Today, there are several methods to identify Helicobacter pylori: analysis for antibodies to Helicobacter pylori, stool analysis by PCR, urease breath test, biopsy, cytology. The most effective are IFA (enzyme-linked immunosorbent assay) for Helicobacter and stool analysis (PCR).
Diagnosis of Helicobacter pylori is carried out using two methods:
- invasive (endoscopy with biopsy)
- non-invasive (laboratory methods).
A reliable method for determining Helicobacter is invasive. A test for the bacterium is carried out for everyone who complains of pain and discomfort in the stomach.
Detection of pylori igg antibodies is routine in studies of the epidemiology of infection.
Breath test - definition and its types
A breath test to detect Helicobacter pylori is a diagnosis of infection that allows you to identify the activity of Helicobacter pylori and assess the level of infection. Gastroenterologists, therapists, and pediatricians often use it in their practice. The Helicobacter pylori breath test is used for the initial diagnosis of the bacterium. They are also used to monitor the treatment process of the disease and check the effectiveness of therapeutic treatment.
The method is absolutely safe, the most effective and in demand in medicine today. The analysis shows the waste products of bacteria in the air that the patient inhales.
There are two main types of method. They differ in the reacting component:
- carbon
- ammonium
Carbon breath analysis provides a more accurate result.
Advantages and disadvantages of the method
This respiratory method has its advantages:
- The result is ready in a short period of time (20-25 minutes).
- Reliability of the result is 90-95%.
- The test does not harm the human body.
Since the method has only advantages, it has no contraindications. But the result will be accurate only if you prepare for the test correctly.
Preparing for a breath test
In order for the test to give the most accurate results, special preparation for the breath test is recommended:
- one month before the test, you should not take antibiotics;
- three days before the examination, do not drink legumes and alcoholic beverages;
- 6 hours before the test, do not eat anything;
- 14 days before the examination, avoid taking drugs that suppress the course; physiological and enzymatic processes in the body;
- You can’t chew gum or smoke for a few hours;
- the last meal no later than 22 hours, it should be a light dinner;
- one hour before the examination you can drink no more than 10 ml of water;
- for the analysis result to be accurate, the patient should not move;
- Before the examination, thoroughly clean your teeth and mouth.
It is very important to prepare for the test correctly, otherwise you will not get an accurate result. If the patient was unable to comply with all the rules, he must inform the doctor about this and another time will be assigned to him.
How the test is carried out
The procedure is carried out in a hospital setting under the supervision of a specialist. If the examination is carried out using a tube, the manipulation lasts no more than 15 minutes. If an electronic device is used, the procedure time is 10 minutes.
The procedure is simple:
- the patient takes a comfortable position
- a plastic tube is placed in the mouth, and breathing should be normal
- it is advisable not to touch the tube with your tongue and palate so that saliva does not get there
- if saliva accumulates, you can spit it out or swallow it, pull out the tube and take an air sample
- the first stage of manipulation lasts 6 minutes
- the patient is given a carbamide solution to drink
- the tube is placed back in the mouth
- the second stage also lasts 6 minutes, air testing is carried out
- after this the result is displayed.
Interpretation of analysis results and normal indicators
The norm is when the difference between the indicators of the first and second stages of the survey is zero. If there is Helicobacter in the body, the indicator will be above zero.
With the indicator:
- trace value is 1.5 -3.5, the microorganism is in an inactive phase and can be quickly gotten rid of;
- 3.5 - 5.5 – low level;
- small - up to 7 ppm;
- from 7 to 15, the bacteria is in the active phase, multiplying, the treatment process becomes difficult;
- above 15 – high level of contamination.
With any positive result, therapy should be started immediately, this will avoid complications and pain. But the Helicobacter treatment regimen must be drawn up by a doctor.
Contraindications for carrying out
The method has no contraindications, as it does not include any interventions or stress. It can be used for everyone, without restrictions.
Blood tests
If the patient complains of pain in the stomach, any discomfort, with functional digestive disorders, with gastritis and peptic ulcers, a blood test is taken for Helicobacter pylori. Antibodies to helicobacter pylori in the blood are an indicator of human infection with the bacterium helicobacteriosis.
It is recommended to donate blood for Helicobacter bacteria if:
- weak immunity
- hereditary predisposition to stomach cancer
- as a preventive diagnosis
- to evaluate the treatment received for the infection.
How to prepare for the analysis?
Before the analysis, you must not eat food, coffee, tea, alcoholic drinks, or smoke 8 hours before the test. This test for Helicobacter pylori determines the amount of immunoglobulins. When a certain toxin enters the human body, a virus, microbe, immunoglobulins interact with them and neutralize these harmful substances. The analysis shows the interaction of the pathogen and immunoglobulins, which makes it possible to determine whether Helicobacter pylori is in the stomach or duodenum.
Advantages and disadvantages
Advantages of this test:
- the diagnostic procedure is not expensive;
- high accuracy of the result;
- analysis is available to everyone.
The test for Helicobacter pylori has its drawbacks:
- there are factors that influence the result of the analysis;
- some patients experience fear when taking blood;
- thorough results are obtained in 4-6 days.
Analysis transcript
Deciphering the result of a blood test for Helicobacter pylori can be done without medical skills. Antibodies are divided into categories A, G, M. Opposite each category there is a result on the form. If all blood test parameters for Helicobacter pylori do not exceed the norm, then there is no bacteria in the body:
- immunoglabulin LgG is absent or significantly lower than normal: bacteria are absent in the body;
- LgG detected: helicobacteriasis is present or has been previously experienced;
- immunoglabulin LgM was not detected or below the norm: conditional norm for Helicobacter pylori;
- LgM class detected: initial stage of the disease;
- immunoglabulin LgA is not detected in the blood: this may indicate an early stage of the disease, recent antibiotic therapy, or the patient is in the recovery stage.
Contraindications
A blood test for Helicobacter is not performed:
- for convulsions
- with increased excitability of the patient
- if there is skin damage at the injection site.
A blood test for antibodies is also not prescribed for venous phlebitis.
Stomach and esophagus / Does Helicobacter exist and how to check for it?
There are many microbes in the world, they are around us, they live in the external environment, and some can live inside us. For example, bacteria in the intestines. But not all bacteria can reach it, since most microbes die in the stomach. Bacteria enter the stomach in large numbers, and die in the same large numbers.
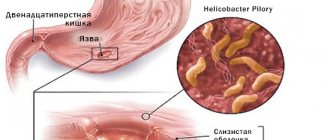
We are fundamentally interested in Helicobacter because it can potentially cause stomach problems. Other microbes can too, but fortunately they quickly die in the stomach, and if they manage to harm it, it is very little. So you don't even have to fight them. But Helicobacter can live in the stomach indefinitely, since the body cannot get rid of it on its own.
You can get this microbe from another person who already has it. Possible, but not guaranteed! You need to treat this bacteria like you would any other infection, such as the flu. After all, you can get sick or not get sick, even if someone sneezed on you. Because there are 3 levels of immune defense that normally prevent infection.
That bacterium settles in the stomach for a long time, and this is the main problem. However, bacteria are different. And just like there are breeds of dogs or cats, there are also “breeds” of Helicobacter. Some species cause stomach ulcers, not instantly, but gradually - first irritation, then slight inflammation, then major inflammation, then erosions resembling abrasions, and then ulcers. Other types of Helicobacter cause atrophy in the stomach, also not immediately - first there is mild inflammation, then the stomach wall becomes thin, produces less acid, there are fewer vessels in it, atrophy appears, then metaplasia, then dysplasia, more dysplasia and stomach cancer.
Apparently, this Helicobacter bacterium is really dangerous, but there is nothing urgent or urgent about it. We can cure her in time. Not always, but in many people we can determine which specific type of Helicobacter has entered the stomach.
It's not that difficult to check. You just need to get tested. But the assortment is large and it can be difficult to choose. There is the simplest test, the rapid breathing test, quickly breathe into a tube and get the result. Unfortunately, it does not show the bacterium itself, but its metabolic products. The same waste may come from other bacteria, so there is no guarantee that Helicobacter is actually in your stomach. The same rapid test is also done during gastroscopy directly inside the stomach.
A more reliable analysis is to take a sample from the stomach (biopsy), special staining and examination under a microscope, counting the number of microbes. But this is now done very rarely, it is too labor-intensive. It is much easier to take a stool test and determine the antigens of the bacterium in it, that is, fragments of its shell. If Helicobacter is present in the stomach, it is always in sufficient quantity so that its pieces are excreted in the feces. Inconvenient, but simple.
There is also a blood test for Helicobacter, which also determines not the bacterium itself, but the reaction of the immune system to it. Therefore, this examination will only help those who have not had Helicobacter before and were found for the first time. Also, a separate version of a blood test allows you to determine what the bacterium is capable of. That is, it can cause an ulcer or atrophy, or both an ulcer and atrophy, or it is defenseless and harmless.
Unfortunately, you need to prepare for the tests, for example, do not eat before the blood test, take hormones in the morning, and so on. Very often they forget about this when they are tested for Helicobacter. As a result, we get a false positive result or a false negative, thus we treat what is not necessary and do not treat what needs to be cured.
The most common rapid test (respiratory or endoscopic) needs to be double-checked; it has very low specificity. The blood test is only for those who have not previously been treated for Helicobacter. And, most importantly, you should not take stomach medications for 1 month before the test in order to get the correct result. But the stomach hurts and heartburn torments, so many people do not stop taking the pills and get tested, but in the end they get the wrong result. If you have already started taking the pills yourself and cannot stop taking them because the pain is returning, then you need to go to the doctor for temporary treatment in order to get the correct test result.
The answer is quite simple, but there are two conditions. First, Helicobacter needs to be treated if you have it, because if it is not there, then there is simply nothing to treat. Secondly, it needs to be treated if we understand that it is really pathogenic, because there are also non-pathogenic types of this bacterium. Third, it needs to be treated if there is already a risk of developing serious stomach problems.
In real life, it turns out that we use unreliable diagnostic methods, or take medications that change test results, and then treat the false result, and even with the wrong medications. Although effective treatment regimens for Helicobacter are known, they are quite safe and have virtually no side effects. Therefore, it is best to test yourself using a reliable method and, if necessary, recover, rather than carrying a time bomb with you all your life and not treating something that does not exist.
Stool analysis
PCR – what is it? This is a sensitive way to detect infection. It recognizes the DNA or RNA of the pathogen. For PCR, the material for research is feces.
A stool test for Helicobacter antigen is the most convenient test for the elderly, children and seriously ill patients. In this case, the presence of the patient in the laboratory is not required and the procedure is not associated with injury to the body. By the way, we will talk about Helicobacter pylori in children separately.
But detecting bacteria in stool is not easy. In the intestine, the microorganism is exposed to unfavorable conditions for it (bile acids, lack of oxygen). Therefore, active organisms adapt to new conditions, change their shape and their number sharply decreases.
A special method of polymerase chain reaction (PCR) is used, which allows you to determine the DNA fragment of a microorganism. The accuracy of the result is 95-96%.
What not to do before donating stool
It is important to know how to get tested for Helicobacter. Before donating stool, it is not recommended to take a lot of dietary fiber, coloring foods, inorganic salts, or medications that increase intestinal motility for 3-4 days.
Stool after an enema or laxative is not suitable for testing for Helicobacter.
A stool test for Helicobacter pylori is carried out before starting treatment. If the patient has previously taken antibiotic therapy for the treatment of any disease, it is better to prescribe a different method of examination.
Analysis transcript
The test result for helicobacter pylori can be positive or negative. A positive result indicates the presence or past infection. Negative data - about the absence of disease or incorrect conduct of the study.
Detailed description of the study
Helicobacter pylori (H. pylori) is a spiral-shaped bacterium that affects up to 50% of the population worldwide, with a higher prevalence in developing countries. H. pylori is the most significant cause of chronic gastritis, peptic ulcers, lymphoma and gastric cancer.
Infection with H. pylori occurs in early childhood, and in most cases the bacterium continues to remain in the body of the infected person throughout life. Transmission of H. pylori occurs primarily through the fecal-oral route (usually through dirty hands due to poor hygiene), and less commonly through the oral-oral route - through contact with infected saliva, for example, when an infected parent or relative kisses a child during childhood. Among children under 10 years of age, on average, 5%-10% are infected with this infection. The prevalence of H. pylori varies around the world, with higher rates of infection observed in developing countries. In Russia, about 60% of the adult population is infected with H. pylori.
There are four important components that lead to the formation of diseases caused by H. pylori. Firstly, this bacterium has the enzyme urease, which neutralizes chemically aggressive gastric juice. Secondly, the presence of flagella helps H. pylori actively move towards the epithelial cells of the host's stomach. The third advantage is the release of special adhesin proteins that interact with stomach cells, which leads to the successful establishment of the pathogen in the host body. Fourth, the bacterium produces toxins that allow it to survive and multiply in the stomach. All of these factors ultimately lead to damage to the stomach tissue and the development of chronic inflammation.
Most people have no symptoms of H. pylori infection. Clinical manifestations, if present, are usually associated with symptoms such as abdominal pain, predominantly on an empty stomach, nausea or heaviness after eating. Examination often reveals a violation of the integrity of the gastric mucosa - ulcers or erosions. There are various extragastric manifestations associated with H. pylori infection, such as anemia and chronic immune thrombocytopenia. The long-term presence of this bacterium in the body increases the risk of developing lymphoma and stomach cancer. This risk is higher among those whose close relatives suffered from these diseases.
When infected with H. pylori, microscopic inflammation of the stomach is always observed. Changes in the mucous membrane of organs are often not visible during endoscopic examination. The “gold standard” for detecting H. pylori infection is taking a biopsy from several parts of the stomach and then examining the resulting samples under a microscope.
Taking a small fragment of stomach tissue, followed by staining and fixing the resulting micropreparation on glass, allows you to study in detail the changes in the cells of this organ under a microscope. Imaging of H. pylori in such a study has a sensitivity and specificity of 90% or more.
Cytological analysis
Cytology is one of the most accurate methods for detecting Helicobacter pylori in the gastric mucosa. With this method, testing for Helicobacter pylori practically does not give false positive results.
For research, a biopsy material is taken during fibrogastroduadenoscopy (fgds), a smear is an imprint of the mucous membrane. The result can be positive or negative. According to the degree of contamination:
- weak - with a magnification of 360 times, up to 20 bacteria are detected in the field of view;
- moderate – 20-40;
- high – more than 40 bacteria.
Analysis for Helicobacter Pylori (HELICOBACTER PYLORI)
Testing for Helicobacter pylori is recommended for anyone who complains of pain and discomfort in the stomach. Since Helicobacter pylori infection provokes the development of many lesions of the mucous membrane of the stomach and duodenum, its timely detection and elimination allows one to avoid the development of serious health problems, including cancer.
Analysis for Helicobacter pylori: an idea of the causative agent of Helicobacter pylori infection
Helicobacter pylori is one of the most common human infections today. Literally, the name of this microorganism means “spiral-shaped bacterium that lives in the pylorus” (the pylorus is the lower part of the stomach, which passes into the duodenum). It belongs to anaerobes - that is, microbes that die in air. The infection is transmitted from person to person through saliva and mucus.
Infection more often occurs within a family or other closely communicating groups, since the infection spreads when using the same utensils, failure to comply with hygiene rules, and overcrowding. Often the infection is transmitted from mother to child (through saliva that gets on the pacifier, spoon and other objects). You can become infected with Helicobacter pylori infection even by kissing.
Once in the human body, Helicobacter descends into the stomach. Next, this microorganism - almost the only bacterium that is not destroyed by gastric juice containing hydrochloric acid - burrows into the gastric mucosa, disrupting the structure of its tissues and their functions. This potentially leads to inflammation of the gastric mucosa (gastritis), erosions and ulcers. In addition, Helicobacter pylori changes the local acidity of the stomach, which leads to a violation of the protective properties of its membranes.
With weakened immunity and long-term existence in the body, Helicobacter pylori can spread both to the overlying parts of the stomach and to the duodenal bulb. This leads to further disruption of the structure and functions of the mucosa, the spread of the inflammatory process and the appearance of new erosions and ulcers.
A clear connection has been established between Helicobacter pylori infection and the development of gastritis, gastric and duodenal ulcers, stomach cancer and a number of other diseases.
Test for Helicobacter pylori: does everyone infected with the bacterium Helicobacter pylori get sick?
Fortunately, despite the fact that 2/3 of humanity is infected with Helicobacter, most infected people are not bothered by it. Not all carriers of Helicobacter pylori develop peptic ulcers and other health problems.
This is where predisposing factors come into play - poor diet, stress, smoking and alcohol, which help Helicobacter do its dirty work. Helicobacter pylori itself does not cause specific symptoms. Its presence in the body can be suspected only when stomach diseases occur.
Helicobacter pylori test: who needs to take it?
Of course, getting tested for Helicobacter pylori is pointless as long as a person can boast of excellent health. But any symptoms of “stomach malaise” should be a reason to visit a gastroenterologist or therapist.
The following signs of trouble with the digestive system should alert you:
- recurring pain in the stomach, especially after eating (a sign of erosions and ulcers);
- appearance or intensification
- heartburn
- feeling
- heaviness in the stomach,
- aversion to meat food (even to the point of vomiting).
In order to determine the presence of Helicobacter pylori in the stomach, today there are a number of methods. The most effective of them can be considered tests for Helicobacter pylori, such as enzyme immunoassay.
Test for Helicobacter pylori: enzyme immunoassay for IgG antibodies to Helicobacter pylori.
Test for Helicobacter pylori: what is an enzyme immunoassay for IgG antibodies to Helicobacter pylori?
This test for Helicobacter pylori is a laboratory test that can determine the level of immunoglobulins (or antibodies) in the blood.
Test for Helicobacter pylori: what are immunoglobulins?
Immunoglobuins are proteins that are produced by blood cells. When a pathogen of a particular infection enters the human body, immunoglobulins bind to it (form a complex) and neutralize it after some time. As many different microbes, viruses and toxins as there are, there are as many different immunoglobulins as there are. Together with blood, they can penetrate into any, even the most distant corners of our body and overtake “aggressors” everywhere. Experts distinguish between immunoglobulins G, M and A, and designate them as IgG, IgM and IgA.
Test for Helicobacter pylori: what is IgG?
This is an indicator confirming the presence of Helicobacter pylori in the human body. Immunoglobulins of this class are detected starting 3-4 weeks after infection. A high level of IgG to Helicobacter persists before and for some time after the elimination of the microorganism.
Helicobacter pylori test: what are the normal values for IgG?
The OLIMP laboratory has its own normal indicators (so-called reference values). They are indicated on the result form. When the antibody level is below the threshold value, the result is considered negative; above the threshold value, the result is positive.
Analysis for Helicobacter pylori: how to decipher the test result?
Positively
A positive result of an ELISA test for IgG to Helicobacter indicates either the presence of Helicobacter infection (high risk of developing peptic ulcer or peptic ulcer; high risk of developing stomach cancer); or that the Helicobacter pylori infection has been cured: a period of gradual disappearance of antibodies.
Negative
A negative result of an ELISA test for IgG to Helicobacter indicates either the absence of Helicobacter pylori infection (low risk of developing a peptic ulcer, but a peptic ulcer cannot be excluded), or that the Helicobacter infection occurred recently (up to 3-4 weeks ago)