General information
Duodeno-gastric reflux (syn. reflux gastritis , biliary reflux , alkaline gastritis , biliary gastritis ) is a pathological process of retrograde flow of bile contents of the duodenal intestine into the stomach, which can be accompanied by clinical symptoms, histological signs and endoscopic changes of reactive (chemical) gastritis.
The term "refluxus" means "reverse flow". Under physiological conditions, bile from the duodenum should not enter the anatomically overlying parts of the digestive canal, therefore the bile reflex is considered a pathological phenomenon. DGR occurs as a result of excessive flow of bile from the duodenum due to insufficiency of the pylorus, which acts as a barrier to the retrograde flow of bile or due to a violation (reduction) of anterograde peristalsis of the stomach and duodenum. Modern scientific research indicates an increase in the number of diseases caused by the presence of pathological duodenogastric reflux in patients. At the same time, the high prevalence of GHD (in 46-52% of cases) and the frequent combination with chronic gastritis , functional dyspepsia , peptic , GERD , stomach cancer , Barrett's esophagus , sphincter of Oddi dysfunction , duodenostasis , postcholecystectomy syndrome , etc. complicates their course and therapy. GHD is quite common after surgery (in 16% of cases after cholecystectomy and in almost 55% of cases after surgery for duodenal ulcers).
In addition, duodenal reflux can cause the development of metaplasia of the esophageal epithelium, severe esophagitis and squamous cell carcinoma of the esophagus against the background of metaplasia. It should be noted that gastroduodenal reflux in its “pure” form (positioned as an isolated diagnosis) is relatively rare (10-15%) and is mainly diagnosed against the background of other diseases. That is, in most cases, GHD is a syndrome accompanying a number of diseases of the upper gastrointestinal tract.
GHD occurs due to excessive flow of bile from the duodenum due to insufficiency of the pylorus, which acts as a barrier to the retrograde flow of bile or due to a violation (reduction) of anterograde peristalsis of the stomach and duodenum.
Thus, duodenal pathological reflux complicates the course of various organic/functional diseases of the gastrointestinal tract, which necessitates its timely diagnosis, correct clinical interpretation and adequate drug correction.
Classification
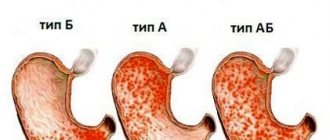
With duodenal reflux, pancreatic juice mixes with bile. As a result, a liquid with very aggressive properties is formed, which negatively affects the condition of the gastric mucosa. The composition of the substance is so caustic that it destroys its protective barrier. Gradually, the shell is damaged, these changes lead to serious consequences. The degree of damage determines the forms of DG reflux:
- Superficial. As a result of indigestion, the gastric mucosa is damaged, but for now only its outer layer is affected.
- Catarrhal. The mucous membrane is affected over the entire area. Most often, swelling is observed. Over time, the inflammatory process develops. In response to allergic reactions, long-term use of certain drugs causes so-called catarrhal reflux.
- Erosive. It often occurs if the patient does not adhere to the doctor’s recommendations regarding nutrition and regimen. For example, alcohol consumption or frequent stress can lead to this. As a result, small ulcers appear on the walls of the stomach.
- Biliary. This form of the disease develops when bile excretion is impaired. In severe cases, it can lead to liver dysfunction.
With duodenal reflux, pancreatic juice mixes with bile
In addition, with gastroduodenal reflux it is customary to distinguish the severity of the pathology. It depends on the duration of the process. Throughout the course of the disease, symptoms may change. During diagnosis, the severity of GHD is determined by analyzing contents from different parts of the stomach.
Pathogenesis
The pathogenetic mechanisms of development of GDR are based on:
- failure of the sphincter apparatus, which allows the contents of the duodenal intestine to freely reach the stomach through the pyloric/lower esophageal sphincters;
- antroduodenal dysmotility (disorder of coordination between the pyloric/antral parts of the stomach and duodenal intestine), which leads to disruption of control over the direction of flow of duodenal contents;
- elimination of the antireflux barrier after surgery (partial gastrectomy ).
With the development of pathological GHD due to dysfunction of the sphincters, bile retrogradely, as part of the refluxate, enters from the duodenum into the higher located stomach. Components of duodenal contents, represented by bile acids, lysolecithin and trypsin , have an aggressive damaging effect on the gastric mucosa. Taurine conjugated bile acids and lysolecithin have the most pronounced effect, especially at acidic pH, which determines their synergy with hydrochloric acid in the development of gastritis . Trypsin and non-conjugated bile acids have a pronounced toxic effect at slightly alkaline and neutral pH, while the toxicity of non-conjugated bile acids is provided predominantly by ionized forms that can easily penetrate the coolant.
Long-term exposure of the coolant to bile acids contained in bile causes necrobiotic and dystrophic changes in the surface epithelium and leads to the condition of reflux gastritis (gastritis C).
In the presence of Helicobacter pylori, the damaging effect of the refluxant on the coolant is enhanced. The formation of DGR contributes to disruption of the motility of various parts of the gastrointestinal tract and the function of the sphincters, which leads to disruption of the digestive conveyor, has a negative effect on membrane/cavity digestion and absorption of food ingredients, and changes the water balance. The aggressive influence initially manifests itself in the form of increasing atrophy, dysplasia and metaplasia of the coolant, which form the risk of developing gastrocarcinogenesis. The gradual aggressive effect of bile with pancreatic juice contributes to the fact that superficial gastritis progresses and mucosal erosions transform into erosive and ulcerative lesions of the coolant.
Duodenogastric reflux (DGR)
| Physiological duodenogastric reflux (Gubergrits N.B. et al.) |
Duodenogastric reflux
(
DGR
) is the reflux of the contents of the duodenum into the stomach.
Acceptable spelling: duodeno-gastric reflux.
Incorrect names:
duodenal gastric reflux, duodenal reflux, gastric reflux, gastroduodenal reflux
.
Duodenogastric reflux occurs in 15% of healthy people. At the same time, duodenogastric reflux is often a syndrome accompanying many diseases of the upper gastrointestinal tract: chronic gastritis, gastric and duodenal ulcers, gastroesophageal reflux disease.
If the contents of the duodenum are thrown not only into the stomach, but also into the esophagus, then such reflux is called duodenogastroesophageal.
Duodenogastric reflux existing for a long time leads to the occurrence of reflux gastritis, stomach ulcers and gastroesophageal reflux disease.
In the clinical picture of severe duodenogastric reflux, there is a high frequency and severity of pain and dyspeptic syndromes, a yellow coating on the tongue, and diffuse abdominal pain on palpation. Duodenogastric refluxes are very often combined with pathological gastroesophageal refluxes (Pakhomovskaya N.L. et al.).
pH-gram of the patient’s stomach body, duodenogastric reflux at night and in the morning (Storonova O.A., Trukhmanov A.S.)
Acidity index and the number of duodeno-gastric refluxes in healthy people
The table shows average quantitative estimates of acidity and duodenogastric reflux in “healthy” people (without complaints of gastroenterological problems and without any subjective sensations) (Kolesnikova I.Yu., 2009):
| Index | Day | Day | Night |
| Average acidity of the stomach body, units. pH | 3,2 | 3,1 | 3,3 |
| Average acidity of the antrum of the stomach, units. pH | 4,0 | 3,6 | 4,4 |
| Total number of DGRs | 64 | 31 | 34 |
| Duration of DGR, % | 40 | 35 | 47 |
| Number of DGRs lasting more than 5 minutes | 29 | 12 | 18 |
| Number of DGRs reaching the body of the stomach | 11 | 5 | 6 |
Duodenogastric reflux as a cause of reflux gastritis
Duodeno-gastric reflux is often the cause of the so-called reflux gastritis (according to the modern classification, classified as chemical gastritis or type C gastritis).
The thrown contents of the duodenum into the stomach have a damaging effect due to constant trauma to the gastric mucosa. Bile acids, which have detergent properties, promote the solubilization of lipids in the membranes of the surface epithelium. This effect depends on the concentration, level of conjugation and hydroxylation of bile acids and, very importantly, on the acidity of the stomach. In an acidic environment, only taurine conjugates damage the mucous membrane; other conjugates precipitate under such conditions. On the contrary, at high pH values, which is especially typical for the stump of a resected stomach, unconjugated and dihydroxyl bile acids have significantly greater damaging properties than conjugated and trihydroxyl bile acids. Lysolecithin, formed during duodenal hydrolysis of lecithin by pancreatic phospholipase, also plays a certain role in damage to the gastric epithelium (Babak O.Ya.). Conference "Esophagus 2013. Neurogastroenterology, motility, acid-related diseases." Academician of the Russian Academy of Sciences V.T. Ivashkin. On the screen is an intragastric pH-gram with duodenogastric reflux, obtained in the laboratory of Professor A.S. Trukhmanova.
Treatment of duodenogastric reflux with dioctahedral smectite (Smectite)
Duodenogastric refluxes, if they exist for a long time, can lead to the development of chronic gastritis (reflux gastritis type C), atrophy, accompanied by the development of intestinal metaplasia, further progression of proliferative processes and the possible development of dysplasia of varying severity, which increases the risk of malignancy. GHD is defined as any increase in gastric body pH above 5.0 that is not associated with food intake. GDR is considered pronounced if the duration of all GDR exceeds 10% of the time of monitoring the pH of the gastric body. The figure below shows the pH gram of patient D., 48 years old. Upon admission, the patient complained of heaviness and discomfort in the epigastrium and periodic heartburn. When conducting 24-hour pH-metry in the body of the stomach, hyperacidity and prolonged pronounced DGR were revealed, mainly at night and in the morning (Storonova O.A., Trukhmanov A.S.):
Taking into account the pH-metry data, the patient was prescribed a course of dioctahedral smectite, 1 sachet 3-4 times a day after meals (after 1.5 hours) and at night. With control pH-metry after 2 weeks, minimal GDR phenomena are detected in the morning (see the following figure). The continuous course of treatment was 1 month. Next, maintenance therapy was prescribed, 1 sachet at night (Storonova O.A., Trukhmanov A.S.).
The role of duodeno-gastric reflux in the development of GERD
Gastroesophageal refluxes are often combined with duodenogastric ones. When contacted with the esophageal epithelium of the esophagus, duodenal contents, in addition to gastric contents, play the role of a pathogenetic factor in the development of esophageal damage. Duodenogastroesophageal reflux aggravates gastroduodenal reflux, as it causes:
- increasing intragastric pressure and thus increasing the risk of gastroesophageal reflux
- effects on the walls of the esophagus of aggressive factors from the contents of the duodenum: bile acids, lysolecithin and pancreatic enzymes.
Damage to the gastric mucosa by duodenal contents leads to “specialized” intestinal metaplasia - a specific sign of Barrett’s esophagus - one of the complications of gastroesophageal reflux disease - a disease with a high risk of developing adenocarcinoma of the esophagus (Babak O.Ya.).
Clinical and functional variants of duodenal ulcer, depending on duodenogastric reflux
Duodenal ulcer disease (DU), depending on the characteristics of DGR, can occur in three clinical and functional variants. Data from 24-hour pH-metry allow us to identify three different functional variants of DGR in duodenal ulcers. The table below shows the corresponding average indicators for these three DGR options (Kolesnikova I.Yu., 2009):
| Index | Period of day | Clinical-functional version of the DU | ||
| 1st | II | III | ||
| Average acidity of the stomach body, units. pH | day | 2,4 | 2,5 | 2,1 |
| night | 2,1 | 2,7 | 1,6 | |
| day | 2,4 | 2,6 | 1,8 | |
| Average acidity of the antrum of the stomach, units. pH | day | 2,3 | 2,7 | 2,1 |
| night | 2,9 | 3,4 | 2,2 | |
| day | 2,8 | 3,1 | 2,2 | |
| Duration of DGR, % | day | 26 | 29 | 10 |
| night | 36 | 42 | 12 | |
| day | 30 | 33 | 10 | |
| Total number of DGRs | day | 15 | 12 | 8 |
| night | 26 | 17 | 10 | |
| day | 41 | 29 | 18 | |
| Number of DGRs reaching the body of the stomach | day | 1 | 5 | 0 |
| night | 3 | 6 | 0 | |
| day | 4 | 11 | 0 | |
Methods for studying duodenogastric reflux
Reliable diagnosis of duodenogastric reflux is possible using 24-hour pH measurements.
To exclude the buffering effect of food and drugs, fluctuations in acidity at night are analyzed. Duodenogastric reflux is considered to be a rise in pH in the body of the stomach above 3.0 (Pakhomovskaya N.L. et al.). Electrogastroenterography is also an effective way to study duodenogastric reflux.
, which provides complete information about the contractility of the stomach and duodenum, reveals the differences between physiological and pathological reflux and influences the methods of treating peptic ulcer (Stupin V.A. et al.). Electrogastrographic data on duodenogastric reflux most often coincide with data obtained using intragastric pH-metry and gastroscopy (Ponomareva A.P. et al.). To detect duodenogastric reflux, fibroesophagoduodengastroscopy is used, however, according to some authors, it itself can provoke GDR and, thus, lead to overdiagnosis (Albuzhi T., Sannikov O.R.). The sign by which gastroscopy determines the presence of duodenogastric reflux is the presence of bile in the gastric juice.
Professional medical work related to the manifestation, diagnosis and treatment of duodenogastric reflux:
- Volkov V.S., Kolesnikova I.Yu. Duodenogastric reflux and duodenal ulcer – let’s dot the I’s // Upper Volga Medical Journal. – 2010. – T. 8. – issue. 1. – pp. 26–29.
- Gnusaev S.F., Ivanova I.I., Apenchenko Yu.S. Diagnosis of gastroesophageal reflux in diseases of the upper digestive tract in children (a manual for doctors). — M:. 2003. - 50 p.
- Babak O.Ya. Bile reflux: modern views on pathogenesis and treatment // Suchasna gastroenterology. (Ukraine) – 2003. – No. 1. – (11).
- Sannikov O.R. Optimization of diagnosis of duodenogastric reflux in patients after cholecystectomy. Abstract of dissertation. PhD, 14.00.27 - surgery. PGMA named after. E.N. Wagner, Perm, 2007.
- Kolesnikova I.Yu. Clinical and functional variants of duodenal ulcer in the light of features of duodenogastric reflux. Abstract of dissertation. Doctor of Medical Sciences, 14.00.05 - internal diseases. TGMA, Moscow, 2009.
- Belousov S.S., Muratov S.V., Akhmad A.M. Gastroesophageal reflux disease and duodenogastric reflux. – N. Novgorod. – 2005. – 120 p. (table of contents).
- Golubeva E.Yu. The rhythm of acid formation in schoolchildren with pathology of the gastroduodenal zone and autonomic dysfunction. Abstract of dissertation. PhD, 14.00.09 – pediatrics. SPbMAPO, St. Petersburg, 2003
- Bart B.Ya., Mikhailusov S.V., Mikhailusova M.P., Melnikov K.V., Nikolaeva A.S. Duodenogastric reflux in clinical practice // Russian Medical Journal. 2013. No. 1. pp. 18–22.
- Mazurenko N.N. Duodenogastric reflux in children: a modern view of the problem // Bulletin of VSMU. – 2021. – Volume 17, No. 1. – P. 23-33.
- Galiev Sh.Z., Amirov N.B. Duodenogastric reflux as a cause of the development of reflux gastritis // Bulletin of modern clinical medicine. – 2015. – T. 8. – Issue. 2. pp. 50-61.
On the website gastroscan.ru in the literature catalog there is a section “Duodenogastric reflux”, containing publications devoted to duodenogastric reflux and their treatment. Back to section
Causes
The main reasons for the formation of DGR include:
- Congenital/acquired functional deficiency (weakening of the closing function) of the pyloric sphincter.
- Hyperkinetic type (with increased motility) of duodenal peristalsis.
- Inconsistency (discoordination) of the physiological cycles of relaxation/contraction of both the stomach and the DP-gut (migrating motor complex).
- Duodenal hypertension (increased pressure in the lumen of the duodenum), caused by splanchnoptosis (prolapse of internal organs), lumbar lordosis , hernias /malignant neoplasms.
- Long-term inflammation of the duodenum (chronic duodenitis , duodenal ulcer , gastroduodenitis ).
- Lack/absence of hormones ( gastrin ).
- Helminthic infestation (giardiasis).
- Anomalies in the development of the duodenal intestine.
Risk factors for developing duodenogastric reflux include:
- irregular food intake and poor quality nutrition (overeating, dry food, fatty and spicy foods that cause hypersecretion of bile);
- smoking and alcohol abuse;
- old age (after 60 years);
- long-term use of antispasmodics and NSAIDs;
- operations for resection of part of the stomach, cholecystectomy (removal of the gallbladder), anastomosis of the intestine and stomach;
- biliary dyskinesia , cholecystitis ;
- pancreatitis;
- diabetes mellitus , obesity .
Symptoms
Symptoms of duodeno-gastric reflux are not specific. As a rule, the disease manifests itself with a predominance of dyspeptic symptoms - nausea, heartburn, air/sour belching, bitterness in the mouth and vomiting bile. Periodically appearing pain in the upper abdomen, intensifying after eating, is cramping in nature and can be provoked by stressful situations, physical activity, or appear after surgery for gastrectomy, cholecystectomy, and with developed duodenal obstruction. Since GHD in its “pure” form is rare and is diagnosed mainly against the background of other gastrointestinal diseases, especially gastroduodenal pathology, the clinical symptoms of reflux are influenced by the symptoms of the underlying disease, which to a certain extent masks the symptoms of GHD.
Which products will be beneficial and which will be harmful?
Symptoms of the disease almost always occur after eating. But it is not enough to simply give up foods that cause heaviness in the stomach or heartburn. A therapeutic diet involves a gentle effect on the digestive system and at the same time contains all the beneficial substances necessary for the body. Here is a short list of foods that are allowed to be consumed:
Replacing your usual food with pureed cereals and pureed soups will help reduce the amount of bile secreted.
- ground porridge (rice, pearl barley, buckwheat, oatmeal);
- puree soups with weak broth;
- steam omelette;
- fish, always lean;
- fresh whole milk;
- low-fat cottage cheese, casseroles based on it;
- lean meat, preferably in the form of souffle, steamed meatballs or cutlets;
- pureed vegetables;
- butter and vegetable oils in small quantities;
- herbal teas;
- dried fruits compote;
- yesterday's bread.
Tests and diagnostics
The diagnosis is established on the basis of clinical symptoms and instrumental research methods, among which the most effective are:
- Daily pH-metry - allows you to assess the height of reflux and the profile of intragastric pH.
- Ultrasound diagnostics (echography with water load): with GHD, the retrograde movement of gas and liquid bubbles (corresponding to the reflux of duodenal contents into the stomach) from the pylorus to the body of the stomach is periodically recorded on echograms.
- Transillumination hemomotodynamic monitoring. The difference in motor wave amplitude in the antrum of the stomach and the duodenal bulb is used as a GDR parameter.
- Fibrogastroduodenoscopy (swelling of the coolant, focal hyperemia, pyloric dehiscence).
- X-ray of the stomach (regurgitation of barium from the duodenum into the stomach is noted).
- Fiberoptic spectrophotometry.
If bile reflux is suspected, differential diagnosis is made with acid gastroesophageal reflux and peptic ulcers of the stomach.
Traditional methods
Traditional medicine for gastroduodenal reflux is acceptable and often quite effective. The risk of side effects is minimal. It is important to remember that even the most harmless folk remedies must be agreed with your doctor. Most popular recipes:
- The herbs of chamomile, St. John's wort and yarrow are taken in any proportion, poured with boiling water, and infused. Drink twice a day, adding a small amount of infusion to regular tea. The product will relieve symptoms of gastritis and DH , relieves heartburn, and will help with dysbacteriosis.
- Fumiya herb in the amount of 2 tablespoons is poured with 0.5 liters of boiling water. It takes an hour. Take 50 ml every 30 minutes. Prevents the release of bile with vomiting.
- Mix crushed roots of calamus, sage - 50 g, angelica - 25 g. Pour boiling water at the rate of 1 teaspoon of mixture per glass of boiling water. Let it brew for 20 minutes. Take three times a day an hour after meals.
- One tablespoon of flax seeds is poured into 100 ml of cold water. Infuse them until the characteristic mucus is released. Take a teaspoon of the product on an empty stomach.
Constant relapses “wear out” the stomach and can lead to extremely negative consequences
Traditional medicine mainly uses various parts of medicinal plants, it is important to be careful not to cause allergic reactions. Otherwise, folk remedies are safe and have no side effects.
Diet
Diet for bile in the stomach
- Efficacy: therapeutic effect after 10 days
- Timing: constantly
- Cost of products: 1400-1500 rubles. in Week
Nutrition correction is a mandatory element of complex therapy. A diet is prescribed for bile in the stomach. Dietary nutrition is aimed at normalizing the motility of the gastroduodenal organs. The main nutritional requirements for the patient are: small frequent meals, adherence to a meal regimen, exclusion from the diet of spicy and salty foods, canned food, marinades, fatty, smoked and fried foods and dishes, wholemeal bread that reduce the rate of gastric emptying. The consumption of various vegetables and legumes rich in fiber (radishes, legumes, turnips, radishes, asparagus) and fruits with rough skin (gooseberries, grapes, dates, currants), as well as coarse cereals (pearl barley, barley, millet, corn) is limited. Limit the consumption of sugar, honey and jam, chocolate. The diet should be based on low-fat boiled, easily digestible foods: light soups, porridges, chicken meat without rough crust, boiled fish and vegetables/vegetable purees, fruit/oatmeal jelly.
Patients with GHD should avoid physical activity and heavy lifting after eating, which increases intra-abdominal pressure. It is equally important to prevent flatulence / constipation . However, since GHD occurs predominantly against the background of other gastrointestinal diseases, a diet for the underlying disease may be prescribed, for example, Diet No. 5 , Diet for gastric ulcer , Diet for gastritis , Diet for gastroduodenitis , etc.
Diet for GHD
The key to treating many diseases is proper nutrition. This is especially true for gastrointestinal diseases. The Harvard School of Medicine determined the influence of the esophageal sphincter on the occurrence of duodenogastroesophageal reflux. Some foods with GHD not only irritate the walls of the stomach and intestines, but also injure the sphincter.
In addition to limiting the consumption of certain types of food, the diet for GHD has some recommendations regarding diet and cooking:
- preference should be given to food boiled in water, steamed, or baked;
- the temperature of the dishes is strictly warm, not hot or cold;
- fractional meals - 5-6 meals per day;
- it is necessary to exclude all acidic foods, including fermented milk and certain fruits;
- eat chopped food;
- You need to chew each piece very carefully;
- completely eliminate the possibility of overeating.
Some foods with GHD not only irritate the walls of the stomach and intestines, but also injure the sphincter
You can make a list of “bad” foods yourself by observing your condition and recording the results in a notebook. After eating, it is advisable to avoid physical activity and sudden movements for 30-60 minutes. Replacing your usual food with pureed porridge and pureed soups will help reduce the amount of bile secreted. It is allowed to eat low-fat fish and meat. Although fermented milk products are prohibited, milk and curdled milk are allowed.
Prevention
Prevention of GHD consists of:
- Timely treatment of gastrointestinal diseases (especially gastroduodenal pathology).
- Correction of body weight.
- Maintaining the correct diet to ensure physiologically normal gastrointestinal motility.
- Quitting smoking and alcohol abuse.
- Normalization of physical activity and psycho-emotional sphere. Elimination of factors that provoke reflux (lifting weights, exercises with strong abdominal tension, avoiding being in a horizontal position after eating, working in an inclined position).
- Exclusion/avoidance of long-term use of medications that worsen bile rheology and gallbladder motility (antibiotics, expectorants, sedatives, NSAIDs, estrogens, antispasmodics, β-blockers, hypnotics, calcium channel blockers).
List of sources
- Zvyagintseva T.D., Chernobay A.I. Functional disorders of the motor-evacuation function of the digestive tract and their pathogenetic correction // News of medicine and pharmacy. – 2009.– No. 294. pp. 7–11.
- Zvyagintseva T.D., Chernobay A.I. Duodenogastric reflux in the practice of a gastroenterologist: obvious dangers and hidden threats // Medical newspaper “Health of Ukraine”. 2012.—No. 1. P.11.
- Trukhan D.I., Filimonov S.N. Differential diagnosis of the main gastroenterological syndromes and symptoms. M.: Practical Medicine, 2021. 168 p.
- Trukhan D.I. Rational pharmacotherapy in gastroenterology // Directory of a polyclinic doctor. 2012. No. 10. pp. 18–24.
- Bagnenko G.F., Nazarov E.V., Kabanov M.Yu. Methods of pharmacological correction of motor-evacuation disorders of the stomach and duodenum. // Rus. honey. magazine. Diseases of the digestive system. –2004. – T. 1. – P. 19-23.