Causes of colon cancer
The causes of colon cancer, like any other oncology, are not known for certain, but there are risk factors for its development:
- A diet high in animal fats, carcinogens,
- Heredity,
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis),
- Smoking,
- Alcohol.
A cancerous tumor can arise from the degeneration of a polyp (benign neoplasm) or appear on its own. It develops slowly and may not manifest itself in any way in the early stages.
The most common clinical manifestations of colon cancer are blood in the stool or black stool (if the lesion is located further from the rectum) and intestinal obstruction (if the lesion is closer to the rectum). However, these symptoms occur in later stages, when the tumor has penetrated deep into the intestinal wall or has grown to a large size, closing part of the intestinal lumen. Treatment at such stages is no longer effective, so screening plays an important role in the early diagnosis of colon cancer.
Screening is a mass examination that allows you to identify a group of people who require more thorough diagnosis. Stool occult blood testing and colonoscopy are used to screen for colon cancer.
Operations
If possible, radical removal of the tumor node with underlying tissues within the limits of possible damage and removal of lymph nodes are always performed. Often the required extent of surgery becomes apparent only upon direct examination of the affected area.
The basic principles of oncosurgery are applied:
- Radicality. Elimination of all malignantly damaged tissues, removal of regional lymph nodes.
- Ablasticity. Extraction of tumor cells without even the slightest particles getting into intact areas. Creation of conditions during surgery to prevent the dissemination (spread) of cancer cells.
- Organ preservation - the surgeon must maintain a balance between complete removal of tumor tissue, thereby saving the patient’s life, and preservation of organs (if possible) to reduce disability and ensure a good quality of life for the patient in the future.
- Restoring intestinal patency.
Often operations are carried out in two stages, when the tumor is first removed and a stoma (unnatural opening) is created to drain feces. This creates conditions for rapid healing of the operated area. Then, in the second stage, the normal path of bowel movement is restored.
Among the surgical methods, typical operations, combined operations (remove the tumor site and organ affected by metastasis), and extended interventions for widespread or synchronous tumor processes are used. For colon cancer, the prognosis for survival after surgery directly depends on the stage of the disease and the degree of tumor differentiation. The smaller the malignancy, the earlier radical treatment is started, the greater the chances of a complete cure and maintaining quality of life in the future.
Modern methods and equipment used in our clinic make it possible to remove both low-lying colon cancer (rectum) and large tumors in the overlying sections. Without large incisions on the abdomen (endoscopically), it is possible to perform:
- Transanal resection of the lower ampullary rectum.
- Transanal microsurgical excision of neoplasms.
Sectoral resection of the rectum and anal canal is performed for stage 0-1 cancer located below the dentate line, which allows preserving the obturator apparatus of the rectum.
Diagnostics
More in-depth diagnostic methods include:
- Colonoscopy with biopsy
- Irrigoscopy (administration of a contrast agent using an enema and an x-ray of the abdomen with contrasted intestines)
- Computed tomography, magnetic resonance imaging of the abdominal cavity
- Ultrasound of the abdominal cavity and pelvis
- Blood test for tumor markers
- Diagnostic laparoscopy/laparotomy (operations that allow you to see the nuances of the oncological process that are inaccessible to other diagnostic techniques)
Abdominal cramps and bloating
This problem, like aching pain around the navel, is difficult to correlate with cancer. Cramps and bloating may accompany an intestinal infection, poisoning, or simple indigestion. They occur when pathogenic bacteria multiply in the digestive tract. In cancer, the microflora deteriorates due to the activity of “sick” cells and their rapid proliferation.
Remove legumes, pastries, sugar from the menu and monitor your condition. Pay close attention to cramps as a possible symptom of cancer if they occur every day even with the “safest” diet. As the tumor develops, flatulence intensifies, and abdominal pain no longer disappears.
Treatment of colon cancer
Treatment of colon cancer is complex and includes:
- Surgical removal
- Drug treatment (chemotherapy, targeted therapy, immunotherapy)
- Radiological treatment
Surgical treatment involves resection of the part of the colon affected by the tumor and the creation of an anastomosis or removal of the stoma to the surface of the body, as well as the removal of lymph nodes into which tumor cells can spread.
Chemotherapy can be given before surgery or both before and after. Its goal is to reduce the risk of cancer cells spreading and destroy existing metastases. The decision on additional drug therapy is made individually for each patient.
Treatment methods at the Federal Scientific Center
- Laparocentesis, thoracentesis, drainage and stenting of the bile ducts for obstructive jaundice
- Conducting palliative/symptomatic therapy
- Chemoembolization of liver tumors
- Effective pain relief using modern techniques
2. Reasons
The etiopathogenesis of cancer, that is, the appearance and non-stop division of immature cells with the development of a tumor from them, growing into neighboring structures, forming its own blood supply network and capable of metastasizing to other parts of the body, is beyond the scope of this article. Let us only note that this mechanism, common to any oncological pathology, still remains the subject of intense research; this, of course, does not mean that it is completely unknown, however, the immediate causes of the fatal “breakdown” of the immune system (one of the tasks of which is the identification and destruction of immature cells) have yet to be established and clarified, which will ultimately make it possible to develop means of reliable prevention and treatment.
Risk factors that contribute to the initiation of the cancer process in the sigmoid colon are well known:
- unhealthy diet with a predominance of “cooked red meat” (WHO wording), fats, sugar and all those food additives, most of which are clear and aggressive carcinogens; insufficient consumption of plant foods and fluids;
- physical inactivity, excess body weight;
- alcohol consumption and smoking (these factors are not included for propaganda purposes: it has long been reliably proven, for example, that in relation to colon cancer, smoking is not only a pathogenetic factor, but also doubles mortality despite therapy);
- mature and old age, especially in the presence of the above risk factors;
- inflammatory and/or ulcerative processes in the intestines;
- tendency to constipation due to hypotension and weakened peristalsis;
- hereditary predisposition;
- the presence of asymptomatic polyps and papillomas in the intestines (some genetically determined forms of polyposis practically guarantee malignancy, i.e. malignant degeneration of intestinal polyps).
Visit our Oncology page
Dyspnea
This sign of oncology occurs in late stages. Due to exhaustion, in addition to fatigue and weakness, patients may experience breathing problems. Even walking a short distance or laughing loudly for a long time causes discomfort. There is no talk of heavy loads. Breathing becomes shallow and rapid, and there is pressure in the chest. The appearance of tachycardia - increased heart rate - is possible.
Systemic symptoms of colorectal cancer
Colon cancer affects not only the digestive tract, but also the condition of the entire body. The general manifestations of the disease are called systemic; without them, cancer can easily be confused with other gastrointestinal problems.
Characteristic general symptoms:
- Unexplained loss of appetite, changes in taste.
- Nausea, vomiting not associated with food intake.
- Yellowing of the skin, whites of the eyes, anemia.
If metastases (secondary foci of cancer) have spread to other organs, the following may appear:
- stiffness and pain in the joints;
- cough and chest discomfort;
- swelling of the limbs;
- increased liver volume;
- confusion;
- headaches, cramps.
Reviews from our patients
- Feedback on bowel cancer treatment
Review of bowel cancer treatment March 2, 2021The patient is undergoing treatment for an intestinal disease. Surgery was performed. To date, the sixth course of adjuvant chemotherapy has been completed. The patient tolerated the treatment satisfactorily. A state of remission has been achieved. After a follow-up examination, an operation to close the colostomy is planned, as well as six courses of chemotherapy.
read more
- Bowel cancer. Review of treatment
Bowel cancer. Review of treatment January 11, 2021
The patient was admitted with intestinal disease. During the hospitalization period, control examinations were carried out. The first course of chemotherapy was completed. Further treatment tactics have been determined.
read more
- Feedback on hemicolectomy
Review of hemicolectomy May 11, 2021
The patient was admitted to us in critical condition. The diagnosis is intestinal obstruction due to cancer. The illness came unexpectedly. The only hospital in the community was repurposed to fight coronavirus. The patient went to a paid medical center, but they could not help. The condition gradually worsened. When contacting us, the patient promptly underwent surgical intervention involving a left-sided hemicolectomy. The patient tolerated the operation well. Recovery period...
read more
- For treatment from Vladivostok to Moscow
For treatment from Vladivostok to Moscow on May 7, 2021.
What to do if cancer is complicated by heart problems? You will be helped at the Medicine 24/7 clinic. The patient came to us from Vladivostok with her sister. Cancer is complicated by heart rhythm disturbances. The patient might not have been able to endure the complex operation. An interdisciplinary consultation was held to determine treatment tactics. The patient was fitted with a pacemaker, which will help her in the future. The next day, May 1, an operation was performed to resection the tumor….
read more
How is metastatic cancer treated?
In case of metastases to other organs and a small size of the primary formation, which can technically be removed, everything is determined by the possibility of removing these metastases. If there are few of them and it is technically possible to remove all metastases including part of the lung or liver, then a one-stage surgical intervention is performed on the intestines and metastatic foci. Good results are achieved with radiofrequency ablation of liver metastases. Next, the patient undergoes prophylactic adjuvant chemotherapy.
For small cancers that do not threaten complications - obstruction and bleeding, another tactic is possible, when the surgical stage is carried out after several courses of chemotherapy, then the affected part of the colon and metastatic foci are removed simultaneously or at intervals. Postoperative drug therapy is adjusted to a total duration of six months.
When, with multiple metastases, there remains a danger of complete blocking of the lumen of the intestinal tube by cancer, the issue of palliation is resolved with the formation of a colostomy above the tumor conglomerate, which will prevent fatal intestinal obstruction. The patient is prescribed cyclic chemotherapy.
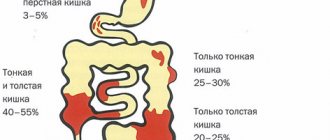
INTESTINAL TUMORS
13.12.12
Diagnosis of the disease
Unlike colon cancer, rectal cancer is diagnosed using simple “routine” methods: characteristic complaints, digital, endoscopic, X-ray examination of the rectum, morphological examination of the material obtained from a tumor biopsy. To identify the prevalence of the process, more complex methods are used, which will be discussed below.
Clinical symptoms of rectal cancer and the degree of their manifestation are determined by the size, degree of invasion, growth pattern and localization of the tumor, as well as associated complications and the nature of metastasis. As the tumor grows and metastasizes, the symptoms of the disease become more varied and their severity increases.
Depending on the pathogenetic mechanism, the following clinical symptoms are distinguished:
- Primary or local – caused by the presence of a tumor in the rectum.
- Secondary – caused by tumor growth, which leads to obstruction and disruption of intestinal function.
- Symptoms caused by tumor growth into neighboring organs, as well as complications and metastasis associated with cancer.
- General – caused by the general effect of cancer on the body.
In the early stages of the development of the tumor process, local symptoms (primary) are most often not expressed sharply, can appear periodically and do not attract the proper attention of the patient and the doctor. The primary symptoms of intestinal cancer are pathological discharge of blood and mucus from the intestine.
Blood in the stool initially appears in the form of streaks. As the tumor grows and becomes injured, the amount of blood released increases. The blood is dark or black (altered), almost always mixed with stool, or precedes stool. In the later stages of the disease, it may become foul-smelling or excrete in the form of blood clots.
Mucus in rectal cancer is very rarely released in its pure form. More typical is the secretion of mucus streaked with blood, often with bloody discharge, or in later stages with an admixture of bloody fluid or pus with a fetid odor.
The presence of blood or, more typically, blood and mucus in the stool is a direct indication for digital examination of the rectum and rectoscopy. The presence of hemorrhoids with bleeding, acute and chronic anal fissure, chronic paraproctitis and other diseases of the perianal region, anal canal and rectum with a similar clinical picture (blood in the stool) in a patient cannot be a contraindication for performing the above diagnostic procedures.
You should always remember the possibility of the simultaneous development of two or more diseases in one person. This approach may make it possible to detect a tumor at an early stage of the disease.
As the tumor grows, local symptoms become more pronounced: the discharge of blood from the rectum increases, clots often appear, but there is no profuse (stream) bleeding. The shape of the bowel movements may change - ribbon-like feces, a feeling of a foreign body in the rectum.
Secondary symptoms appear when the tumor reaches a significant size. They are caused by a narrowing of the lumen of the rectum and rigidity (limited mobility) of the walls; in rare cases, they are the first and only symptoms of the disease. With cancer localized in the upper part of the rectum, symptoms of intestinal obstruction of varying severity, up to complete, predominate. It all starts with a violation of the passage of feces through the intestines: constipation, bloating, rumbling in the stomach, increased peristalsis, in advanced cases accompanied by cramping pain in the abdomen. Often persistent constipation is replaced by periodic diarrhea. The mechanism of this phenomenon is due to the fact that dense feces do not pass through the narrowed lumen of the rectum, which in turn leads to a decrease in water absorption, increased secretory activity and increased peristalsis of the large intestine. With such false diarrhea, the solid part of the feces does not pass through the tumor canal and gradually accumulates in the colon above the tumor. Without treatment, obstructive intestinal obstruction, perforation of the intestine above the tumor due to overdistension and, as a result, fecal peritonitis may develop.
In case of ampullary rectal cancer, complete intestinal obstruction is extremely rare due to the width of the lumen. This localization, along with the symptoms of partial colonic obstruction, is characterized by a feeling of incomplete emptying after defecation, due to the presence of a large tumor in the intestine.
When the tumor significantly narrows the lower part of the rectum, a number of patients experience frequent, up to 15-20 times a day, painful urge to defecate - tenesmus. In this case, either nothing is released from the rectum, or only liquid feces with pathological impurities, and then in small quantities. This tumor, like a foreign body, triggers the defecation reflex, but solid feces do not pass through the narrowed section of the intestine and, despite “stooling up to 20 times a day,” the patient has symptoms of incomplete obstruction.
When a tumor grows into the intestinal wall and into neighboring structures and organs, along with those listed, other symptoms appear. The tumor, located in the lower rectum, can spread to the anus, the prostate gland in men and the vagina in women. In these cases, patients experience pain in the anus, coccyx, sacrum and lumbar region. Men may have difficulty urinating.
With cancer of the upper and middle rectum in men, the tumor can grow into the wall of the bladder. Clinical manifestations in this case occur when a fistula tract forms between the intestine and the bladder. In such patients, due to the development of an ascending urinary tract infection, fever is noted. Gases and feces are released from the urethra during urination. There may be leakage of urine from the rectum. When a rectal tumor grows into the uterus, there are no clinical manifestations. When the posterior wall of the vagina grows, a rectovaginal fistula can form and feces and gases will begin to leak from the vagina.
In the rectum, the tumor is constantly traumatized by feces, which, in turn, leads to the occurrence of inflammation in the tumor itself, spreading to surrounding tissues. In these cases, symptoms characteristic of perifocal inflammation appear, pelvic abscesses, abdominal abscesses, intestinal perforation resulting in peritonitis, as well as fistulas. Symptoms characteristic of the listed pathological conditions in rectal cancer are present simultaneously with the primary symptoms and symptoms caused by narrowing of the rectal lumen. Therefore, these manifestations of cancer are considered complications of rectal cancer .
Metastases of rectal cancer in the liver are common; they do not have characteristic clinical manifestations; only with significant liver damage can one see an enlargement of the organ. If the nodes are localized in the area of the porta hepatis, jaundice may appear. With purulent melting of metastases in the liver, the clinical picture of liver abscess develops.
General symptoms - a violation of the general condition of patients: weight loss, weakness, decreased ability to work, fatigue, anemia, sallow complexion, decreased turgor and dry skin - occur only with a widespread tumor process, but in the initial stages the condition practically does not change.
DIAGNOSIS OF RECTAL CANCER
Unlike colon cancer, rectal tumors can be diagnosed using simple – “routine” – methods: digital, endoscopic, x-ray examination of the rectum.
A digital rectal examination can detect a tumor in 80% of patients. However, more than 80% of newly hospitalized patients are diagnosed with advanced stages of the disease - III - IV. In this regard, the problem of early cancer is one of the most pressing in modern oncology. To be fair, it should be said that the scanty symptoms at the early stage of the disease, its similarity with various diseases of the colon, late patients seeking qualified medical care, as well as the lack of oncological alertness among general practitioners and health education work contribute to the fact that only 30- 40% of patients undergo radical treatment.
Rectal examination - special examination techniques to assess the condition of the rectum and surrounding organs and tissues, performed through the lumen of the rectum.
In clinical practice, digital and instrumental rectal examination (abbr. R.I.) is used. Digital examination is a mandatory method for diagnosing diseases of the rectum, pelvis and abdominal organs. It should always be performed if there are complaints of abdominal pain, dysfunction of the pelvic organs, or intestinal activity. It always precedes the instrumental R.I. and allows you to decide the feasibility of carrying out the latter, to avoid serious complications in the event of a sharp narrowing of the anal canal or rectal lumen by a tumor or inflammatory infiltrate.
Paltsevoye R.I. allows:
- assess the functional state of the anal muscles,
- identify diseases, pathological changes in the anal canal and rectum (cracks, fistulas, hemorrhoids, cicatricial changes and narrowing of the intestinal lumen, benign and malignant neoplasms, foreign bodies);
- determine inflammatory infiltrates, cystic and tumor formations of the tissue surrounding the intestine, sacrum and coccyx;
- detect changes in the prostate gland in men and internal genital organs in women;
- assess the condition of the pelvic peritoneum, rectouterine or rectovesical recess.
Sometimes finger R.I. is the only method for detecting a pathological process localized on the posterior semicircle of the rectal wall above the anal canal, in an area that is difficult to access with any type of instrumental rectal examination.
Paltsevoye R.I. It is contraindicated in case of a sharp narrowing of the anus, as well as in case of severe pain (until the pain is relieved with the help of ointment with dicaine, analgesics or narcotics).
A rectal examination is carried out in various positions of the patient: lying on his side with the legs bent at the hip and knee joints, in the knee-elbow position, in the supine position (on a gynecological chair) with the knees bent and legs brought to the stomach. Sometimes, to assess the condition of the hard-to-reach upper parts of the rectum with digital R.I., the patient is placed in a squatting position. If peritonitis or abscess is suspected, digital R.I. is carried out with the patient in the supine position, because Only under this condition can one identify the symptom of overhang and pain in the anterior semicircle of the rectal wall.
Instrumental rectal examination is carried out using a rectal speculum, anoscope or sigmoidoscope.
Is there a real opportunity today to diagnose cancer at an early stage or prevent it?
If we assume that cancer tumors develop from benign, often asymptomatic, adenomatous polyps, we can assume that removal of such polyps is the only current method of preventing colorectal cancer. Detection of these polyps is possible only with a total colonoscopy, which should be performed for the first time in all practically healthy people when they reach 40-50 years of age. If the first preventive colonoscopy does not reveal pathological changes in the colon, it should be repeated after 3 years, and then after 5 years.
There is another opinion about the possible development of cancerous tumors on the “unchanged” mucosa of the colon (de novo). We can speak with confidence only about obligate precancer - hereditary familial polyposis, although the frequency of this disease is not so high and is unlikely to improve the rates of early diagnosis.
Information about risk factors for colorectal cancer is extensive and sometimes contradictory; however, a number of researchers include such factors as:
- Eating disorders (consumption of high-calorie, fatty foods);
- Alcohol abuse;
- Social status and environment;
- Living conditions;
- Heredity.
The influence of these factors on the occurrence of cancer is only partially confirmed. According to international cancer registries, the incidence of rectal cancer varies significantly in countries with almost identical climatic conditions, diet composition, etc., and there are no significant differences in the incidence of rectal cancer in people with different socioeconomic status, education, etc.
Considering this circumstance, the American Proctological Society in 1999 proposed dividing the entire population into 3 risk groups:
- Low risk group. This includes people over 50 years of age with a family history of colorectal cancer (negative family history). They need a test for occult blood and digital examination annually, as well as fibrocolonoscopy or irrigoscopy every 5 years.
- Medium risk group. People of the same age who have one or more relatives with colon cancer. In this group, screening should begin at age 40 according to the above scheme.
- High risk group. These are patients with familial polyposis, ulcerative colitis or Crohn's disease. These patients require annual colonoscopy starting at 12-14 years of age.
Thus, only regular familiarization of the population with the first signs of rectal cancer, only mass tests for occult blood in the stool and periodic colonoscopy in a group of people at high risk of the disease can reduce the incidence of advanced forms of cancer of this localization and thereby increase the survival of patients.
It is quite obvious that the emergence in the arsenal of medicine of new universal methods for detecting or marking a tumor focus at an early stage will significantly increase the patient’s chances of cure.
Since the mid-70s, an active search has been carried out and put into practice to determine the level of so-called tumor markers in the patient’s blood serum.
The most well-known marker of colon cancer is carcinoembryonic antigen ( CEA ), discovered in 1965. CEA is a glycoprotein located in the peripheral layers of the cell membrane. As a tumor marker it has a number of disadvantages. Firstly, CEA is not detected in 40% of patients with colorectal cancer. Secondly, it has low specificity, since an increase in its level is detected in other malignant tumors and in non-tumor diseases. Thus, CEA has not found application in the primary diagnosis of colorectal cancer. But it can be a marker of the course of the disease: an increase in the level of CEA is observed in advanced stages of the tumor process. A high level of the marker is often detected with liver metastases, less often with local cancer. After radical treatment, the level of CEA in the patient’s blood, as a rule, decreases relative to the initial level or to normal.
Systematic determination of CEA in patients after radical treatment makes it possible to identify relapse. An increase in the level of CEA in the patient's plasma by more than 2 times compared to the initial (postoperative) level or an indicator of -10 ng/ml can be considered an alarm signal and requires an in-depth examination to identify a relapse.
Another widely detected marker, CA-19-9 , has prognostic value in colon cancer. If its level exceeds 37 units/ml, the risk of death within 3 years after surgery increases 4 times compared with those patients in whom this indicator is negative or lower.
Thus, a universal marker that helps detect colorectal cancer at an early stage of the process has not yet been found, but certain successes in this area are encouraging.
The difficulty of early diagnosis of rectal cancer lies in the absence of pathognomonic signs of “early” rectal cancer. Only in those clinical situations when complaints characteristic of advanced cancer appear (tenesmus, constipation, discharge of mucus, blood, etc.) is diagnosis truly simple. Complaints and digital examination of the rectum make it possible to diagnose rectal cancer in more than 2/3 of patients with a high degree of probability. With a digital examination, it is possible to feel the tumor, determine the size along the perimeter of the intestine, sometimes its length, the degree of narrowing of the lumen, mobility, and infiltration of surrounding tissues. A digital examination provides an experienced proctologist with comprehensive information and can determine further treatment tactics. In women, digital examination of the rectum must be supplemented with vaginal examination. This allows you to obtain additional information about the extent of the tumor in the intestine and pelvis.
A digital examination of each patient should be supplemented by rectoscopy. With its help, it is possible to examine a 30 cm long section of the intestine. In addition, obtain material for morphological research.
Morphological confirmation of the diagnosis even with the most characteristic picture of rectal cancer is mandatory.
A biopsy is performed at the end of the study. If the answer is negative, the biopsy must be repeated (up to 3 times).
Using digital examination of the rectum, rectoscopy and morphological examination of biopsy material, it is possible to establish the correct diagnosis of rectal cancer in 80% of patients. However, diagnosis cannot end at the stage of diagnosis verification. It is necessary to get an idea of the extent of the tumor along the intestinal wall, the nature of its growth, possible invasion into neighboring organs and tissues, the presence of distant metastases, and the condition of the entire colon.
Although rectoscopy In addition, synchronous cancer of the rectum and colon is not uncommon, occurring in 1.5–2% of patients, therefore all parts of the large intestine are examined in all patients with rectal cancer. Both colonoscopy and irrigoscopy are suitable for this purpose. These are not competing, but complementary survey methods.
Irrigoscopy (fluoroscopy with filling the intestine with barium using an enema) allows you to assess the length of the tumor, the shape of its growth, identify a second tumor, large polyps, diverticula, and, to a certain extent, judge the growth into surrounding tissues.
When an endoscope can be passed through the "cancer channel", a total colonoscopy . The method allows you to examine all parts of the colon and take biopsy material.
Modern capabilities of computer technology now allow computer reconstruction of the inner surface of the intestine without endoscopic examination. The method is called virtual computed tomography (CT) colonoscopy . The essence of the method is as follows. After appropriate preparation of the patient’s intestines (emptying the lumen of feces) and introducing air into the colon, a spiral computed tomography scan of the abdominal cavity is performed. The obtained data is subjected to computer processing and displayed in the form of a three-dimensional image of the intestinal lumen. The method allows you to detect polyps up to 5 mm in diameter. The disadvantages of virtual colonoscopy are the inability to reproduce the texture and color of altered areas of the mucous membrane, the inability to perform a biopsy, as well as false-positive results due to fecal retention or collapse of a segment of the intestine.
To clarify the prevalence of the tumor process in the pelvis and identify metastases in the lymph nodes, additional research methods are used: transabdominal ultrasound imaging, CT, lymphography, magnetic resonance imaging, laparoscopy.
Transrectal ultrasound is one of the most informative methods for determining the depth of invasion of the intestinal wall and damage to regional lymph nodes. Primary diagnosis of the disease using the transabdominal method is difficult for a number of objective reasons. This is primarily due to the fact that during transabdominal scanning the rectum is visualized only in 85% of cases. The anal canal area is practically inaccessible for research due to the great depth of its location and the imposition of an acoustic shadow from the pubic bone. In addition, the study requires a good filling of the bladder.
The sensitivity of the method in the differential diagnosis of localized and locally advanced tumors is 91%, specificity is 89%.
Of course, transrectal ultrasound tomography cannot be a method of primary diagnosis of rectal cancer. However, this type of introscopy allows solving the most important diagnostic problems:
- assess the extent of the tumor process;
- determine the degree of damage to the intestinal wall;
- determine the depth of infiltration of pararectal tissues;
- identify metastatic lesions of pararectal lymph nodes;
- identify the spread of the tumor process to nearby organs;
- evaluate the effectiveness of preoperative radiation therapy.
To identify metastases in the lungs, chest x-ray in two projections, and, if necessary, x-ray tomography and x-ray computed tomography.
One of the most informative available methods for detecting distant metastases in the liver and lymph nodes is computed tomography . It is used to detect metastases in the liver, porta hepatis larger than 1 cm, and lymph nodes. Computer semiotics and additional contrasting make it possible to distinguish tumor lesions from other focal liver diseases. In addition, the method allows you to perform targeted fine-needle percutaneous puncture of a focal formation and obtain material for cytological examination.
Transabdominal ultrasound tomography has approximately the same information content in detecting liver metastases. With its help, in 80-85% of patients, lesions in the liver up to 1 cm in size can be detected. The method also allows for targeted fine-needle percutaneous puncture of the focal formation.
Detection of micrometastases in regional and distant lymph nodes, determination of subclinical metastases in the liver, dissemination in the abdominal cavity in colorectal cancer are of great importance, both in tactical and prognostic terms. However, the possibilities of preoperative diagnosis of micrometastases are significantly limited.
One of the most sensitive and informative methods for detecting “small” tumors, relapses, and micrometastases is positron emission tomography (PET). PET makes it possible to differentiate metastatic lesions of the lymph nodes from lymphadenopathy of another nature, which cannot be done using computed tomography, and can also be successfully used to determine the extent of the primary tumor. The possibility of using PET to assess the operability of patients with liver metastases is also being studied.
The method is a type of scanning using a radiolabeled glucose derivative. The obtained data is processed using standard computer technology. The finished tomograms are displayed. PET has several advantages over other imaging techniques. The method allows you to differentiate viable tumor tissue from areas of fibrosis, necrosis or scar changes. In addition, it is possible to detect tumor tissue as early as possible, since metabolic activity is diagnosed before structural changes detected by various methods appear.
A comprehensive examination of patients with rectal cancer allows us to clarify the extent of tumor spread, select the optimal treatment method, determine the extent of the operation and evaluate the prognosis.