Pancreatitis is a severe inflammatory process in the pancreas. This pathological condition affects the organs of the digestive tract, in addition, serious problems arise with the condition and functions of all organs and systems of the human body. Death from pancreatitis, unfortunately, often occurs, especially in the acute course of the disease, and also if severe complications develop, disruption of the vital functions of the body.
Pancreatitis: probable mortality from the disease
Mortality due to inflammation of the pancreas accounts for 40 percent of all cases of acute inflammation of the pancreas. These are very high numbers, indicating the danger of this pathology, the need for timely diagnosis, treatment and prevention of pancreatitis.
Patients die due to severe acute inflammatory pathology or exacerbation of a chronic inflammatory process, with the development of severe complications:
- pancreatic necrosis,
- internal bleeding, especially in the case of its severe complication - hypovolemic shock,
- acute intoxication with decay products as a cause of infectious-toxic shock, more often relevant in pancreatitis of alcoholic origin,
- abscesses, ulcers on the surface of the pancreas or nearby organs (omentum, liver, gall bladder, stomach), purulent inflammatory process in the ducts of the gland, when ruptured or spread, a serious condition develops - peritonitis,
- pain shock,
- pancreatic cancer due to long-term chronic pancreatitis.
If you do not seek medical help in time, do not diagnose these serious conditions in a timely manner and do not begin to treat the patient correctly, then the risk of death is very high.
Signs of severe pancreatitis
Inflammation of the pancreas manifests itself in a variety of symptoms that significantly worsen the patient’s condition and reduce his quality of life, judging by their reviews. Diagnosis of the disease is often difficult due to the similarity of the symptoms of pancreatitis with other gastrointestinal pathologies, especially in children who cannot make complaints on their own. The main signs of severe complicated inflammation:
- Severe abdominal pain of different localization: in the peri-umbilical, hypochondrium region on the left or on both sides. Often the pain is girdling in nature, radiating to the lower back, right and left shoulder, and chest. The pain syndrome during an attack of pancreatitis can be so intense that it can lead to painful shock with impaired consciousness and the development of fatal multiple organ failure.
- Dyspeptic syndrome, manifested by several signs: nausea, vomiting, which does not bring relief, increased gas formation in the intestines, bloating, stool disturbances (more often in the form of diarrhea). Severe dyspepsia with prolonged profuse vomiting and diarrhea leads to dehydration of the patient and loss of essential microelements and vitamins. This is especially common when infusion therapy is insufficient or untimely. Dehydration of body tissues, lack of minerals (magnesium, potassium, calcium, iron and others) negatively affects the functioning of all organs and systems (especially the heart and blood vessels), and in severe cases it is life-threatening.
- General intoxication syndrome, manifested by many severe symptoms, indicating damage to all systems of the human body. The main signs of intoxication: increased body temperature, weakness, decreased blood pressure to the point of collapse, shortness of breath, changes (pallor, cyanosis, icterus) in skin color, headaches, dizziness, impaired consciousness and many others.
- Deterioration of laboratory and instrumental research data in the case of severe inflammation of the pancreas. The CBC reveals pronounced leukocytosis with pathological changes in the leukocyte formula, a sharp increase in ESR due to inflammation. Due to liver damage or the development of internal bleeding, anemia and thrombocytopenia may develop. According to the results of a biochemical blood test, the level of liver enzymes, amylase and other indicators indicating damage to the pancreas increases. When performing an ultrasound, CT scan of intra-abdominal organs, signs of edema, destruction of gland tissue, abscesses and other pathological changes are revealed.
Dangerous symptoms: when to call an ambulance
Death from acute pancreatitis becomes a real threat if a person does not pay attention to the warning signs of the disease. The signs are similar to those of other gastrointestinal diseases, so it is important to differentiate them and carry out timely diagnosis in a hospital setting. Acute pancreatitis is recognized by the following symptoms:
- sharp girdle pain in the stomach and under the shoulder blades, radiating to the shoulders,
- temperature increase (with infection) or decrease (with pancreatic swelling),
- bluish or yellowish coloration of the skin,
- frequent vomiting, which does not bring relief, with bile, pieces of undigested food,
- nausea that occurs even when drinking water,
- palpation of the abdomen - severe pain,
- dark circles under the eyes, sharpened facial features,
- decreased blood pressure (blood pressure),
- coating on the tongue,
- increased heart rate,
- weakness, disorientation, lack of interest in what is happening.
With acute pancreatitis, painful attacks cannot be avoided - complications manifest themselves in the form of damage to neighboring organs and tissues. Pancreatic juice is an aggressive environment that thins and makes the walls of the pancreas and intestines loose, through which pathogenic microbes enter the peritoneal region, enter the bloodstream and spread throughout the body. In this case, sepsis cannot be avoided. The patient's condition worsens before our eyes and can lead to collapse (acute heart failure), loss of consciousness and death.
Severe pain sometimes cannot be dealt with before the ambulance arrives even with the help of strong painkillers. It is not possible to reduce the high body temperature; vomiting invariably follows after eating. When the ducts are clogged, the organ parenchyma looks like a battlefield: ulcerated lesions, purulent formations, clots of coagulated blood. As a result of a severe course of the disease, not only does the pancreas completely fail, but the functioning of the liver, kidneys, stomach, and intestinal tract is also disrupted.
Types of pancreatitis in which an acute course of pathology is possible:
- hemorrhagic (vascular damage),
- purulent (foci of inflammation),
- mixed.
People who suffer from cholelithiasis and abuse alcohol are primarily at risk of developing alarming symptoms. The body can tolerate a one-time powerful intoxication that occurs after taking a large dose of alcohol without serious consequences. But the systematic consumption of strong drinks necessarily leads to irreversible changes in the tissues of internal organs involved in the processing and neutralization of decay products.
This type of pancreatitis is called alcoholic. Unfortunately, the number of people suffering from it is growing rapidly. It all starts with cocktails, beer, wine and ends with severe mental and physical illness, and then premature death.
Death from acute inflammation: how to prevent tragedy?
Acute pancreatitis develops most often due to alcohol abuse and fatty foods. It is very difficult and often leads to life-threatening complications.
Mortality statistics from acute pancreatitis state that 20% of patients with this diagnosis may die, especially in the absence of proper timely therapy.
In order to avoid tragedy, it is necessary to make a timely correct diagnosis and choose the right treatment tactics: surgical intervention according to indications or conservative treatment in the intensive care unit.
Early diagnosis
If a person is diagnosed with chronic pancreatitis, he is familiar with the symptoms of exacerbation and the need for urgent hospitalization in a hospital. With the development of acute pancreatitis, the condition can be underestimated. The slightest delay in medical care can lead to irreparable consequences (disability or death of the patient). Therefore, if you develop any digestive problems, acute abdominal pain, especially against the background of fever, or a deterioration in your general condition, you must consult a specialist or call an ambulance.
To establish a diagnosis, a doctor (gastroenterologist, therapist or surgeon) will conduct a survey to clarify the medical history of the disease, identify risk factors for the disease, and bad habits. Then the specialist will examine the patient and examine him using physical methods: palpation, percussion, auscultation.
To identify an acute inflammatory process, it is necessary to conduct a laboratory examination (CBC, OAM, biochemical blood test, coprological study). Instrumental methods for diagnosing pancreatic pathology will require ultrasound, CT or MRI, and x-ray examination of the digestive organs.
Prevention of pancreatic inflammation
To prevent the development of acute pancreatitis (primary prevention), as well as to prevent exacerbations of chronic inflammation of the pancreas (secondary prevention), all people are recommended to follow certain rules:
- Proper nutrition based on the principles of mechanical, chemical and temperature sparing of the mucous membranes of the digestive tract. Fatty, fried, salty, spicy, and sour foods are excluded. The temperature of food and drinks is within body temperature. Dishes are served to the patient in liquid, puree, or mushy form to facilitate digestion.
- Categorical refusal of bad habits (alcohol abuse, smoking) is one of the most important rules for disease prevention.
- Maintaining a healthy lifestyle, playing sports (specially selected gymnastics), frequent walks in the fresh air.
- Compliance with the work and rest regime, exclusion of heavy physical activity and stressful situations. Sleep should be at least 8 hours a day.
- Timely diagnosis and treatment of other gastrointestinal diseases. Gallstone disease, chronic cholecystitis, any pathology of the biliary system, gastritis, duodenitis are especially important for the development of pancreatitis. Taking prescribed medications in tablets or parenterally to treat concomitant pathologies is extremely important for the prevention of pancreatitis.
Main causes of death from pancreatitis
Mortality due to inflammation of the gland depends on its type (etiology, pathogenesis, symptoms of the inflammatory process).
Alcoholic pancreatitis
Among those who died from alcoholic pancreatitis, many were young; this diagnosis was especially often given to men, since they are the ones who most often suffer from alcoholism.
Regular consumption of ethanol leads to toxic damage to the cells of parenchymal organs - liver, pancreas.
Alcoholic pancreatitis is characterized by the development of necrosis of the pancreas and disruption of its functions.
Acute pancreatitis
The statistics of death from acute pancreatitis with severe symptoms is considered the highest. Death occurs within the first week from the onset of the disease, sometimes even with timely initiation of therapy. The main conditions in which a patient dies due to acute pancreatitis are considered to be massive necrosis of the pancreas and internal bleeding.
Chronic pancreatitis
A long-term chronic inflammatory process in the pancreas is considered not as dangerous as an acute one. But, due to the inevitable damage to the organ during exacerbations, it is impossible to completely exclude the development of severe complications. In addition to death, during an exacerbation of the disease, death is also possible due to the development of a malignant tumor in the pancreas and the progression of cancer to stage 3-4, which cannot be cured.
Hemorrhagic pancreatitis
Inflammation of the pancreas, accompanied by bleeding, is a very dangerous pathological condition. It develops when the wall of a vessel is damaged due to the possible influence of pancreatic enzymes on it.
If internal bleeding (especially from a large artery) is not diagnosed in time and abdominal surgery is not performed, blood loss can quickly become massive, hemorrhagic shock will develop, and the patient will die.
Pancreatic necrosis
Necrosis (destruction) of pancreatic tissue occurs for various reasons. Most often this happens due to acute destructive pancreatitis that develops after abuse of alcohol or junk food. Due to inflammation, swelling of the gland or the presence of stones in the excretory ducts, their lumen decreases, and pancreatic juice, aggressive to any tissue, remains inside the pancreas itself. Proteolytic enzymes destroy the gland and adjacent organs.
With the lightning-fast course of pancreatic necrosis and untimely provision of assistance to the patient, death is almost inevitable.
Death after pancreatic resection
For the formation of abscesses, ulcers, fistulas, and the development of pancreatic necrosis, surgical intervention is considered the only effective treatment. The operation is performed in several ways. The volume of intervention depends on the degree of damage to the pancreas: excision of necrotic tissue, resection of one section or (less often) the entire organ. But even after successful surgical treatment, death is also possible for several reasons:
- Postoperative bleeding.
- Reactive postoperative pancreatitis.
- Infectious complications and postoperative peritonitis.
- Diabetes mellitus, its complications (hyperglycemic coma and others) due to incorrectly selected insulin replacement therapy or the patient’s failure to comply with the recommendations of the attending physician.
Is it possible to die from pancreatitis (pancreatic necrosis)
The pancreas is a small organ, but it performs and plays a huge role in all processes of the body. The shape of the pancreas resembles a willow leaf. It performs two important functions: it participates in the digestion of food and produces important hormones insulin and glucagon, without which not a single process occurs in the body.
Patients often do not understand how serious the pathological processes in this organ are, and whether they die from pancreatitis so often as to attach importance to this. In the last decade, modern medicine has recorded an increase in the statistics of deaths from pancreatitis, namely, from the acute course, death occurs in about 40% of patients.
A fatal outcome from pancreatitis can occur with equal probability in both men and women, since both sexes have poor nutritional balance and bad habits.
In our “fast food time,” this disease has become widespread, and the age of patients is decreasing every year; pancreatitis is already being registered in young people.
Etiology of the disease
There are two main causes of pancreatitis: drinking excessive amounts of alcohol (about 60%) and cholelithiasis (about 30%).
Additional factors contributing to the development of inflammation are:
- diseases of the duodenum;
- abdominal injuries;
- history of gastric or biliary tract surgery;
- infections – viral hepatitis B and C, mumps (“mumps”);
- helminthic infestations – ascariasis, enterobiasis;
- changes in hormonal levels;
- heredity;
- tumors, narrowing of the pancreatic ducts in the anamnesis.
There are two forms of pancreatitis: acute and chronic.
Symptoms of pancreatitis
| Form | Symptoms | a brief description of |
| Acute course is the most life-threatening | Severe pain in the upper part of the abdominal area, which is girdling in nature. | The pain affects the areas of the right or left hypochondrium, the epigastric region, the back and shoulder girdle may hurt. Antispasmodics have no effect and do not relieve pain. |
| Vomiting is common. | It doesn't bring relief. | |
| Less commonly – diarrhea, general weakness, dizziness. | The patient experiences fatigue and loss of appetite. | |
| Externally – an unnatural enlargement of the abdomen, signs of paresis of the intestines and stomach. | These signs indicate rapidly progressing inflammation. | |
| Increased temperature, pulse and heart rate are higher than normal, decreased blood pressure, pale skin color, dehydration, thick coating appears on the tongue, facial features become sharper. | These are already bad symptoms that can signal a high probability of death from pancreatitis. | |
| Chronic pancreatitis | The symptoms are not so pronounced, the main symptoms are: a feeling of heaviness after eating, especially with a large feast. Enlarged abdomen, nausea, belching, diarrhea, sudden attacks of hunger, sharp, quickly passing pain. | The chronic course does not pose a threat to the patient’s life, but requires adherence to a diet and constant monitoring by a specialist. Pancreatic cancer is registered in those patients who previously had a chronic process. Therefore, it is so important to understand the danger of this disease and the possibility of death from it. |
Reasons for diagnosis
The diagnosis is made after a series of studies and a comprehensive assessment of the results obtained. The following laboratory and instrumental tests are performed:
- a general blood test, first of all, check the level of leukocytes, determine the ESR - these are the main indicators of the presence or absence of an inflammatory process;
- blood biochemistry - to check the level of pancreatic enzymes;
- detection of amylase levels in a urine test is the main indicator for determining the degree of damage to the pancreas;
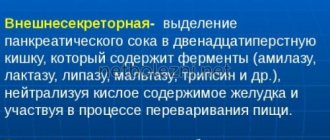
- determination of undigested fiber in the patient’s stool - how well enzymes enter the duodenum;
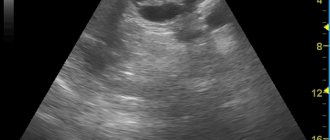
- Ultrasound and radiography of the abdominal organs - to assess the extent of inflammation and whether other organs are affected by the pathological process;
- gastroscopy;
- retrograde cholangiopancreatography using the endoscopic method;
- Carrying out the necessary functional tests.
Important! If acute pancreatitis is suspected, do not waste time in order to prevent the death of pancreatic cells and further death from pancreatic necrosis.
Is it possible to die from pancreatitis - true or false?
Death from pancreatitis, or more precisely from pancreatic necrosis, is possible. You can imagine it in the form of several stages, which follow one after another:
- The acute form of pancreatitis can develop reactively within a few days and pancreatic cells begin to die.
- Foci of necrosis appear. Cell death occurs due to the fact that the gland's enzymes begin to digest its own cells - this is called pancreatic necrosis.
- Areas of the gland that are attacked by their own enzymes become necrotic.
- The intestinal walls become inflamed and destroyed due to enzymes, bacteria and undigested intestinal contents infecting everything around.
- Bleeding occurs, and in some places the blood, on the contrary, coagulates and clogs the vessels.
- Damage to several vital organs (liver, kidneys, intestines, lungs) is observed.
- Cardiac and respiratory arrest occurs, especially quickly in elderly patients; the heart simply cannot cope with the load.
- The skin becomes pale grayish in color, the lips turn blue, the pupils stop responding to light, body temperature and pressure drop to a minimum level.
- Near-death sensations arise.
- Clinical death from pancreatitis is registered.