July 2, 2021
As part of the materials on the treatment of oncological diseases, we have not yet touched upon such a critical area as surgery in our blog. Although surgical removal of the tumor is the only radical treatment method that exists in oncology. A radical method is one that eliminates the main problem and the cause of all other severe symptoms: malignant neoplasm.
“Medicine 24/7”, first of all, is a surgical hospital with a serious workload: among private clinics in Moscow, ours is in first place in the consumption of blood and blood components that are needed during operations.
Liver operations are not the most important and popular area of the clinic’s work. However, the fact that in our hospital, in principle, such manipulations are performed, and patients are not sent somewhere else, is a marker and an indicator of the highly qualified team of surgeons.
Liver surgery is equivalent to brain and open heart surgery. As a rule, this is the seventh category of complexity out of 7 possible.
At the same time, successful surgical treatment of malignant neoplasms in the liver allows one to count on prolonging the patient’s life: a five-year survival rate of 40-50% for primary liver cancer or single metastases is a good result.
We often receive patients who were not operated on in other clinics for one official reason or another. But people want a second chance, and we give it to them.
In this article we will try to explain why the liver so often requires attention when treating cancer, why not every surgeon risks operating on it, and whether there are alternatives to a scalpel.
Meeting point: why cancer so often affects the liver
The liver is an amazingly multi-tasking organ. Her work can be divided into 3 areas.
- Deposit. The body stores many necessary things in the liver: energy reserves in the form of glycogen; some vitamins (A, D, B12, K, PP); microelements (the main one is iron). There is also a very significant amount of blood constantly present here. If, as a result of an injury, a hole is formed in the body that was not provided for by nature, then this blood reserve will be urgently released into the main bloodstream and will temporarily compensate for the blood loss.
- Synthesis. This organ is a “factory” of important hormones and enzymes. Many blood plasma proteins, including those that allow blood to clot when needed, but not stick together into blood clots in normal life, are formed here. But most importantly, the liver produces bile, a component of healthy digestion.
- Detox. The liver is unique in that it can neutralize poisons, toxins, allergens and other dangerous substances that enter the body from the outside, as well as those that arise as a product of our metabolism.
All these important functions of the liver are provided by its special blood supply system.
About 1.5 liters of blood passes through the liver per minute. About a quarter of this volume comes through the hepatic artery, the remaining 75% through the portal vein from the intestine.
Inside the liver there are sinusoids - special capillaries in which arterial blood mixes with venous blood and this mixture is “filtered” by hepatocytes (liver tissue cells): useful substances and nutrients are stored, toxins are neutralized as a result of complex chemical reactions. Then the blood, which has gone through all the stages of “processing,” enters the hepatic vein and returns to the heart.
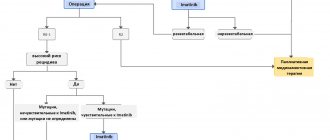
Diagram of blood circulation in the liver
But this same wonderful system, which allows the liver to filter 2,000 liters of blood per day, also contributes to the spread of cancer cells. They are carried throughout the body through the bloodstream, and the liver, which allows and retains everything unnecessary, thus becomes a target for metastases.
Liver tumors: hard to find, easy to start, sometimes impossible to cut out
According to statistics, a primary liver tumor - hepatocellular cancer - is less common than metastases in this organ from other malignant neoplasms. The total number of patients with liver metastases in Russia is more than 100,000 - many times more than patients with primary tumors of the liver and intrahepatic bile ducts (less than 15,000).
But almost all malignant neoplasms metastasize to the liver. Colon cancer (colorectal cancer) does this in 50% of cases. In 30% of cases, metastatic lesions occur here in melanoma and breast cancer.
Our leading oncologist surgeon in this area, Anton Aleksandrovich Ivanov, gives one of the most interesting examples in his practice.
“Patient with breast cancer metastases in the liver. Usually it is not customary to operate on such cases at all. But during the examination, we found out that the liver was the only organ that succumbed to metastasis. This was a rare success, and the surgeons made a collective decision: to operate.
And when, in preparation for the operation, a biopsy of the metastases was taken, it turned out that the cancer cells in the liver had mutated, and the initial HER2-negative status of the tumor changed to HER2-positive, 3+. This means that the disease is sensitive to Herceptin, an effective drug against this type of cancer. The patient had metastases removed and half of the liver was resected. More than 10 years have passed, she is receiving the drug and is still alive. When he comes for examinations, he complains not so much about his health, but about his hooligan grandchildren.”
Unfortunately, both liver cancer and liver metastases are often diagnosed in an already advanced state.
Signs and symptoms of liver tumors
The most common manifestation of liver tumors in children is an increase in the size of the abdomen and a detectable thickening. Other symptoms include loss of appetite and weight loss. Loose stools or constipation are rare.
Anemia (anemia), fever, vomiting and jaundice usually appear with an advanced tumor process, and more often in patients with hepatocellular cancer.
In rare cases, patients with hepatoblastoma experience premature puberty due to the tumor's production of the hormone human chorionic gonadotropin.
Sits quietly: why liver tumors are discovered too late
The reasons for this situation are the other side of the organ’s “superpowers”. The liver has a huge margin of safety: to cope with its duties, 15-20% of healthy parenchyma (liver tissue) is enough for it.
“Tumors themselves do not hurt, but simply use the resource of healthy tissue. So it turns out that a liver affected by a tumor may not give signals at all until the disease affects more than half of the organ - and this is stage III-IV: 58% of primary liver tumors are detected in Russia in a state of advanced process,” explains Anton Aleksandrovich .
At the same time, ultrasound and even CT can miss a node in the liver if it is still very small, and not in 100% of cases such studies make it possible to understand the exact size, outline and nature of the lesion.
This diagnostic difficulty can be overcome: use hepatotropic (i.e., acting specifically on the liver) contrast agents for MRI. There are three of them in total; in Russia, since 2007, only one has been approved and recommended for use: Primovist. It is capable of accumulating in hepatocytes, but malignant tumors do not “absorb” it, due to this they become most clearly visible in the photographs.
An example of how the contrast agent Primovist works
Today, this drug is the gold standard for MRI diagnosis of liver tumors; hepatologists at Medicine 24/7 use it without fail, which ensures the proper level of accuracy.
But, unfortunately, in many regions the situation is more complicated: finding clinics there that know and use Primovist is still difficult, as it was 10 years ago.
Determination of the stage (prevalence) of malignant liver tumors
After a comprehensive examination, the stage of the disease is determined, which is important for planning treatment and assessing the prognosis (outcome) of the disease.
Stage I - the tumor is completely removable
Stage II - after removal of the tumor, individual tumor cells remain.
Stage III - tumor rupture during surgery, the presence of affected lymph nodes, or only partial removal of the tumor.
Stage IV - presence of distant metastases
Why not every surgeon can perform liver surgery
Even having discovered a tumor focus in the liver, not every doctor will be able to remove it: working in the hepatopancreatobiliary zone is more difficult for a surgeon than reading the word “hepatopancreatobiliary” out loud the first time.
This area includes the liver (Greek hepar), pancreas (Latin pancreas), gallbladder (Latin vesica biliaris) and bile ducts. All these organs are closely related anatomically and functionally.
Most interventions in other areas of surgery take place on one small specific localization, and if we are talking about resection (removal of part) of the liver, then the amount of work is large, even when affecting one or two segments.
It is difficult, firstly, purely technically.
The liver is on the right side, the pancreas is on the left, all their ducts combine into one and exit into the duodenum
The liver is very complex, it consists of segments and lobes, between which there are ligaments, all of which are literally entangled and penetrated by veins, arteries and bile ducts.
Relationships between liver segments, bile ducts and blood vessels
There is a risk that in this area there is a large vascular bundle, everything happens very close to the inferior vena cava, the hepatic artery: these are large main vessels. The liver itself bleeds heavily. Accordingly, there is a danger of serious blood loss, the operation must be both as fast as possible and extremely careful.
Such an intervention must be performed by a person with extensive experience in carrying out these operations, and the number of such specialists is limited. We have two of these at Medicine 24/7, and patients often come to them through referrals from colleagues from other (very respected) medical institutions, where, however, there are no specialists with sufficient skills.
Symptoms of stage 4 liver cancer
The last stage of the disease is characterized by the addition of signs of tumor metastases affecting other organs and tissues, including:
- pain in the spine and ribs, arms and legs;
- internal bleeding;
- other painful and life-threatening conditions for the patient.
If you need a second opinion to clarify your diagnosis or treatment plan, send us an application and documents for consultation, or schedule an in-person consultation by phone.
+7 499 490-24-13
Expert opinion
How the operation works: risk control and online decision making
Both the doctor and the patient carefully prepare for liver surgery so that everything goes as predictably as possible. Anton Aleksandrovich Ivanov explained in detail how the oncologist surgeon and his team prepare for liver surgery, and that they try to plan for everything.
“In order to accurately determine the scope and method of intervention, all necessary studies are carried out. The operation area is visualized with maximum accuracy. The results of many analyzes are taken into account. For example, for certain infectious diseases or a decrease in the number of platelets in the blood, the doctor will first select therapy to restore normal values and only then prescribe surgery.
Directly at the time of the intervention, in addition to the doctor, there is a whole team of specialists in the operating room monitoring the patient’s vital activity: anesthesiologists, resuscitators, transfusiologists, and an operating nurse. Of course, today a doctor doesn’t even remove a tooth alone, but liver operations bring together the largest team in the operating room.
A supply of blood components is required - red blood cells, plasma, so that at any time in case of large blood losses they can be compensated. In our practice, we use a special device, Cell Saver, which immediately separates (separates) red blood cells from the patient’s lost blood and returns them back to the patient’s bloodstream. “Our own” are always more favorable than “canned” donor red blood cells, even those matching the blood type.”
The patient's blood enters the Cell Saver and it returns red blood cells to the patient
Quite regularly, operations are simultaneous (one-stage): liver resection takes place simultaneously with other interventions. Both the primary focus, for example, in the colon, and the metastasis in the liver are removed.
However, even with maximum predictability and complete control of the process, surgeons sometimes deviate from the planned plan.
For example, during surgery for a primary stomach tumor, an accidental discovery may occur: a small single metastasis in the liver. In this case, surgeons can invite colleagues, specialists in liver surgery, to carry out their stage: removing part of the liver.
Joint operations are good because the patient is exposed to anesthesia and the difficulties of the recovery period only once.
The operation takes from 1.5 hours (for resection of a single metastasis) to 10-12. “In my practice, the longest operation with simultaneous removal of the primary lesion in the intestine and metastases in the liver lasted 15 hours,” recalls Dr. Ivanov, “but this is rather an exceptional case.”
Not all tumors are equally operable
Size matters. If the tumor is large and has managed to “eat” too much healthy tissue, then removing it may be pointless. In order for the patient to be guaranteed to undergo surgery, at least 30% of the liver must remain after removal of the part. With fibrosis, fatty hepatosis or cirrhosis (and they often accompany or precede liver cancer), this figure increases to 35-40%, otherwise the remaining liver with these pathologies will not be able to function adequately.
Localization of foci and their number. If metastases are multiple and “scattered” over several segments, then removing them may not be advisable: statistics show that survival rate does not improve with such operations.
The prevalence of tumor foci sometimes makes surgical treatment impossible
Contraindications. These are the patient's health conditions that make the success of the proposed operation statistically minimal.
- Peritoneal carcinomatosis (carcinomatosis is a less familiar term, but medically more accurate). Cancer cells from the primary focus through the blood and lymph flow: spread throughout the abdominal cavity and “grow” in several organs at once.
- Intractable ascites is the accumulation of a large amount of fluid in the abdominal cavity. In addition to the fact that this creates difficulties during surgery, ascites acts as a factor that provokes the spread of metastases. If it cannot be controlled, then there is a high probability that metastases will quickly recur.
- Mechanical jaundice. A tumor focus that compresses the bile ducts disrupts the outflow of bile and provokes the entry of bilirubin (a breakdown product of hemoglobin) into the blood. As it accumulates, it colors the sclera (whites of the eyes), skin and mucous membranes of the patient yellow. This is dangerous: bilirubin is toxic and aggravates the patient’s condition.
However, even for such patients for whom surgery is not an option, treatment options exist.
Alternatives to the scalpel
In cases where the patient is faced with the impossibility of removing a tumor in the liver using classical surgery, there is interventional oncology and endovascular (“intravascular”) surgery.
Hepatologists at Medicine 24/7 actively use them to improve survival rates. Like classical operations, these methods also have limitations, but thanks to them, many of our patients with unresectable liver tumors have received a second chance to prolong life.
Chemoembolization of vessels feeding the tumor is the main method of endovascular treatment of liver cancer. A thin catheter inserted through the femoral artery is advanced directly into the vessel supplying blood to the tumor tissue and delivers a drug containing microcapsules made of special medical plastic. They mechanically block the blood flow, depriving tumor cells of nutrition, and release a drug against tumor growth, directly into the lesion and in high concentration.
This method can reduce the volume of the tumor in the liver, and, therefore, in some cases, make one of the options for surgical resection possible.
Scheme of introducing emboli (microcapsules) through a catheter directly to the tumor
Radiofrequency ablation of the tumor. Through a puncture in the skin, a thin electrode is applied directly to the tumor site, at the end of which a radiofrequency pulse creates a high temperature. And the surgeon precisely “burns out” the tumor.
Stenting. Installing a stent (dilator) into a bile duct or vessel compressed by a tumor helps to overcome, for example, obstructive jaundice, improve blood flow and outflow of bile - i.e. remove one of the main contraindications for surgery.
These are the most popular methods in our clinic. In other cases, we use cryodestruction (tumor destruction at low temperatures), hyperthermic chemotherapy HIPEC (against peritoneal carcinomatosis), and other suitable methods.
Histological signs of liver angiosarcoma: article, diagnosis and prognosis
Angiosarcoma of the liver is an extremely aggressive oncological disease, the occurrence of which is directly caused by contact with toxic chemicals - copper, arsenic, vinyl chloride, as well as radiation. Angiosarcoma often occurs due to the accumulation in the body of the substance thorotrast, which was used in the last century as a contrast agent for X-ray studies.
The symptoms of angiosarcoma are non-specific - the patient may experience abdominal pain, bloating, fever, loss of weight and appetite. Early diagnosis of angiosarcoma is difficult because at first it is asymptomatic. During palpation, a compaction may be felt; during auscultation, the doctor may hear characteristic noises.
Diagnosis of angiosarcoma is the same as in other cases of suspected liver cancer. X-ray of the abdominal cavity allows you to see Thorotrast deposits in the spleen and liver, or areas of hemorrhage in the soft tissues. For histological examination of tissue, diagnostic laparoscopy is performed, during which a tumor sample is removed, after which it is sent for biopsy.
Unfortunately, angiosarcoma is most often discovered at a later stage, when treatment, either conservative or surgical, will no longer produce any results. In order not to miss the onset of the development of the disease and to begin treatment in a timely manner, it is necessary to take care of your health and undergo an annual medical examination at the Yusupov Hospital. Our clinic is equipped with the most modern equipment, the accuracy of the results of which allows us to recognize cancer in the initial stages of development.
Problems and prognoses in the surgical treatment of liver tumors
“The lack of competent surgeons is the most obvious difficulty that patients face,” says Anton Aleksandrovich Ivanov. – I have worked for 19 years in both public and private medicine, and everywhere there are enthusiastic doctors who do not have enough experience, who say: “Now we’ll cut it out!”, They take the patient to the operating table, but perform the operation to the wrong extent, which one was needed, for example. Unfortunately, the prognosis for such patients does not improve after surgery.”
There are doctors who honestly admit that they do not perform such operations, and refer the patient to large centers, to capitals. On the one hand, this is safer than a half-educated surgeon, on the other hand, it is extremely difficult for such a patient to get free treatment. Even in the compulsory medical insurance system, liver surgery is not included in the standard of medical care. This is a high-tech surgical procedure performed according to quotas.
In any case, the patient must remember, no matter how frightening the verdict may be, it is necessary to get a second opinion: this is true not only in therapy, clinical oncology, but also in surgery.
At Medicine 24/7, our surgeons and hepatologists, despite their impressive experience, always discuss each liver operation collectively in order to make the most informed decision.
Price. For those unlucky enough to qualify for free surgery, surgical treatment of liver tumors costs serious money. In our private hospital, for example, the resection itself, plus a stay in the clinic, pre- and postoperative studies, resuscitation, costs about 700,000 rubles.
Abroad, despite the fact that the same technologies are used and the same risks are present, liver surgery for metastatic lesions costs 6 times more: from 60,000 euros.
Difficulties with transplantation. For each patient with unresectable tumors and contraindications to other interventions, ideally there should always be a last chance: a liver transplant. But in Russia, transplantology still lags behind world experience.
Largely due to administrative problems. The legislation and the issuance of licenses for donor organ transplants are not fully regulated; a large waiting list, and the lists of those in need of a transplant are not combined by region. In the EU, for example, the control system for donor organs is centralized: a suitable liver that appears in one of the countries can be promptly brought to another country where it is urgently needed.
Moreover, the problem is in the public consciousness. In Western Europe or the USA, the consent of, say, a niece to give part of her liver for a transplant to her uncle is a fairly commonplace story. Our relatives refuse to become donors. Not all people know how successfully a liver from which part has been taken away is restored, but not all surgeons are ready to risk two lives, not one.
Hope for bioengineering developments: judging by current work in this direction, in 20 years scientists will learn to “grow” an artificial liver in the required quantities. We sincerely hope to catch this moment.
In the meantime, the bright minds of researchers are figuring out how to solve the problem of shortage of donor material, the golden hands of our surgeons are gaining new experience.
The ALPPS (Associated Liver Partition and Portal vein ligation for Staged hepatectomy) technique, described and tested by German surgeons in 2012, expands the possibilities for surgical treatment of liver tumors previously considered unresectable.
The point of this two-stage operation is not to remove the part of the liver affected by the tumor at once, but to separate it from healthy tissue, separate their blood flow and, as it were, give the patient two autonomous livers. Then wait 6-8 days until the remaining “piece” of healthy tissue grows to a size sufficient to perform its functions, and remove the metastases of the affected part in full.
Within a week, the left lobe of the liver grows to a size that allows it to function normally.
In Russia, ALPPS is not yet widely used, but the experience that our domestic colleagues already have shows results as successful as those of foreign surgeons.
Development of endoscopic surgery. Technical equipment is still developing rapidly. Now we can, using thin flexible microinstruments inserted into two skin punctures, cure a person, remove an entire organ, etc. Surgeons can perform very complex procedures that were not possible 20-30 years ago. The quality of images from microscopic cameras during such operations improves every year.
The main thing is that doctors need enough motivation and desire to learn and master these technologies. And of course, serious money is needed to purchase sophisticated equipment and train doctors. Both of these factors can rarely be combined in a medical institution, even if it is an advanced scientific institute. And among private clinics, we are the only ones who perform central liver resection.