Vagotomy technique
There are a large number of different modifications for performing both vagotomy and pyloroplasty. Vagotomy is distinguished between trunk subdiaphragmatic (intersection of the entire nerve in the thickness of the esophageal wall at the point where it exits through the diaphragm into the abdominal cavity), selective - intersection of branches that innervate only the stomach, and selective proximal - intersection of the trunks of the vagus nerve going to the upper parts of the stomach. Laparoscopically, vagotomy is more often performed, since pyloroplasty requires the use of expensive consumables (stitching devices, atraumatic suture material). Four to five trocars are used to perform vagotomy. Through one, a laparoscope is inserted, into three or four others - instruments for retracting and holding organs, as well as crossing the vagus nerve, which is carried out using endoscissors using coagulation. Often during the operation, endoscopic staplers or manual suturing of the stomach wall are used. Trocar wounds of 1 cm are sutured, 0.5 cm are sealed with a plaster. The operation is performed under anesthesia.
Stomach surgery
Stomach surgery ¦ Organ-preserving operations for gastric and duodenal ulcers
In case of gastric ulcer and/or duodenal ulcer, both complicated and uncomplicated, in accordance with the available indications, patients undergo organ-preserving surgical interventions - intersection of the branches of the vagus nerve, or vagotomy, the choice of method is carried out strictly on an individual basis.
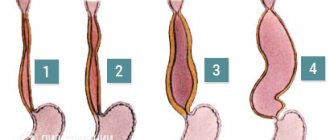
The first subphrenic 2-sided truncal vagotomy was performed in 1932 by Piri. However, it should be noted that the method he proposed has significant drawbacks, because performing such an operation leads to parasympathetic denervation of the abdominal organs and disruption of their normal functioning: the appearance of atony of the stomach and gallbladder, the development of diarrhea, alkaline reflux gastritis, etc. Therefore, at the present stage, many experts believe that truncal vagotomy should be resorted to only in special cases.
The so-called “selective” gastric vagotomy, which consists in crossing only the anterior and posterior branches of the vagus going to the stomach below the place where the branches to the gallbladder and liver depart from it, is also fraught with certain complications and, in particular, causes problems with the pylorus, which requires drainage surgery, namely, pyloroplasty according to Heineke-Mikulich or Judd with excision of the ulcerative defect of the anterior wall of the stomach and part of the pylorus, or intervention according to Finney, or the creation of a bypass gastroduodenoanastomosis according to Dzhabula. However, such a step cannot in any way be called an organ-preserving element.
Most doctors with sufficient experience in performing vagotomy believe that the main organ-preserving operation for peptic ulcer disease should be proximal selective vagotomy, not accompanied by drainage intervention. This tactic was developed in 1964 by Holle and Hart; its essence consists of parasympathetic denervation of only the acid-producing zone, i.e. the body of the stomach and its fundus while maintaining the innervation of the pylorus and antrum. This method allows you to achieve an adequate reduction in gastric secretion and prevents the occurrence of dumping syndrome, alkaline reflux gastritis and diarrhea.
At the present stage, in order to reduce the morbidity of this operation, specialists use laparoscopic techniques to perform it. The entire procedure is carried out through four miniature puncture incisions on the anterior abdominal wall. Using special endoscopic instruments, the surgeon carefully isolates the posterior vagus nerve near the gastroesophageal junction and crosses it and its smaller branches with an ultrasonic dissector. The anterior branches of the vagus cross at the anterior wall of the lesser curvature of the stomach, moving from the esophagus to the angle of the stomach. To monitor the effectiveness of the intervention, a study is carried out with a special probe – pH meter. If a patient has a combined pathology: chronic calculous cholecystitis, hiatal hernia, it can also be corrected in parallel by performing laparoscopic cholecystectomy or laparoscopic Nissen or Toupet fundoplication.
(495) 506-61-01 — the best clinics for gastric and duodenal surgery
REQUEST TO THE CLINIC
Postoperative complications with vagotomy
Possible complications during surgery include damage to the esophagus, bleeding from the gastric arteries. After vagotomies, recurrent ulcers occur quite often (up to 10%). Dumping syndrome (rapid evacuation of food from the stomach into the intestines and the associated complex symptom complex - weakness, sweating, palpitations, digestive disorders that occur after eating), duodeno-gastric reflux (reverse reflux of duodenal contents into the stomach - pain, regurgitation and vomiting of bile, constant bitterness in the mouth, weight loss), diarrhea (stool disorders). See also Complications possible after laparoscopy
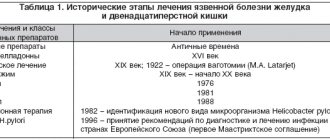
Evolution of treatment for patients with GERD: from vagotomy to proven pharmacotherapy
GERD is called a disease of modern civilization or a diagnosis of the “Western lifestyle.” In addition to heartburn, its manifestations include belching and difficulty swallowing (dysphagia), which can cause serious discomfort to a person, reduce his quality of life, and the chronic course of the disease in some cases can lead to complications such as damage to the mucous membrane (esophagitis) and cancer ( adenocarcinoma) of the esophagus2. The prevalence of GERD among adults worldwide reaches 40%, and in Russia it affects from 18% to 46% of the adult population, and the incidence rate is growing1.
GERD develops as a result of regular reflux of stomach contents into the esophagus and is an acid-dependent disease, which also includes ulcers, etc. The treatment of such diseases has a long history: the first attempts to treat GERD were examples of alternative medicine and herbal medicine. In the 19th century, an “advanced” method was invented - vagotomy: it was proposed to treat severe heartburn and ulcers by cutting the nerve going to the stomach to “turn off” the secretion of hydrochloric acid. As a result, rehabilitation after surgery took many months, and the consequences of such an operation accompanied patients throughout their lives.3
A major breakthrough in therapy occurred in 1989, when a group of Swedish researchers led by Ivan Estholm invented the first proton pump inhibitor4, a molecule that can reduce the production of hydrochloric acid without surgery. This event played a key role in the development of a new approach to the treatment of GERD and marked a breakthrough in the treatment of digestive diseases. In 1993, at the International Congress of Gastroenterologists at Yale, it was decided to abandon vagotomy forever. In 2000, the next generation of PPIs, esomeprazole, was developed and launched on the market, which has been successfully used for the treatment of GERD, gastric and duodenal ulcers in 125 countries around the world for 20 years.4
- Ivashkin V.T., Maev V.I., Trukhmanov A.S. et al. Clinical guidelines of the Russian Gastroenterological Association for the diagnosis and treatment of gastroesophageal reflux disease. RZHGGK. 2017;27(4):75-95
- R. Jones, O. Junghard, J. Dent et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009 Nov 15;30(10):1030-8
- Ivashkin V.T. School of clinician. Peptic ulcer disease - history of medicine. // Medical Bulletin. - 2006. - No. 19 (362). - p. 9-10.
- Olbe L., Carlsson E., Lindberg P. A proton-pump inhibitor expedition: the case histories of omeprazole and esomeprazole. Nat Rev Drug Dis 2003; 2:132-9.
Postoperative regimen and rehabilitation.
On the first day until the evening, due to anesthesia, bed rest is prescribed, in the evening you can drink liquids, turn and sit up in bed, the next day you can get up and walk, take semi-liquid food. All dietary restrictions are lifted after a week. When pyloroplasty is performed simultaneously with vagotomy, the diet is prescribed for a period of up to 2-3 weeks.
During the first two weeks after surgery, wash in the shower; after washing, treat wounds with iodine solution or 5% potassium permanganate solution. Removal of sutures is usually not required. The usual mode of labor and physical work is possible after 3 weeks. See also Postoperative regimen and rehabilitation.
Advantages
The laparoscopic option for performing the intervention is obvious: significantly less trauma, excellent cosmetic effect, virtually no postoperative pain, shorter hospital stay, faster rehabilitation.
To the disadvantages
It can be attributed to the fact that the operation is performed, on average, a little longer (10-20 minutes) than with the open version and requires consumables. For more information, see 18 advantages and 4 disadvantages of laparoscopy.
Gastrointestinal surgery
There are currently no active promotions in this area.
Anesthesiology and resuscitation
| Service code | Internal code | Name | Price, rub |
| B01.003.004.007 | 37.1.1 | Spinal anesthesia lasting up to 1 hour | 8 000 |
| B01.003.004.006 | 37.1.2 | Epidural anesthesia lasting up to 1 hour | 14 000 |
| B01.003.004.008 | 37.1.3 | Spinoepidural anesthesia lasting up to 1 hour | 20 000 |
| B01.003.004.009 | 37.1.4 | Total intravenous anesthesia up to 20 minutes | 6 000 |
| B01.003.004.009 | 37.1.5 | Total intravenous anesthesia from 20 minutes to 60 minutes | 12 000 |
| B01.003.004.010 | 37.1.6 | Endotracheal anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.010 | 37.1.7 | Endotracheal anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.010 | 37.1.8 | Endotracheal anesthesia from 3 hours to 4 hours | 34 000 |
| B01.003.004.010 | 37.1.9 | Endotracheal anesthesia from 5 to 6 hours | 58 000 |
| B03.016.011 | 37.1.10 | Express analysis of blood gases and electrolytes | 2 000 |
| B03.016.011 | 37.1.11 | Advanced express analysis of blood gases and electrolytes | 2 500 |
| B03.016.011 | 37.1.12 | Artificial ventilation for 12 hours | 7 200 |
| B01.003.004.010 | 37.1.13 | Endotracheal anesthesia up to 1 hour | 14 000 |
| B01.003.004.010 | 37.1.14 | Endotracheal anesthesia from 4 to 5 hours | 40 000 |
| B01.003.004.002 | 37.1.15 | Conduction anesthesia of the 1st category of complexity | 4 000 |
| B01.003.004.005 | 37.1.16 | Infiltration anesthesia (large volume or area) up to 30 minutes | 3 000 |
| B01.003.004.005 | 37.1.17 | Infiltration anesthesia up to 15 minutes | 1 400 |
| B01.003.004.004 | 37.1.18 | Application anesthesia | 1 000 |
| B01.003.004.009 | 37.1.19 | Drug sedation with hemodynamic monitoring | 3 000 |
| B01.003.004 | 37.1.20 | Prolonged regional anesthesia (days) | 8 000 |
| A11.12.001 | 37.1.21 | central vein catheterization | 10 000 |
| A11.23.002 | 37.1.22 | TAP TEST | 12 500 |
| B01.003.004.007 | 37.1.1.2 | Spinal anesthesia from 1 hour to 2 hours | 14 000 |
| B01.003.004.007 | 37.1.1.3 | Spinal anesthesia from 2 hours to 3 hours | 17 000 |
| B01.003.004.007 | 37.1.1.4 | Spinal anesthesia from 3 hours to 4 hours | 20 000 |
| A11.23.003.001 | 37.1.2.1 | Placement of an epidural catheter | 8 000 |
| B01.003.004.006 | 37.1.2.2 | Epidural anesthesia from 1 hour to 2 hours | 17 000 |
| B01.003.004.006 | 37.1.2.3 | Epidural anesthesia from 2 hours to 3 hours | 21 000 |
| B01.003.004.006 | 37.1.2.4 | Epidural anesthesia from 3 hours to 4 hours | 24 000 |
| B01.003.004.006 | 37.1.2.5 | Epidural anesthesia from 4 hours to 5 hours | 28 000 |
| B01.003.004.008 | 37.1.3.1 | Spinoepidural anesthesia from 1 hour to 2 hours | 22 000 |
| B01.003.004.008 | 37.1.3.2 | Spinoepidural anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.008 | 37.1.3.3 | Spinoepidural anesthesia from 3 hours to 4 hours | 27 000 |
| B01.003.004.008 | 37.1.3.4 | Spinoepidural anesthesia from 4 hours to 5 hours | 30 000 |
| B01.003.004.009 | 37.1.5.1 | Total intravenous anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.009 | 37.1.5.2 | Total intravenous anesthesia from 2 hours to 3 hours | 24 000 |
| B01.003.004.010 | 37.1.9.1 | Endotracheal anesthesia from 6 to 7 hours | 65 000 |
| B01.003.004.010 | 37.1.9.2 | Endotracheal anesthesia from 7 to 8 hours | 70 000 |
| B01.003.004.002 | 37.1.15.1 | Conduction anesthesia of the 2nd category of complexity | 5 000 |
| B01.003.004.002 | 37.1.15.2 | Conduction anesthesia of the 3rd category of complexity | 6 000 |
Hernia of the anterior abdominal wall (Tyumin A. A.)
| Service code | Internal code | Name | Price, rub |
| A16.30.001 | 37.46.1.1 | Open surgical treatment of inguinofemoral hernia | 90 000 |
| A16.30.002 | 37.46.10.1 | Surgical treatment of umbilical hernia, category 2 | 80 000 |
| A16.30.001.001 | 37.46.2.1 | Laparoscopic surgical treatment of inguinofemoral hernia | 110 000 |
| A16.30.002 | 37.46.4.1 | Surgical treatment of category 2 ventral hernia | 110 000 |
| A16.30.002 | 37.46.9.1 | Surgical treatment of category 1 umbilical hernia | 60 000 |
Gastrointestinal tract
| Service code | Internal code | Name | Price, rub |
| A16.16.010 | 37.39.1 | Gastrotomy | 25 000 |
| A16.16.010 | 37.39.2 | Gastrotomy, stitching of a bleeding stomach ulcer | 66 000 |
| A16.16.010 | 37.39.3 | Gastrotomy, suturing of gastric varicose veins | 100 000 |
| A16.16.015 | 37.39.4 | Gastrectomy (including transthoracic) | 180 000 |
| A16.16.017.004 | 37.39.5 | Proximal gastrectomy | 170 000 |
| A16.16.017.002 | 37.39.6 | Reconstructive gastrectomy | 190 000 |
| A16.16.017.001 | 37.39.7 | Distal gastrectomy | 145 000 |
| A16.16.017.008 | 37.39.8 | Segmental endoscopic gastrectomy | 200 000 |
| A16.16.011 | 37.39.9 | Pyloroplasty | 65 000 |
| A16.16.020 | 37.39.10 | Gastroenterostomy | 90 000 |
| A16.16.021 | 37.39.11 | Suturing of a perforated gastric or duodenal ulcer | 75 000 |
| A16.16.021.001 | 37.39.12 | Laparoscopic suturing of a gastric or duodenal ulcer | 110 000 |
| A16.16.047 | 37.39.13 | Installation of an endogastric balloon (without balloon cost) | 30 000 |
| A16.16.047 | 37.39.14 | Installation of the LAP-BAND system (without the cost of a gastric band | 160 000 |
| A16.16.004 | 37.39.15 | Cardiodilation of the esophagus | 50 000 |
| A16.16.033 | 37.39.16 | Fundoplication | 85 000 |
| A16.16.033.001 | 37.39.17 | Laparoscopic fundoplication | 130 000 |
| A16.16.034 | 37.39.18 | Gastrostomy | 55 000 |
| A16.16.034.001 | 37.39.19 | Laparoscopic gastrostomy | 70 000 |
| A16.16.036 | 37.39.20 | Reconstruction of gastroenteroanastomosis | 160 000 |
| A16.17.001 | 37.39.21 | Excision of small intestinal diverticulum | 50 000 |
| A16.17.005 | 37.39.22 | Small bowel resection | 60 000 |
| A16.30.006 | 37.39.23 | Laparotomy, dissection of adhesions in case of obstruction | 85 000 |
| A16.30.006 | 37.39.24 | Laparotomy for strangulated hernias with resection of a section of the small intestine with nasointestinal drainage | 140 000 |
| A16.17.007 | 37.39.25 | Ileostomy | 48 000 |
| A16.17.009 | 37.39.26 | Release of the small intestine from intussusception | 37 000 |
| A16.17.010 | 37.39.27 | Enetrotomy, removal of a foreign body | 50 000 |
| A16.18.004 | 37.39.28 | Total colectomy | 250 000 |
| A16.18.015 | 37.39.29 | Left hemicolectomy | 180 000 |
| A16.18.016 | 37.39.30 | Right hemicolectomy | 180 000 |
| A16.18.017.003 | 37.39.31 | Laparoscopic hemicolectomy | 250 000 |
| A16.19.019 | 37.39.32 | Resection of the sigmoid colon | 120 000 |
| A16.19.021.005 | 37.39.33 | Low anterior rectal resection | 250 000 |
| A16.19.021.010 | 37.39.34 | Anterior rectal resection | 170 000 |
| A16.19.020.003 | 37.39.35 | abdominoperineal extirpation of the rectum | 250 000 |
| A16.18.007 | 37.39.36 | Colostomy | 40 000 |
| A16.18.009 | 37.39.37 | Open appendectomy 1 stage | 50 000 |
| A16.18.009 | 37.39.38 | Open appendectomy 2nd stage | 70 000 |
| A16.18.009 | 37.39.39 | Open appendectomy 3rd stage | 110 000 |
| A16.18.009.001 | 37.39.40 | Laparoscopic appendectomy 1st stage | 60 000 |
| A16.18.009.001 | 37.39.41 | Laparoscopic appendectomy category 2 | 80 000 |
| A16.18.009.001 | 37.39.42 | Laparoscopic appendectomy category 3 | 115 000 |
| A16.17.010 | 37.39.43 | Colotomy, foreign body removal | 50 000 |
| A16.18.012 | 37.39.44 | Formation of intestinal bypass anastomosis 1st stage | 55 000 |
| A16.18.012 | 37.39.45 | Formation of intestinal bypass anastomosis 2nd stage | 80 000 |
| A16.19.026 | 37.39.46 | Reconstructive surgery on the colon | 150 000 |
| A16.19.021.015 | 37.39.47 | transanal full-wall tumor excision | 150 000 |
| A16.18.028.001 | 37.39.48 | Laparoscopic removal of colonic fat pad | 50 000 |
| A16.16.034.003 | 37.39.49 | Percutaneous endoscopic gastrostomy (excluding cost of gastrostomy kit) | 30 000 |
General hospital services
| Service code | Internal code | Name | Price, rub |
| S01.001.001 | 37.0.1 | Stay in a hospital ward (daily) | 6 000 |
| S01.001.002 | 37.0.2 | Stay in a hospital ward (daytime until 21:00) | 3 000 |
| S01.001.003 | 37.0.3 | Stay in the ward for accompanying persons (daily) | 6 000 |
| S01.001.004 | 37.0.4 | Stay in hospital room VIP 1 (daily) | 10 000 |
| S01.001.005 | 37.0.5 | Stay in hospital room VIP 2 (daily) | 16 000 |
| S01.001.006 | 37.0.6 | Stay in a hospital ward (daily, without meals) | 3 400 |
| S01.001.007 | 37.0.7 | Stay in the intensive care unit from 6-24 hours | 8 000 |
| B01.047.009 | 37.0.9 | Supervision by a therapeutic physician (1 visit) | 2 500 |
| A11.12.003 | 37.0.10 | Infusion therapy of expensive drugs | 4 000 |
| A23.01.001 | 37.0.11 | Extraction of surgical material using delivery means (calculated price) | 1 000 |
| A18.05.013 | 37.0.22 | Treatment using blood products (calculation, price) | 1 000 |
| A11.12.003 | 37.0.23 | Treatment using additional drug therapy (calculation, price) | 1 000 |
| A23.01.001 | 37.0.24 | Selection of implants (calculation, price) | 1 000 |
| S01.002.001 | 37.0.25 | Selection of compression garments (calculation, price) | 1 000 |
| B01.057.001 | 37.0.28 | Appointment with an operating specialist | 0 |
| A11.01.014 | 37.0.29 | Hemostasis using local hemostatic agent Zhelplastan 2.5 g | 6 600 |
| A11.01.014 | 37.0.30 | Hemostasis using local hemostatic agent Zhelplastan 5.0 g | 12 700 |
| A11.12.003.002 | 37.0.31 | IV drip infusion of Ferinject 500 mg (Ferinject, 50 mg/ml, 2 ml No. 5 in ampoules or 50 mg/ml, 10 ml in a bottle), duration up to 30 minutes | 8 000 |
| А11.12.003.003 | 37.0.32 | IV drip infusion of Ferinject 1000 mg (Ferinject, 50 mg/ml, 10 ml in bottle No. 2), duration up to 30 minutes | 15 000 |
| S01.001.008 | 37.0.1.1 | Stay in a hospital room (overnight) | 3 000 |
| S01.001.009 | 37.0.4.1 | Stay in hospital room VIP 1 (no more than 12 hours) | 5 000 |
| S01.001.010 | 37.0.5.1 | Stay in hospital room VIP 2 (no more than 12 hours) | 8 000 |