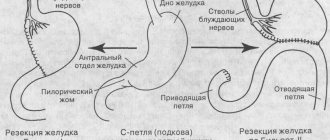
Principle of gastric bypass
is based on changes in the anatomical structure of the gastrointestinal tract, but excludes the removal of any organs. Reconstruction of the gastrointestinal tract is performed in the following order: the doctor removes the bottom and part of the body of the stomach, thus reducing its volume to 50-70 ml, and then connects it to the jejunum. Thus, food digestion no longer occurs in most of the stomach, and most of the small intestine is eliminated from the process. Digestive enzymes and juices from the pancreas and liver enter directly into the distal jejunum through a specially formed loop that includes the duodenum and part of the small intestine.
The effect of the operation is achieved by reducing the volume of the stomach and thus reducing the volume of food entering it, as well as reducing the level of its digestion and absorption. The bolus of food is less processed by juices and enzymes and travels a shorter distance through the gastrointestinal tract (GIT), not allowing nutrients to be absorbed. Gastric bypass surgery is also very effective in controlling type 2 diabetes and its complications.
What is gastric bypass?
Gastric Bypass (Gastric Bypass) is a bariatric surgery performed for weight loss.
The operation can be performed through an open incision (hardly used today), laparoscopically, or using a surgical robot. The operation creates a small pouch in the stomach that is directly connected to the small intestine. Weight loss then occurs due to two effects:
- Inability to eat a lot . Once in a small pouch, even a very small amount of food causes a feeling of fullness. As a result, there is a long-term decrease in appetite, and sometimes even a temporary aversion to food.
- Malabsorption is the inability to absorb nutrients . Decreased appetite is not the only reason for weight loss after this operation. The fact that food passes by the stomach and duodenum leads to a decrease in the level of absorption of nutrients. And especially fats, which are simply excreted from the body unchanged. This mechanism further enhances weight loss during gastric bypass surgery.
Weight loss with gastric bypass is on average 65 to 75% of excess weight. Primary weight loss occurs faster than with other bariatric surgeries - in about 12 months.
Problems with health and quality of life associated with excess weight are also solved. These improvements usually appear long before maximum weight loss is achieved.
Sleeve gastroplasty: brief description
Sleeve gastroplasty is a restrictive bariatric surgery that limits the amount of food entering the body. This result is achieved by reducing the volume of the stomach by 10 times. After crossing its ligamentous apparatus, a long narrow tube “sleeve” is cut out along the lesser curvature using a special template, preserving the pyloric sphincter, located in the outlet section of the stomach. This narrow “ventricle” has a diameter of no more than 1.5-2 cm and further serves as a food container. The severed area of the stomach, including the fundus and most of the body, is removed through one of the laparoscopic approaches, which is slightly expanded for this purpose.
Subject to a special dietary regimen after gastric sleeve surgery, patients lose up to 80% of excess weight. However, the operation is not without its drawbacks. There is a risk:
- formation of hiatal hernia;
- development of obstruction of the stomach “sleeve”;
- deficiency of vitamin B12, the absorption of which requires a glycoprotein produced in the fundus of the stomach.
Gastric bypass for morbid obesity
Morbid obesity is a disease that often has multiple associated medical conditions and is associated with a significant reduction in life expectancy. Many of them can be reversed if sufficiently pronounced and long-term weight loss is achieved.
Data suggest that diet, exercise, and medications have a high failure rate for most obese patients and that bariatric surgery is the most effective long-term way to achieve significant weight loss in these patients.
The risks of a non-surgical approach to your morbid obesity are a very high rate of failure to gain weight in the long term, leading to a higher risk of obesity-related medical conditions and reduced life expectancy.
Indications for surgery
In 1991, the National Institutes of Health (NIH) provided a consensus statement on patient selection for bariatric surgery. Patients are considered candidates for Gastric Bypass surgery if they meet one of the following criteria:
- BMI (Body Mass Index) > 40
- BMI 35-40 plus one of the following obesity-related comorbidities:
- severe diabetes mellitus;
- Pickwick's syndrome;
- obesity-related cardiomyopathy;
- severe sleep apnea;
- osteoarthritis;
- lifestyle incompatible with severe obesity.
To be candidates for gastric bypass, patients must have a history of unsuccessful attempts to lose an appropriate amount of weight through controlled diet changes. Patients must also follow a postoperative diet and exercise.
Indications and contraindications for mini-bypass surgery
Indications for mini-gastrobypass surgery do not differ from those for classical Roux-en-Y surgery. The intervention is carried out in the following cases:
- body mass index above 45-50 kg/m2;
- BMI is above 40 kg/m2 if the patient refuses to follow the recommended diet and rapid weight gain;
- the presence of diseases, successful treatment of which is possible only after losing weight;
- diabetes mellitus of non-insulin-dependent type due to obesity;
- lack of effect from other weight loss methods.
The choice in favor of mini-bypass surgery is made when there is a high risk of complications, the need to reduce the time spent under anesthesia or to facilitate the regeneration process as much as possible. To determine the presence of indications, choose the optimal method of work and eliminate contraindications, the clinic’s doctors will provide you with a full range of preoperative diagnostics.
After the examination, our doctor may refuse to perform surgery on you if it would jeopardize your life and health. Thus, mini-gastrobypass surgery is not performed for patients with exacerbation of cardiovascular diseases, blood clotting disorders, or acute infectious diseases. In addition, intervention is contraindicated if the patient is under 16-18 years of age, has acute mental disorders, drug addiction, or alcoholism. The procedure is not indicated for people with a BMI less than 40 kg/m2 and is rarely used as a first treatment option. First, the patient is recommended to try conservative methods of weight correction.
Contraindications
Contraindications for gastric bypass surgery:
- alcohol or drug addiction;
- serious mental disorders;
- decompensated stages of chronic diseases of the kidneys, heart, liver.
It is important to understand that bariatric surgery is only a tool to solve problems with persistent obesity. Patients who are not committed to long-term lifestyle changes may not be considered ideal candidates for this procedure.
Operations at the Assuta™ clinic
Gastric bypass surgery is designed to help you lose weight and reduce the risk of life-threatening complications that obesity can cause in the long term, including:
- Gastroesophageal reflux
- Diseases of the cardiovascular system
- Hypertension
- Severe form of sleep apnea (breath holding)
- Diabetes mellitus type 2
- Brain stroke
Gastric bypass and other surgeries to treat obesity are usually done only after you have tried other weight loss measures, such as changing your diet to a healthier diet and engaging in regular physical activity.
What are the advantages of gastric bypass over other types of bariatric surgery?
Benefits of the procedure
- Faster and more pronounced weight loss compared to other bariatric surgeries. The average loss in the first two years is 70% of excess weight.
- Lasting results in the long term. 5-6 years after surgery, weight loss remains in the average range of 70-80% of excess weight.
- Possible reversibility of the results of the operation with restoration of physiological digestion.
- There are no restrictions on sports activities and the level of possible physical activity.
Risks associated with bypass surgery
- Complications associated with the operation, such as, for example, the formation of fistulas at the suture sites.
- The need for lifelong intake of vitamins, minerals, and sometimes protein shakes as replacement therapy.
- Inability to take tableted nonsteroidal anti-inflammatory drugs (NSAIDs).
- Forced refusal of combined oral contraceptives and a number of medications in the form of capsules and tablets.
What is the difference between classic gastric bypass and mini gastric bypass?
The main difference between mini-gastrobypass and the classic version of the operation according to the method of the German scientist Wilhelm Roux is the number of anastomoses - artificial connections between parts of the intestine. With classic gastric bypass surgery, the surgeon cuts off a small part of the stomach and creates a small ventricle with a volume of about 20-40 ml. The small intestine is divided approximately down the middle. Its lower part is sutured to the newly created ventricle, and the upper part, connected to the remaining lobe of the large stomach, is implanted into the lower gastrointestinal tract. Thus, the doctor makes two anastomoses, one of which is located on the small stomach, the second on the final part of the jejunum.
The mini-gastrobypass technique is generally similar to the procedure described above. However, the small ventricle has an elongated shape and is directly sutured at the level of 150-200 cm from the beginning of the jejunum. Its complete intersection is not performed. Anastomosis is present only at the junction of the ventricle with the middle part of the small intestine. This approach allows Moscow Bariatric Group surgeons to significantly reduce the time of surgery and anesthesia.
Mini-gastrobypass compared to conventional gastric bypass is preferable in the following cases:
- poor tolerance to general anesthesia, need to reduce the duration of anesthesia;
- diseases of the cardiovascular system;
- high risk of postoperative complications;
- insufficient ability to recover in patients with diabetes (fewer number of anastomoses - it is easier for the body to heal damage).
The decision about the optimal method of operation remains with the surgeon. Our doctors accept it based on the results of a comprehensive examination and consultations with related specialists (endocrinologist, gastroenterologist, cardiologist), who will observe you free of charge throughout the course of treatment at the Moscow Bariatric Group.
Gastric Bypass Preparation and Precautions
Pregnancy
Pregnancy should be avoided in the first year after surgery. Periods of rapid weight loss are not suitable for trying to get pregnant or trying to maintain an existing pregnancy.
Preoperative fasting
To make your surgery technically safe, your surgeon may start you on the Optifast diet at least two weeks before your surgery. This is an ultra-low-calorie diet (800 Kcal per day) with a predominance of liquid dishes.
It is designed to shrink the liver and reduce the risk of surgical complications. She also introduces you to the liquid diet regimen that you will need to follow in the postoperative period.
Smoking
Smoking increases the risk of pulmonary complications and blood clots, regardless of the type of surgery. It is recommended that you try to quit smoking before surgery. Even quitting smoking a week before surgery can be helpful.
Preoperative gastroscopy
Preoperative gastroscopy is used to ensure that there are no other physical abnormalities that might prevent surgery.
For patients undergoing gastric bypass surgery, this is extremely important. Because the stomach will be divided and most of it will not be accessible, it is important that this part is examined before surgery.
Other tests
The doctor may order other tests depending on your condition - ECG, ultrasound of the pancreas, test for sleep apnea, etc.
It is important to understand that after surgery, most of the stomach will not be accessible using traditional endoscopy. Nor will there be access to remove gallstones using the endoscopic ERCP procedure. Surgery will be required to access the stomach or biliary tract.
Biliopancreatic bypass for morbid obesity and metabolic syndrome
Biliopancreatic shunting is a restrictive shunting intervention that involves reducing the stomach and reconstructing the small intestine with the separation of the pathways for food and digestive juices. In bariatric surgery, two modifications of biliopancreatic bypass are performed: the Scopinaro operation and the Hess-Marceau operation.
The general scheme of intervention involves resection of the stomach and its anastomosis with the small intestine; application of enteroenteroanastomosis between the proximal resected segment and the ileum. Thus, an alimentary loop is created (for the passage of food), a biliopancreatic loop (for the removal of digestive juices) and a general loop where they are mixed. BPS is considered the most effective bariatric surgery for highly obese patients with comorbidities.
Biliopancreatic bypass is a combined intervention combining gastrorestrictive and malabsorptive components. In bariatric surgery, BPS replaced various types of small intestinal bypass (including jejunoileobypass): the latter involved the exclusion of the small intestine from the passage of food and the digestive process, which led to the development of severe metabolic disorders in patients. At the end of the 70s of the last century, the Italian surgeon Scopinaro performed a bypass operation, during which he separated the transport routes of chyme and digestive juices, without completely excluding the small intestine from digestion. A more modern modification of this method is the Hess-Marseau-Baltasar biliopancreatic bypass with exclusion of the duodenum, which can be performed through abdominal or laparoscopic access.
First of all, biliopancreatic bypass surgery is indicated for patients with morbid obesity and a BMI over 45 kg/m2, in whom previous conservative therapy was ineffective. Additional reasons for BPS are concomitant diseases associated with excess weight (type 2 diabetes mellitus, sleep apnea, hypertension, hypercholesterolemia, non-alcoholic fatty liver disease, deforming arthrosis, etc.). Persons suffering from hyperobesity (BMI more than 50-60 kg/m2) usually undergo step-by-step treatment: first, a longitudinal gastrectomy is performed, then (after 1-1.5 years), after partial loss of excess weight, a bypass stage of the operation. BPS is suitable for patients who require additional surgical treatment for cholelithiasis or gastroesophageal reflux disease.
Biliopancreatic bypass may be refused in the case of severe and decompensated somatic diseases, previous operations on the digestive tract, exacerbation of any gastrointestinal pathology, bleeding disorders, or oncological diseases. The operation is not performed on pregnant women and women; persons suffering from alcoholism, mental disorders and drug addiction. A criterion for exclusion from candidates for BPS may be age (under 18 and over 60-65 years).
In order to establish indications and exclude contraindications for biliopancreatic bypass, patients undergo a complete clinical and instrumental examination.
The BPS operation is performed under general anesthesia laparoscopically through 5-7 punctures of the abdominal wall. The complex of biliopancreatic bypass in the Scopinaro modification includes distal resection of 2/3 of the stomach and the application of a small intestinal anastomosis according to Roux. A number of authors recommend supplementing BPS with cholecystectomy and appendectomy, citing the prevention of the development of cholelithiasis and appendicitis during active weight loss.
Mobilization of the stomach is performed according to the generally accepted method in operative gastroenterology. The stomach is then sutured and cut off at the border of the pyloroantrum. The duodenal stump is sutured with a purse-string suture. A small reservoir with a volume of 200-250 ml is formed in the upper part of the stomach, the distal parts of the stomach are completely removed. After gastrectomy, the optimal length of the total, biliopancreatic and gastric loop is determined. Then, at the intended location, the jejunum is intersected, after which its distal segment is anastomosed with the stump of the stomach (gastroenteroanastomosis), and the proximal segment with the ileum (jejunoileal anastomosis). The duration of the operation can vary from 3 to 6 hours depending on the degree of obesity, the chosen technique and the experience of the bariatric surgeon.
Biliopancreatic bypass in the Hess-Maurceau modification differs in that the first stage is not a distal gastrectomy, but a sleeve gastroplasty with preservation of the pylorus. The duodenum is transected, its distal stump is peritonized, and the segment adjacent to the pylorus is anastomosed with the distal segment of the transected small intestine (duodenoileoanastomosis).
As a result of biliopancreatic shunting, three loops are formed from the small intestine: alimentary (about 200 cm long), through which food is transported from the small stomach; biliopancreatic, through which bile and pancreatic enzymes are removed; general (50-70 cm long), where food is mixed with digestive juices. The effectiveness of biliopancreatic bypass is ensured by two mechanisms: a decrease in the volume of the stomach and the absorptive surface of the intestine, which ultimately leads to a decrease in excess body weight.
The main advantage of BPS is its unsurpassed effectiveness compared to other gastrorestrictive and bypass operations. 1.5-2 years after biliopancreatic bypass, the loss of excess body weight is 75-100%, and the result is consistently maintained over subsequent years. Another advantage of the method is the absence of restrictions on calorie intake and the need to follow a diet, starting from 3-4 weeks after surgery. Theoretically, after BPS, complete restoration of the continuity of the small intestine is possible, but in practice such a need usually does not arise.
Numerous clinical studies have confirmed the therapeutic effect of biliopancreatic bypass in relation to concomitant diseases. A pronounced and sustained decrease in the level of total cholesterol, LDL and blood triglycerides in the postoperative period has been proven. No less significant is the decrease in blood glucose levels - after BPS, patients with type 2 diabetes mellitus experience stable normoglycemia without additional drug support and diet therapy. In addition, blood pressure is clinically significantly reduced and cardiovascular risk is reduced.
The recovery period after surgery is longer - 6-8 weeks, which is associated with serious reconstruction of the gastrointestinal tract.
Patients who have undergone BPS should take vitamin and mineral supplements for life, have regular blood tests to assess nutritional status, and visit medical specialists (nutritionist, bariatric surgeon). During the first year after biliopancreatic bypass, control examinations are carried out once every 3 months, during the second year once every 6 months, then annually.
(based on scientific publications)
Advantages of gastric bypass surgery in Belgium
- Belgian surgeons have extensive experience in performing this type of surgery. So only in the Namur Obesity Clinic (a division of the Sainte-Elizabeth Clinic) up to several hundred procedures are performed every year. Experience in this case creates a high level of competence and becomes a guarantee of minimal risk of complications.
- Possibility of using robotic surgery. The experience of Belgian surgeons also includes performing gastric bypass surgery using a surgical robot. The robot-assisted version of the procedure is associated with less postoperative bleeding and less need for blood transfusions. The recovery period is also significantly shorter. But such an operation is 30-40% more expensive than a standard laparoscopic procedure.
- The price of surgery in Belgium is 30-50% lower than in neighboring countries such as Germany or Switzerland.
Why do they trust us and choose the CELT clinic?
The specialists of the multidisciplinary CELT clinic have the most extensive experience in performing biliopancreatic bypass operations in our country and in Eastern Europe, and the experience of performing BPS in the SADI modification is one of the most advanced in the world. The head of the obesity surgery service of the clinic - Professor Yuri Ivanovich Yashkov - is one of the leading bariatric surgeons in the world, from 2000 to 2017 he headed the Russian Society of Bariatric Surgeons, from 2012 to 2014 he was President of the European branch of the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO ). We have proven ourselves so well in this area that even patients from America and Western Europe come to us, attracted by our affordable prices and good results. The International Federation for the Surgery of Obesity (IFSO) awarded the CELT Multidisciplinary Clinic the honorary title of “Excellence Center” in the field of bariatric surgery.
The clinic has a friendly multidisciplinary team, which includes surgeons, an endocrinologist, and a therapist. Thanks to their close cooperation, well-coordinated work, and constant dynamic monitoring of patients, it is possible to achieve excellent results in the most difficult clinical situations. Significant emphasis is placed on performing repeat bariatric surgeries. We also accept patients who have previously been operated on in other clinics, but did not receive sufficient results from the previous operation.
How is gastric bypass performed in Belgium?
The operation is performed under general anesthesia. The procedure involves making several small incisions through which laparoscopic instruments are inserted to perform the operation.
The surgeon then redirects your digestive tract to bypass most of your stomach and part of your small intestine.
Although gastric bypass surgery is performed as a laparoscopic procedure, you may need to stay at the medical center for two days after surgery.
During this time, a multidisciplinary team of surgeons, nutritionists and psychologists work together to ensure that everything goes well and you are in a state of health that allows you to leave the clinic safely.
Postoperative period
After undergoing gastric bypass surgery, as after any bariatric surgery, you will not be able to eat for one to two days. This is necessary to ensure that your stomach and digestive system recover properly after the procedure. Then, for 12 days, you will need to follow a special diet. At first - only drink liquids, then - soft food. Eventually you will be able to eat normal foods but still have strict restrictions on how much you eat and drink.
Gastric recovery and side effects
In the postoperative period, you may need time to figure out how your new stomach behaves, and you may have problems with discomfort after eating and occasional vomiting.
Dumping syndrome
After gastric bypass surgery, you may experience intolerance to certain foods, usually fatty foods, dairy products or sweets. This can cause unpleasant symptoms similar to motion sickness:
- sweating;
- nausea;
- shake;
- abdominal pain;
- diarrhea that lasts from a few minutes to an hour.
This condition is known as "dumping syndrome."
Some patients find this a beneficial side effect because it increases their inability to consume high-calorie foods.
Other possible side effects
Combined oral contraceptives (COCs) will no longer be fully absorbed and provide a contraceptive effect. Therefore, it is necessary to find another means of contraception after surgery.
Anti-inflammatory drugs (aspirin, diclofenac, etc.) in any form are prohibited after bypass surgery, as they significantly increase acid production and put the patient at risk of developing intestinal erosions and ulcers.
Deficiency of vitamins and microelements. Gastric bypass surgery results in vitamin deficiencies that can be corrected by taking vitamin supplements throughout life. Although this may seem overwhelming, remember that bypass surgery allows you to eliminate the need for multiple medications every day.
What results can you expect?
Weight loss with gastric bypass can be very rapid. You will quickly lose a large amount of weight in the first few months after gastric bypass surgery.
Studies have shown that, on average, gastric bypass patients lose their appetite within the first five months after surgery. During this period, it is important to take the right amount of calories, proteins and vitamins so as not to feel sick, weak and possibly lose some hair.
It is important that you follow the dietary recommendations given to you by your dietitian. Your chances of achieving your weight loss goals increase if you follow our bariatric program after surgery.
Your goal is to burn fat, not muscle, so you need to take protein to maintain muscle mass. Your best chance of losing weight with gastric bypass is in the first nine months.
Remember that the purpose of surgery is to make you healthier, increase your life expectancy, and reduce problems caused by obesity-related diseases, not to reduce your weight below normal.
Find out more about gastric bypass surgery in Belgium. Write to us or request a call back.
Advantages and disadvantages of mini-bypass surgery
The advantages of mini-gastrobypass surgery include:
- weight loss that is many times greater than that achieved with other treatment methods;
- reducing the risk of heart attacks, strokes and other diseases associated with excess weight;
- complete cure of type II diabetes mellitus in 98% of cases;
- less surgical trauma compared to classic bypass surgery;
- shorter and easier recovery period;
- significant reduction in operational risks;
- reversibility of changes - if necessary, the intestines can be returned to their previous state.
The main disadvantage of the procedure is insufficient absorption of vitamins. They must be taken in tablet form. In addition, dumping syndrome may occur when eating foods rich in simple carbohydrates and fats. In most cases, it manifests itself with vomiting, diarrhea, dizziness and a feeling of heat in the upper half of the body. It should be noted that this is only conditionally a disadvantage. In fact, this reaction to energy-dense foods will keep you from eating them and will provide additional protection against weight gain again in the future.