestinal obstruction is divided into the following types:
- dynamic,
- mechanical,
- vascular.
The type is determined by the cause that caused this pathological condition.
Causes of dynamic obstruction:
- constant spasm of the intestinal muscles, which can occur with painful irritation of the intestines by worms, with acute pancreatitis, with traumatic injuries from foreign bodies;
- paralysis of the intestinal muscles, which develops during surgical interventions, poisoning with morphine-containing drugs, salts of heavy metals, as a result of food infections.
In case of mechanical obstruction, there must be some kind of obstacle:
- fecal stones, stones from the biliary tract, foreign body, compression of the intestinal lumen from the outside by tumor formations and cystic formations of other organs, intestinal tumors growing into the lumen;
- volvulus of intestinal loops as a result of intestinal strangulation at the gates of abdominal hernias, adhesions and cicatricial processes, a knot of intestinal loops.
Vascular obstruction is always facilitated by disturbances in the blood supply (thrombosis, embolism) of the mesenteric blood vessels.
Intestinal obstruction - healing
Healing a bowel obstruction depends on the background and severity of the blockage. Complete mechanical obstruction usually requires surgical intervention.
Ways to heal digestive obstruction:
Medicinal healing
. Opioids can cause constipation. If this happens, laxatives will help.
Observation
. The obstruction may need to be monitored for several days and often resolves over time. During this time, you still need to limit food and drink. Doctors may give fluids intravenously to prevent dehydration.
Nasogastric tube.
This is a narrow tube that is inserted through the nose into the stomach.
It removes liquid and gas trapped in the stomach, relieving pressure. This simplifies pain (physical or emotional suffering, painful or unpleasant sensation)
and vomiting
(Vomiting is a reflex eruption of the contents of the stomach and sometimes the duodenum through the mouth, sometimes through the nose)
.
Operation
. Doctors can remove blocked or distorted parts of the intestine. In some cases, stricture plastic surgery may be required, when the surgeon widens the narrowed section of the intestine.
Therapeutic enema
. The nurse or doctor will inject drugs or water into the intestinal tract to induce bowel movements for severe constipation.
Use medications that can reduce discomfort:
- anti-nausea medications to prevent vomiting (Vomiting is a reflex eruption of the contents of the stomach and sometimes the duodenum through the mouth, sometimes through the nose)
; - painkillers;
- medicines to fight bacterial infections.
First aid for intestinal obstruction
Intestinal obstruction is a condition that requires surgical intervention. Drug therapy is completely ineffective. Therefore, if you suspect this condition, you should immediately seek medical help.
Before the ambulance team arrives, the patient must be laid on a flat, horizontal surface, ensuring complete rest as much as possible.
It is strictly forbidden to induce stool using laxatives - the desired effect will not be achieved, and by increasing the frequency of contractions of the intestinal walls, the patient's condition will worsen.
You can give cool drinks in small doses. It is important to monitor body temperature, blood pressure, and pulse. This information will facilitate and speed up diagnosis by specialists.
If the patient is in serious condition, the ambulance paramedic can carry out initial therapy, including injections of drugs to relieve spasms and infusions with a plasma replacement solution. In case of severe and painful vomiting, a special probe is installed to facilitate the passage of vomit.
Intestinal blockage with fecal stones
Blockage of fecal “stones” occurs mainly in the large intestine. This type of obstruction is observed in elderly people suffering from chronic colitis and prolonged constipation. Predisposing factors are often developmental anomalies (megacolon, megasigma, congenital mucosal membranes, etc.).
Clinical picture and diagnosis. Fecal stones may pass out on their own in the stool. In some cases, they lead to the development of bedsores of the intestinal wall and fecal peritonitis. Stones can cause acute obstruction of the colon, the symptoms and clinical course of which are characteristic of low intestinal obstruction: cramping pain, retention of stool and gases, increased, long-lasting peristalsis, sudden swelling of the colon, taking the form of an inflated car tire, an empty, balloon-shaped ampulla of the rectum intestines.
Treatment. For obturation with fecal stones, surgery is indicated in those rare cases when conservative treatment methods (siphon and oil enemas, attempts at digital or endoscopic crushing and removal of stones through the rectum) do not produce an effect.
Surgical treatment consists of colotomy, removal of stones and temporary colostomy.
Acute strangulation intestinal obstruction, clinical picture, diagnosis, treatment.
Strangulated intestinal obstruction is a separate type of intestinal obstruction, when, in addition to compression of the intestinal lumen, compression of the vessels and nerves of the mesentery occurs, which quickly leads to impaired circulation in the intestine and can cause necrosis of a section of the intestine.
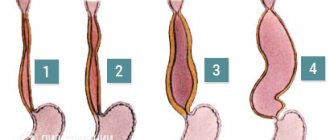
There are three types of strangulation intestinal obstruction: volvulus, nodulation and pinching.
Volvulus is observed in those parts of the intestine where there is a mesentery. Its appearance is promoted by scars and adhesions in the abdominal cavity, a long mesentery of the intestine, fasting followed by overfilling the intestines with rough food, and increased intestinal motility. Nodulation can occur at any level of the small and large intestines, where the mesentery is mobile. More often, nodes are formed from loops of the small intestine and sigmoid colon. The pinch ring is formed by the small intestine, and the sigmoid colon is pinched.
Volvulus of the small intestine is most often observed in the ileum. There are volvulus along the axis of the intestine and along the axis of the mesentery. The onset of the disease is acute, the pain is cramping in nature and is localized in the upper abdominal cavity or near the navel. Simultaneously with the pain, nausea and vomiting appear, which do not bring relief. All patients quickly experience stool and gas retention. The face is pale, the lips are cyanotic, the expression is pained, the tongue is dry. The pulse is frequent, weak filling, blood pressure is reduced. At the beginning of the disease, peristalsis is noticeable to the eye (symptom of hoses), during auscultation one hears increased peristaltic sounds of the intestines, the abdomen is of a normal configuration, soft, painful at the site of strangulation. Valya's symptoms quickly appear. After 6-8 hours, all phenomena decrease somewhat. Intestinal peristalsis weakens or is completely absent. You can often identify the symptoms of Mathieu-Sklyarov, Kivul, Spasokukotsky. A blood test determines neutrophilic leukocytosis, erythrocytosis, increased hemoglobin, decreased albumin, and hypochloremia. X-rays are used to diagnose Kloiber's cups located in the mesogastric area.
A cecal volvulus is accompanied on an x-ray, with the patient in a supine position, by a significant swelling of a single loop of the colon. Due to the fact that volvulus can occur in a well-moving cecum, it occupies one of three positions:
a) under the right half of the diaphragm;
b) in front of the spine;
c) to the left of the ridge, where one would expect the presence of a sigmoid colon.
Most often, the distorted cecum is located on the left, sometimes in front of the spine, very rarely on the right side. The twisted, distended cecum may have a kidney-shaped or oval-round shape. It has a funnel-shaped shape when the swollen loop is localized on the right or left, and round-oval when localized in front of the spine. The kidney-shaped form of the cecum occurs when it is distorted around a transverse or longitudinal axis, while the round-oval shape occurs when it is distorted around an oblique axis. In the area of the swollen intestine, contraction of the wall of the cecum and pronounced haustration are clearly visible, the disappearance of which indicates the possibility of intestinal necrosis.
Ileocecal angle volvulus occurs in 4% of all volvulus cases. There are three types of inversions of the ileocecal angle: around the axis of the mesentery, around its longitudinal axis and inflection, around its transverse axis. Volvulus is more common in older people because intestinal mobility increases with age. The disease begins with acute severe pain in the abdomen, mainly in the right iliac region and around the navel, vomiting, retention of stool and gas. A swollen cecum in most cases causes abdominal asymmetry, Wahl's symptoms. This type of obstruction is characterized by a false urge to stool and retraction of the right iliac region - the Schiemann-Dans symptom. An X-ray examination reveals a swollen cecum and a wide horizontal level in the right iliac region, and several small intestinal bowls to the left.
Transverse colon volvulus is rare and accounts for 0.5% of all intestinal volvulus. The clinical picture resembles the symptoms of acute strangulation obstruction. Upon examination and palpation in the middle part of the abdomen, painful tumor-like formations can be identified. The symptoms of Mathieu-Sklyarov and Grekov are positive. X-ray examination reveals a wide cup of Kloiber in the mesogastric area. When establishing a diagnosis, immediate irrigography and colonoscopy play an important role, with the help of which the level of obstruction can be determined.
Sigmoid volvulus is the most common form of strangulated intestinal obstruction. Mostly older men are affected. Volvulus of the sigmoid colon is associated with the development of folds of the mucous membrane due to cicatricial changes in the intestinal wall. Occurs in the presence of a long sigmoid colon and a narrow mesenteric root. The onset of the disease is acute. The pain is cramping in nature and is most often localized on the left. Vomiting may be absent for a long time, and then becomes a frequent occurrence, with a fecal odor. The skin is pale, the pulse is frequent. The tongue is dry. Retention of stool and gases is always observed. In the early stages of the disease, Wahl's syndrome is detected, positive symptoms of Mathieu-Sklyarov, Kivul, Spasokukotsky are determined. The patients are severely intoxicated and have impaired hemodynamics. The symptoms of Grekov and Tsege-Manteuffel are positive. An X-ray examination reveals a gas-inflated sigmoid colon in the form of a large horseshoe and wide levels at its base, a symptom of a “light belly.”
Nodulation is the most severe form of strangulation obstruction. There are known cases of death 12 hours after the onset of the disease, which is explained by early gangrene of the intestine, excluding a significant part of the intestine, and shock.
Nodulation gives a very high mortality rate, which reaches 40-50%, despite early surgical intervention. Occurs more often at night. Two sections of the intestine are always involved in nodulation, most often the sigmoid and small intestines.
Predisposing causes include: a) congenital or acquired excessively long intestinal mesentery, malrotation, b) scar cords, adhesions, adhesions between intestinal loops, both congenital and acquired, c) sudden weight loss with the disappearance of fatty layers between the layers of the mesentery. Producing causes include: a) a sudden increase in intra-abdominal pressure, leading to a sharp movement of intestinal loops, b) nutritional factors: irregular nutrition, prolonged fasting with subsequent overload of the intestine with a large amount of roughage.
Under normal conditions, the intestinal loops make significant movements and often make turns of up to 180°C without causing any pathological disorders. When the intestine is twisted more than 180°, its lumen is blocked and the mesenteric vessels are compressed. Hemorrhages and necrosis of the intestinal wall occur. Peritonitis subsequently develops.
Volvulus of the cecum is possible in cases where the intestine has its own mesentery or is common with the mesentery of the small intestine. The most common occurrence is sigmoid colon volvulus. In addition to the significant length of the mesentery, volvulus is facilitated by cicatricial wrinkling of the root of the mesentery of the sigmoid colon in mesosigmoiditis. The consequence of this is the convergence of the intestinal loops, which are located almost parallel (like a “double-barreled shotgun”). When peristaltic contractions increase or overflow with dense and gaseous contents, the intestine easily twists around its axis, which leads to obstruction.
Clinical presentation and diagnosis: small intestinal volvulus begins acutely. The disease occurs with severe general and local clinical symptoms characteristic of acute high strangulation intestinal obstruction. The leading symptom is sharp pain. Characterized by constant acute pain in the depths of the abdomen and in the prevertebral region. In the first hours of the disease, against the background of constant pain, cramping pain periodically occurs, the intensity of which increases synchronously with peristalsis, reaching the character of unbearable. Often patients scream in pain, become restless, and take a forced position with their legs brought to their stomach. . Vomiting from the very beginning is repeated and does not bring relief. |At first it is reflexive, with unchanged gastric contents and bile, and then takes on a fecaloid character. Retention of stool and gases does not always occur. Often at the beginning of the disease there is a single stool due to emptying of the lower intestines, which does not bring relief. The general condition is extremely serious. Disorders of water-salt, protein and carbohydrate metabolism, microcirculatory and hemodynamic disorders, intoxication quickly appear and increase, and diuresis decreases. The abdomen is moderately distended. Sometimes swelling of the follicle appears only as a smoothing of the subcostal areas. In the first hours of the disease, a positive Val's sign is often detected. At a later date, a “splashing noise” is determined over a distended strangulated loop of the small intestine (positive Sklyarov’s sign). During a survey fluoroscopy of the abdomen, Kloiber's cups are detected, which appear 1–2 hours after the onset of the disease.
Prognosis: with volvulus of the small intestine, poor. The mortality rate is 30%. With cecal volvulus, the symptoms are as acute as with small intestinal volvulus.
Pain (both constant and cramping) is localized in the right half of the abdomen and in the umbilical region. Vomiting appears at the beginning of the disease, but is rarely fecaloid. Retention of stool and gases occurs in most patients. Upon examination, asymmetry of the abdomen is revealed due to swelling in the umbilical region. At the same time, retraction of the right iliac region often occurs (positive Schiemann-Dans sign). Palpation of the abdomen often reveals rigidity of the abdominal wall muscles.
When listening to the abdomen, characteristic ringing peristaltic noises with a metallic tint are noted. Subsequently, as peritonitis develops, peristaltic sounds weaken.
A plain radiograph of the abdomen shows a spherically swollen cecum, which is localized in the right half of the abdomen or is displaced inward and upward. In the intestinal projection area, a large (up to 20 cm long) horizontal fluid level is visible. Sigmoid colon volvulus occurs more often in older people who have suffered from constipation for a long time.
The pain is of the same nature as in other forms of strangulation obstruction. They occur suddenly, intensely, and are usually localized in the lower abdomen and sacrum area. Vomiting once and twice. Fecaloid vomiting usually does not occur. It appears only with the development of peritonitis. The leading symptom is stool and gas retention. The abdomen is sharply swollen. Asymmetry is manifested by bulging of the upper parts of its right half. In this case, the stomach takes on a characteristic “skewed” appearance.
Due to severe swelling of the colon, all internal organs and the diaphragm are pushed upward. In this regard, patients have difficulty breathing and impaired cardiac activity.
Fluoroscopy reveals the sigmoid colon, sharply distended with gases, which occupies almost the entire abdominal cavity and gives the characteristic symptom of a “light abdomen”, against which 1–2 Kloiber cups with long fluid levels are visible. Treatment: In case of intestinal volvulus, emergency surgery is necessary, since conservative treatment methods are not effective.
Surgical treatment consists of straightening the twisted loops of intestine (detorsion) and emptying the intestine of its contents (decompression). If there is necrosis of the intestine, its resection is indicated. Resection is carried out according to the general rules adopted for the surgical treatment of acute intestinal obstruction (see above). In order to prevent relapse of the disease in cases of volvulus of the cecum and sigmoid colon, their fixation to the abdominal wall is necessary. Intestinal nodules (nodulus intestini). It occurs with severe circulatory disorders in the mesenteric vessels and early necrosis of large sections of the small and large intestine. It is observed in 3-4% of all patients with acute intestinal obstruction. Etiology - at least two intestinal loops take part in nodule formation. One of the intestinal loops, folded in the form of a double-barrel gun together with its mesentery, forms an axis around which the second intestinal loop, also together with its mesentery, twists one or more turns, compresses the first loop and itself undergoes strangulation. As a result of the formation of a node, the intestinal lumen is blocked at at least two levels.
The small intestine and mobile parts of the large intestine, which have their own mesentery, usually take part in nodule formation. The most common types of interintestinal nodes are those between the small intestine and the sigmoid or small intestine and the cecum, which in these cases has its own mesentery. Nodulation between the loops of the small intestine (jejunum and ileum) is rarely observed. The blood supply in the vessels of the mesenteries of the strangulating and strangulating intestines in the initial stages of the disease is disrupted to varying degrees. At the onset of the disease, the blood supply in the strangulated loop is usually more affected. Then the blood supply to both loops is quickly disrupted, and they find themselves in a state of necrosis.
Clinic and diagnosis: intestinal nodule formation should be assumed in cases where clinical and radiological signs of small intestinal strangulation are combined with signs of large intestinal obstruction, it is impossible to administer a high enema, there is a “balloon-shaped” ampulla of the rectum and horizontal fluid levels in the left parts of the large intestine (along with with fluid levels in the small intestine) Treatment: surgical.
In the early stage of the disease, the knot is untied. If it is impossible to straighten the node, which is often observed in the later stages, they resort to resection of large sections of the large and small intestine.
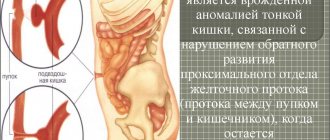
Prognosis: often unfavorable. Mortality is about 25%. Intussusception (invaginacio intestini). Intussusception is a type of obstruction that involves the penetration of the overlying segment of the intestine into the underlying one (descending intussusception). Intestinal intrusion in the opposite direction (ascending intussusception) is rare.
Resection: for intestinal necrosis within 30-40 cm proximal and 15-20 cm distal to the visible area of necrosis. It is necessary to determine the indications for intestinal tube intubation and choose its method, perform sanitation and drainage of the abdominal cavity in the presence of peritonitis.
| Treatment of strangulation forms of acute intestinal obstruction All forms of strangulation intestinal obstruction are subject to urgent surgical intervention. The operation is recommended to be performed under general anesthesia with the obligatory injection of 0.25-0.5% novocaine solution into the intestinal mesentery. When performing an operation under local anesthesia, it is necessary to first perform a bilateral novocaine lumbar blockade according to A.V. Vishnevsky. The best conditions for performing the operation are provided by a median approach. A median laparotomy is usually performed; in case of volvulus of the sigmoid and cecum, the operation can be performed through the lower median access. If the location of the obstruction is unclear, a lower median laparotomy is first performed; after revision of the abdominal cavity, if necessary, the incision is expanded upward. The operation consists of straightening the volvulus (detorsion); in case of intestinal gangrene, intestinal resection is performed. After straightening the volvulus in the presence of intestinal paresis, overflowing with intestinal contents, it is necessary to release the small intestine from contents and gases by puncture with a thick needle or enterotomy after preliminary application of a purse-string suture. Forcible reduction of swollen loops is unacceptable due to the risk of shock, serosa tears, intestinal ruptures and repeated volvulus in the postoperative period. The puncture site should be carefully sutured with purse-string and interrupted silk sutures. Resection of the intestine is also indicated if there is doubt about the viability of the intestinal loop, when warming with warm saline does not restore peristalsis and in the absence of pulsation of the mesenteric vessels. Assessing the viability of the intestine should be done with great caution, given that necrotic changes appear first in the mucous membrane, and the serous integument is affected last and may be little changed with extensive necrosis of the intestinal mucosa. Resection should be carried out within healthy tissues, necessarily with the removal of at least 30-40 cm of the afferent loop of the small intestine. However, it is necessary to caution against excessive, in particular, total resections of the small intestine. During resection, it is imperative to empty the afferent section of the small intestine of contents and gases using an electric suction through the intestinal lumen. |
Obstruction of the intestine by a tumor
Obstruction of the intestine by a tumor accounts for 9-10% of all forms of acute intestinal obstruction; its causes are mainly malignant tumors localized in the large intestine (usually in the sigmoid intestine), less often - tumors of the small intestine.
Clinical picture and diagnosis. Symptoms of intestinal obstruction develop gradually, subacutely, usually combined with symptoms of a malignant tumor (exhaustion, anemia, intoxication, etc.). Often, obstruction is the first manifestation of a colon tumor.
The disease can occur as either high or low obstruction. A sharp distention of the colon due to a tumor obstructing the sigmoid colon leads to severe disruption of microcirculation in the intestinal wall, ulceration and perforation.
Treatment. Surgical and conservative treatment is used depending on the cause of obstruction. For small intestinal tumors, intestinal resection with primary interintestinal anastomosis is performed. When the cecum and ascending colon are obstructed by a tumor, a hemicolectomy is performed. In the case of an inoperable tumor, a bypass ileotransverse anastomosis is performed. When the tumor is localized in the left parts of the colon, two- and three-stage operations are performed. In case of inoperable tumor of these parts of the intestine, an unnatural anus is created. Postoperative mortality is 20-30%.