Characteristics of the disease
Hepatocellular cancer develops as a result of the following previous diseases:
- steatosis;
- long-term inflammation, often viral hepatitis;
- systematic alcohol abuse, which led to liver cirrhosis.
Most often, symptoms of oncology appear in the third or fourth stage . People who carefully monitor their health and well-being are able to detect signs of liver cancer at stage 2.
The last degree of oncology is characterized by a severe form of tumor development, often with metastasis to other organs. Treatment is aimed at alleviating the general condition or reducing pain, less often at combating the tumor.
In most cases, patients with stage 4 liver cancer die within a few years.
There are substages of stage 4 liver cancer:
- IVA - a liver tumor metastasizes to neighboring tissues, and there is a huge number of neoplasms in the organ itself. Lymph nodes and blood vessels are affected.
- IVB – neoplasms affect neighboring and distant organs, which sharply worsens the patient’s well-being.
Degrees (stages) of fibrosis
Liver fibrosis develops gradually over many years and sometimes decades. Its rate is influenced by both the activity of the underlying liver disease and the individual characteristics of the person, as well as the presence of additional damaging factors. To classify fibrosis, special scales can be used and, in particular, the METAVIR scale, which distinguishes five degrees (stages) of liver fibrosis, reflecting the degree of changes occurring and the possibility of reversibility of the processes:
F0 – healthy liver.
F1 - first degree , when excess fibrous tissue is located only around the branches of the hepatic artery and vein, located in special areas called portal tracts, without the formation of partitions (septa). At this stage there are usually no symptoms, and liver enzymes may also be normal. On a survey ultrasound of the liver, changes in its tissues are most often not detected; less often, an increase in the size of the organ is noted - hepatomegaly and the presence of structural heterogeneity (this study cannot determine the stage of fibrosis).
F2 – second degree , in which additional septa are formed from fibrous tissue, isolating the main liver cells (hepatocytes) from the blood entering the liver. This disrupts the process of blood purification by hepatocytes and prevents the entry of substances that these cells produce into the blood. In places where septa are formed, blood bypasses the liver cells and is discharged from the afferent vessels into the hepatic veins. In most cases, there are no symptoms at this stage either. Liver enzymes and inflammatory markers increase; liver ultrasound in all patients shows an increase in the size of the organ and the presence of structural heterogeneity.
F3 – the third degree occurs 6-8 or more years from the onset of the disease. The number of septa and fibrous tissue in the portal tracts increases significantly. Usually at this stage the first symptoms appear - weakness, drowsiness, fatigue, bruises on the skin and others. Liver enzymes increase, hemoglobin and platelet levels decrease, inflammatory markers increase, and on liver ultrasound, the presence of denser areas is added to liver enlargement and diffuse changes. Up to the third stage, fibrotic changes in the liver can be reversible with complete cure of the disease that caused them.
F4 – liver cirrhosis , at this stage there is an irreversible replacement of liver tissue with fibrous, connective tissue. Read more about liver cirrhosis.
Signs and symptoms
Blood circulates in the liver in a special way, which exposes the organ to metastasis most often. The most common signs of stage 4 liver cancer are as follows:
- Pain and heaviness from the organ.
- Itching and rash on the body.
- Pallor of the skin.
- The thermometer consistently shows 38 °C.
- Development of jaundice.
- A sharp drop in body weight.
- Heaviness and pain in the stomach, disturbances in stool and gastrointestinal function, and often nausea.
Depending on the extent of growth in the tumor organ, other signs may appear:
- Darkening of urine, lightening of stool, appearance of a green tint to the skin.
- The development of cholestasis as a result of compression of the bile ducts by large neoplasms.
- Increased bilirubin and development of jaundice against this background.
- Decreased libido and menstrual irregularities in women.
- Deformation and varicose veins of the esophagus, which can cause bleeding. Develops due to increased pressure in the liver.
- The appearance of vascular networks and hematomas on the skin.
- The appearance of internal and nasal bleeding as a reaction to the reduced ability of blood to clot. This occurs due to disturbances in protein metabolism and liver failure.
Secondary symptoms that occur as a result of advanced liver cancer may include:
- itching of the skin, development of pleurisy, accumulation of a large amount of fluid inside the abdominal cavity;
- severe pain and discomfort not only in the liver area, but also in the abdomen and lower back;
- discomfort, weakness and pain cause a sharp decrease in appetite, apathy and a drop in physical activity.
Diet for liver fibrosis
The composition of food is important for the liver; excess or lack of nutrients negatively affects its condition. The liver is involved in protein metabolism, so it is important to include protein products of plant and animal origin in the diet in equal shares to ensure the required intake of 80-90 grams of protein per day. It is useful to consume foods that prevent the accumulation of fat in the liver - cottage cheese, cheese, egg whites, cod, oatmeal and others. Limiting animal proteins in the diet and replacing them with plant proteins is recommended at the stage of cirrhosis and when the condition worsens.
In most cases, it is also not necessary to limit fats below normal (80-90 grams), except for the stage of liver cirrhosis, when fats are limited to 50-60 grams. Products containing hard-to-digest refractory fats are prohibited: lamb, fatty pork, geese and duck meat.
Excessive consumption of refined sugar and products containing it is harmful to the liver. The daily intake of carbohydrates is limited to 350-400 grams, where the proportion of simple sugars should not exceed 70 grams. Among foods containing carbohydrates, it is recommended to give preference to foods rich in plant fiber: vegetables, fruits, whole grain bread and pasta.
The amount of fluid consumed is limited only in people with cirrhosis of the liver, but salt intake, regardless of the degree of fibrosis, is recommended to be reduced to 8-10 grams, and in the presence of edema to 3-4 grams.
It is also important to eat regularly 4-5 times a day at approximately the same time and avoid late, heavy dinners.
List of recommended products:
Wheat, whole grain, dried rye bread, biscuits, baked goods made from soft dough.
Soups with the addition of vegetables, cereals, pasta in vegetable broth or milk, borscht, beetroot soup, cabbage soup made from fresh cabbage, flour and vegetables are added to the soup without frying.
Dishes of lean meat and poultry (beef, veal, turkey, chicken) boiled, baked, or stewed, steamed.
Dishes from low-fat fish (cod, pike perch, perch, navaga, carp, pike) boiled or baked.
Butter (30-40 g) and vegetable oil (20-30 g): olive, sunflower or corn (added to ready-made dishes in their natural form without cooking).
Various types of boiled and baked vegetables, onions are added only after scalding with boiling water. Also fresh vegetables, especially if you are prone to constipation.
Porridge, especially oatmeal and buckwheat, casseroles from cereals and pasta with the addition of cottage cheese.
No more than 1 egg per day (if well tolerated) or 2 whites to prepare a protein omelet.
Dairy, sour cream sauces with vegetable broth, fruit and berry sauces. Flour for sauces is not sautéed with butter.
Any fruits and berries, except very sour varieties (lemon with sugar is fine). Compotes, purees, and jelly are recommended.
Milk and dairy products - whole, natural milk (if well tolerated), low-fat fresh cottage cheese and cheese, curdled milk, kefir, acidophilus milk; sour cream is added to dishes as a seasoning.
Products to exclude:
- fatty meat and poultry;
- products with added trans fats (solid vegetable oils);
- fried, smoked, pickled and overly salted foods;
- excessively fatty fish;
- sweet pastries, cakes with cream;
- fatty dairy products;
- hot spices, raw garlic and onions;
- carbonated drinks;
- strong meat broths;
- canned food
Alcohol use in liver fibrosis
Alcohol can cause additional liver damage, so if you have chronic liver disease or fibrotic changes, complete abstinence from alcohol is recommended.
Symptoms of imminent death
Just before death, the patient exhibits other signs indicating the body’s inability to fight the tumor, namely:
- Unstable body temperature and decreased blood pressure.
- Impaired urination function, which is accompanied by swelling of tissues and limbs, a sharp decrease in the daily norm of discharge.
- The development of venous spots on the legs indicates disruptions in the circulatory system. The appearance of such marks on the feet indicates imminent death.
- Due to a decrease in blood flow to the organs, the limbs become cold and acquire a bluish tint.
- Shortness of breath appears and breathing worsens. Patients experience difficulty coughing and produce characteristic wheezing due to swelling of the lungs.
- The emotional and mental state is disturbed: quiet, slow, unintelligible speech, apathy, severe lethargy.
- If the condition is accompanied by dysfunction of certain areas of the brain, patients often forget, do not recognize their relatives, experience disorientation and hallucinations.
- Mobility is clearly reduced to the point of inability to move independently.
- Complete lack of appetite due to various unpleasant sensations in the digestive system. In some cases, even water can cause painful reactions.
- Drowsiness is more pronounced against the background of the previous days. The development of this condition occurs as a result of dehydration and exhaustion of the body.
In medicine, there are 4 stages of human death:
- Predagonia is accompanied by a rapid drop in blood pressure, the skin becoming bluish, and deterioration of emotional and physical capabilities.
- Agony – characterized by a lack of oxygen, which leads to difficulty breathing and stopping it. There is a significant slowdown in blood circulation for no more than 3 hours.
- Clinical death - all metabolic processes deteriorate to critical levels, which provokes the cessation of many body functions.
- Biological death - cessation of brain function, death.
All of the listed stages of death are typical for both stage 4 cancer and other cancers.
Treatment
To date, there is no method or panacea for stage 4 liver cancer. However, the most modern methods can slow down the development of the tumor and significantly alleviate the patient’s condition. Among the advanced therapeutic technologies are the following:
- Chemotherapy – with the help of the drugs “Nexavar” and “Sorafenib”, chemically active substances are introduced into the patient’s body, which has a detrimental effect on tumor cells.
Important! The use of drugs to treat other types of oncology to combat liver cancer has no effectiveness. - Radiation therapy – is performed using X-rays, which reduce the intensity of pain experienced by the patient, reduce the size of the tumor, which increases life expectancy.
- Vascular embolization – reducing the access of blood to them helps stop the growth of cancer cells. This is achieved by blocking the liver vessels with special substances. It is used for neoplasms with a tumor diameter of up to 5 cm.
- Ambilation is the introduction of ethyl alcohol into the area of a cancerous tumor. This substance destroys the tumor if its size is up to 3 cm.
Methods for diagnosing liver fibrosis
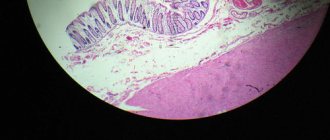
For diagnosis, a puncture biopsy of the liver with histological examination of the resulting sample can be used. It is considered the “gold standard”, but has limitations and disadvantages:
- is an invasive method that can cause complications;
- it is risky to use for dynamic observation and monitoring of treatment results;
- the amount of material obtained from a puncture biopsy is limited and can accurately reflect only the condition of the part of the liver from which it was taken (the liver with fibrosis is heterogeneous);
- sampling errors are possible;
- lack of qualified morphologists conducting histological examinations.
There are also non-invasive methods - laboratory panels of tests, for example, FibroMax and shear wave ultrasound elastography of the liver, which, when combined according to the latest clinical guidelines of the European Society for the Study of the Liver, give a result closest to that obtained with a liver biopsy.
These are more accessible and non-traumatic methods that have sufficient sensitivity and specificity and can be used repeatedly to assess the degree of liver fibrosis at various stages of its progression.
Measures to alleviate the condition
The last stage of liver cancer is often near death and is accompanied by emotional, psychological and physical suffering for the patient. Relatives can help the patient using the following measures:
- Develop a menu and make sure your meals are correct. The patient's diet should include purees, cereals, pureed foods, and liquid dishes. If a regular spoon is not suitable, you can use a probe.
- Constantly feed the patient, wetting the lips if necessary. This will prevent dehydration, improving your breathing.
- To prevent the appearance of bedsores, use talcum powder, wipe the patient's body dry after regular washing, turn over on the bed, knead the back and buttocks.
- If bedsores, ulcers or redness do appear, then Desitin and camphor alcohol are used to combat them.
- Several pillows or an elevated head of the bed will make breathing easier for the patient.
- Communicate with the patient more often, reassure him, and encourage him. In moments of delirium or hallucinations, react adequately, excluding conflicts and quarrels.
- Choose the right painkillers and change them as their effect decreases.
- Give sedatives for excessive agitation, outbursts of aggression, and convulsions.
- Perform breathing exercises to prevent pneumonia.
What does cancer survival depend on?
Let's summarize:
- Cancer is curable, but only with timely detection of pathology and rational treatment.
- In the early stages, it is easier to cope with the disease than if the process spreads significantly and metastases appear.
- The prognosis depends not only on the stage, but also on the type of tumor. Well-differentiated carcinoma is easier to treat than aggressive, low-grade tumors.
- Successful treatment of cancer requires a comprehensive approach: surgery, chemotherapy and radiation.
- The final prognosis of the disease is determined after examination, as well as during treatment.
Prognosis: how long to live at this level?
Predicting life expectancy for a given patient with stage 4 liver cancer is not always easy. Life expectancy is influenced by many factors:
- age - in old people, blood clotting, immune functions of the body and cell regeneration and other features are much weaker than in young patients;
- a history of other diseases - many diseases accelerate the course of cancer, aggravating the general condition of the patient;
- type and nature of treatment measures - without the use of any means and methods of therapy, patients live no more than 1-1.5 years;
- lifestyle – introducing a diet, giving up bad habits and alcohol and other factors increase the patient’s life expectancy.
In general, active therapy can prolong the life of a patient with stage 4 liver cancer by up to 5 years.
Is it possible to cure cancer with metastases?
Liver cancer at stage 4 is considered an incurable disease, which is characterized by the difficulty of achieving a long period of remission. If you follow the doctor’s instructions and follow the treatment regimen he has developed, you can significantly prolong your life. In practice, such patients can often live up to 5 years .
The prognosis is influenced by the individual characteristics and lifestyle of the patient. The presence of metastases and the rate of their progression play an important role in the formation of secondary neoplasms in neighboring organs. In addition to the liver, the tumor can grow into:
- rectum;
- stomach;
- prostate;
- gallbladder;
- ovaries;
- lungs;
- kidneys
With rapid tumor spread in patients with stage 4 liver cancer, even treatment cannot delay death. The maximum for these patients is only 1-2 years. Due to the ability of the disease to develop from the initial to the final stages in a matter of months, oncologists predict only 6% of patients will live for another 5 years.
Stage 4 liver cancer is a very dangerous and incurable disease . Treatment using various methods, including folk remedies, will not get rid of the disease, but can significantly improve the patient’s condition. Proper care will help make the last days or months of your loved ones' lives more comfortable.
Tumor pleurisy (differential diagnosis and treatment)
The history of the doctrine of pleurisy goes back many centuries. In the 18th century some clinicians tried to distinguish pleurisy into an independent nosological form. For decades, the etiology, pathogenesis of pleurisy and the most appropriate methods of their treatment have been studied. Effusion in the pleural cavity should not be considered an independent disease, since it is only a peculiar manifestation of various common diseases: tumors, pneumonia, allergic conditions, tuberculosis, syphilis, heart failure, etc. (Table 1). Accumulation of fluid in the pleural cavity, caused by heart failure and pneumonia, occurs 2 times more often than with malignant tumors [4].
| The mechanism of formation of pleural effusion in malignant neoplasms: |
| Direct effect of the tumor 1. Metastases to the pleura (increased permeability of the capillaries of the pleura) 2. Metastases to the pleura (obstruction of the lymph nodes) 3. Damage to the lymph nodes of the mediastinum (reduced lymphatic outflow from the pleura). 4. Obstruction of the thoracic duct (chylothorax). 5. Obstruction of the bronchus (decreased intrapleural pressure). 6. Tumor pericarditis. Indirect influence of the tumor 1. Hypoproteinemia. 2. Tumor pneumonia. 3. Pulmonary embolism. 4. Condition after radiation therapy. |
Pleural effusion can be a transudate or an exudate. The cause of transudate formation is usually congestive heart failure, mainly in patients with left ventricular failure and pericarditis. With the accumulation of transudate (hydrothorax), the pleura is not involved in the primary pathological process. Hydrothorax
is observed in cases where systemic or pulmonary capillary or plasma oncotic pressure changes (left ventricular failure, liver cirrhosis).
Pleurisy
(accumulation of exudate in the pleural cavity) most often occurs in patients with malignant neoplasms.
The most common cause of exudative pleurisy is metastasis to the pleura and lymph nodes. Pleural effusion from tumors has a complex origin: fluid accumulation is caused by an increase in capillary permeability due to inflammation or rupture of the endothelium, as well as deterioration of lymphatic drainage due to obstruction of the lymphatic pathways by the tumor and tumor growth into the pleura. The accumulation of effusion in cancer patients may be facilitated by poor nutrition and decreased protein levels in the blood serum [1–4]. ALGORITHM FOR TREATMENT OF TUMOR PLEURITIS
Scheme
Tumor (metastatic) pleurisy is a common complication of lung cancer
,
breast, ovaries
, as well as for
lymphomas and leukemia
. Thus, in lung cancer it occurs in 24–50% of patients, in breast cancer – up to 48%, in lymphomas – up to 26%, and in ovarian cancer – up to 10%. In other malignant tumors, tumor pleurisy is detected in 1–6% of patients (cancer of the stomach, colon, pancreas, sarcoma, melanoma, etc.). The most common cause of exudative pleurisy is metastasis to the pleura and mediastinal lymph nodes. Pleurisy, as a rule, indicates an advanced tumor process and is a consequence of tumor rashes in the pleura.
Diagnostics
Cytological examination of pleural fluid
for tumor cells (erythrolyte content more than 1 million/mm3) is an important diagnostic method.
Obtaining hemorrhagic exudate during pleural puncture with a high degree of probability indicates the tumor etiology of the effusion. The detection rate of tumor cells reaches 80–70%. Based on cytological examination of pleural fluid, it is often possible to determine the morphological type of the primary tumor. Table 1. Frequency of effusions of various etiologies (R. Light, 1986) [1]
| Diseases | Frequency of effusions, % |
| Heart failure | 37 |
| Bacterial and viral infections | 30 |
| Malignant tumors | 15 |
| Pulmonary embolism | 11 |
| Diseases of the gastrointestinal tract (liver cirrhosis, pancreatitis, subphrenic abscess, etc.) | 6 |
| Mesothelioma | 0,5 |
| Vascular collagenoses | 0,3 |
| Tuberculosis | 0,2 |
The accumulation of fluid in the pleural cavity leads to compression of the lung, displacement of the mediastinum, which in turn causes increased shortness of breath, disruption of respiratory and cardiac activity. Often pleurisy, being the only manifestation of the tumor process, can be the cause of death of the patient.
Treatment
Treatment of patients with effusion into the pleural cavity consists primarily of fluid evacuation and intrapleural administration of drugs
in order to stop the accumulation of fluid in the pleural cavity and the resorption of exudate.
This leads to an improvement in the patient’s condition, a decrease in shortness of breath, pain, pulmonary heart failure and thereby prolongation of life. The algorithm for diagnosis and treatment of tumor pleurisy is presented in the diagram. Before deciding on the intrapleural administration of certain drugs, it is necessary to clarify the localization of the primary process, since in case of breast cancer, ovarian cancer, small cell lung cancer, and lymphomas, systemic chemotherapy can lead to the elimination of pleural effusion in 30–60% of patients. Table 2. Drugs used for pleurodesis (summary data)
| Class | A drug | Doses |
| Cytostatics | 1. Embikhin | 10-30 mg |
| 2. Thiophosphamide | 30-50 mg | |
| 3. 5-fluorouracil | 750-1000 mg | |
| 4. Adriamycin | 30 mg | |
| 5. Cisplatin | 50 mg | |
| 6. Vepesid | 200 mg | |
| 7. Bleomycin | 15-30 mg | |
| Radioisotopes | 1. Au-198 | 50-100 mCu |
| 2. Phosphorus-32 | ||
| 3. Chrome | ||
| 4. Yttrium-90 | ||
| Immunomodulators | 1. Corinbacterium parvum | 7 mg |
| 2. Interleukin + LAK cells | 500 thousand IU + 10 million cells | |
| Preparations of nonspecific sclerosing action | 1. Talc | 2–4 g |
| 2. Quinacrine | 100 mg | |
| 3. Tetracycline | 1.2-1.6 g |
In cases where systemic chemotherapy is not indicated or has been ineffective, intrapleural administration of drugs is necessary
.
Indications for pleural puncture and intrapleural administration of drugs are the presence of effusion in the pleural cavity above the level of the 2nd–3rd rib in front, severe shortness of breath with symptoms of pulmonary or pulmonary-heart failure, with a life expectancy of more than 2 weeks. If there is effusion without clinical symptoms, there is no point in performing pleural punctures and administering certain medications. Thus, the following indications for pleurodesis
: 1. The presence of subjective symptoms of pleurisy (severe shortness of breath, pain, cough). 2. The presence of effusion, refractory to modern chemotherapy and hormonal therapy. 3. Presence of bronchial obstruction. In table Figure 2 presents the drugs currently used for pleurodesis. Method of administration of cytostatics, their single and total doses, as well as treatment regimen:
| 1. Embiquin 10–30 mg once every 7–14 days, 3–4 injections, total 40–120 mg. 2. Thiophosphamide 30–40 mg once every 7–14 days, 3–4 injections, total 120–160 mg. 3. Fluorouracil 500–1000 mg once every 7 days, 3–4 injections, total 2000–3000 mg. 4. Bleomycin 15–30 mg once every 7 days, 4–5 injections, total 60–150 mg. 5. Adriamycin 30–40 mg once every 7 days, 3–4 injections, total 90–120 mg. 6. Cisplatin 50–60 mg once every 7 days, 2–3 injections, total 100–180 mg. 7. Mitoxantrone (novantrone) 20–25 mg, 2–3 injections. 8. Vepesid 100–150 mg 2 times every 7 days, 3–4 administrations, total 600 mg. 9. Thiophosphamide 30 – 40 mg + fluorouracil 500 mg once every 7 days, 3 injections. |
The effectiveness of intrapleural administration of individual cytostatics for lung and breast cancer ranges from 60 to 80%. In table 3 presents data from the Russian Cancer Research Center named after. N.N. Blokhin of the Russian Academy of Medical Sciences on the effectiveness of chemotherapy for tumor pleurisy [5]. Methods of nonspecific therapy using various sclerosing agents
means for obtaining chemical serositis, gluing pleural layers and thus eliminating effusion in the pleural cavity.
These substances include talc, quinacrine (akrikhin), delagil and tetracycline. The effectiveness of administering talc, quinine, delagil reaches 55–60%, and tetracycline – 80–70% [6–10]. Method of administration of tetracycline.
Tetracycline hydrochloride is most effective in large doses (20 mg/kg or 1200–1600 mg - 12–16 100 mg ampoules).
The patient's pleural cavity is punctured under local anesthesia with the insertion of a thin silicone tube through which the fluid is evacuated using a vacuum suction. After this, the tube is clamped and under X-ray control it is ensured that the lung has expanded. If the lung has not expanded or there is a shift of the mediastinum towards the pleural effusion, tetracycline should not be administered due to the possibility of formation of a truncal lung. Since the administration of tetracycline may be accompanied by pain, it is first diluted in 50 ml of a 0.5% novocaine solution and then injected into the drainage tube. The latter is pressed for 2 hours, and the patient is asked to change his body position several times. After 2 hours, the clamp is removed, and the drainage tube is connected to a vacuum suction with constant pressure (from 15 to 20 cm of water column). Aspiration is continued for at least 24 hours until the volume of fluid removed is less than 150–200 ml per day. After this, the drainage tube is removed. Table 3. Efficacy of chemotherapy for tumor pleurisy (data from the Russian Cancer Research Center)
| Process localization | Number of patients | Complete remissions, % | Partial remissions, % | No effect,% |
| Mammary cancer | 62 | 39 | 39 | 22 |
| Lung cancer | 77 | 45 | 34 | 21 |
| Pleural mesothelioma | 79 | 33 | 33 | 33 |
| Other tumors | 12 | 50 | 33 | 17 |
| Total | 16 | 40 | 35 | 25 |
The procedure is considered successful if the patient develops acute pleurisy
, and with the help of drainage, the rapprochement of the visceral and pariental pleura was ensured and this achieved
obliteration of the pleural cavity
. The failures of this technique are mainly associated with insufficiently complete drainage of the pleural cavity. This technique for draining the pleural cavity can also be used for administering cytostatics. A meta-analysis by S. Belani et al. [11] on the effectiveness of individual drugs in various studies showed that the most effective drugs are tetracycline, talc and bleomycin.
Conclusion
Effusion in the pleural cavity is a fairly common complication of lung cancer, breast cancer and other malignant processes; its manifestation often complicates the problems of treating cancer patients. Many patients with tumor pleurisy live, hoping for a cure, for months and even years. Therefore, effective palliative therapy for tumor pleurisy is an important aspect of the treatment of patients with advanced malignancy to improve their quality of life. For intrapleural administration, both individual cytostatics (bleomycin, cisplatin, etc.) and drugs with nonspecific sclerosing action (tetracycline, talc, etc.) can be used.
Literature:
1. Light R.U. Diseases of the pleura. M., 1986. 2. Hausher FH, Yarbo JW. Diagnosis and treatment of malignant pleural effusion. Cancer Met Rev 1987;6(1):24–30. 3. Leff A, Hopewell PC, Costello J. Pleural effusion from malignancy. Ann Int Med 1978;88:532–7. 4. Sahn SA. Malignant pleural effusion. Clin Chest Med 1985;6:113–25. 5. Kashikova Kh.Sh. Drug therapy of tumor pleurisy. Diss. Ph.D. honey. Sci. M., 1989. 6. Gravelyn TR et al. Tetracycline pleurodesis for malignant pleural effusion: a 10C year retrospective study. Cancer 1987;59(11):1973–7. 7. Kefford RF, Woods RL, Fox R, et al. Intracavitary adriamycin, nitrogen mustard and tetracycline in the control of malignant effusions. Med J Austral 1980;2:447–8. 8. Zoloznik AJ, Oswald SG, Langin M. Intrapleural tetracycline in malignant pleural effusion: Cancer 1983;51:752–5. 9. Bayly TC, Kisher DL, Sybert A, et al. Tetracycline and quinacrine in the control of malignant pleural effusions. Cancer 1978;41:1188–92. 10. Wallach HW. Intrapleural tetracycline for malignant pleural effusions. Chest 1975;68:510–2. 11. Belani CP, Einardson TR, Arikian SR et al. Cost effectiveness analysis of pleurodesis in the management of malignant pleural effusion. J Oncol Management 1995;1(2):24.