Chronic granulomatous inflammation of any part of the gastrointestinal tract (from the oral cavity to the anus, but most often the small intestine is affected in the form of segmental enteritis in 75-80% of patients), and the process begins in the final part of the small intestine - the ileum. The growth of the disease is observed all over the world, Crohn's disease affects mainly the working population, is difficult to diagnose, is reluctant to treat, and can lead to severe complications, disability, and loss of ability to work.
Crohn's disease. Causes
The causes of Crohn's disease are unknown; it is based on an immunological reaction in the intestinal mucosa, resulting in the development of a granulomatous inflammatory process.
The role of infectious factors was considered - according to modern concepts, this is a multifactorial disease with a genetic predisposition, a violation of immunoregulation with an autoimmune component, which allows the implementation of unknown damaging agents (bacterial agents, bacterial endotoxins, autoantigens).
Causes
Predisposing factors for the development of the disease are:
- previous viral infection (measles);
- food allergies;
- stress and mental strain;
- smoking;
- hereditary predisposition.
To date, the causative agent of Crohn's disease has not been identified. However, the infectious theory is the main version of the origin of the disease. This is explained by the positive effect of treatment with antibacterial drugs. In addition, disorders of the immune system play an important role in the development of the disease. Autoimmune processes, in which antibodies are produced against one’s own intestinal tissues, and the insufficiency of the protective function of the immune system are an important link in the origin of the disease.
Crohn's disease. Signs
Clinical manifestations or signs of Crohn's disease depend on the location of the process, but the following are common to it:
- diarrhea (diarrhea),
- abdominal pain,
- fever,
- long-term anemia of “unexplained origin”,
- weight loss,
- extraintestinal lesions.
Crohn's disease. Intestinal manifestations
Diarrhea is the most typical symptom of Crohn's disease, occurring in 70-80% of cases of Crohn's disease of the small intestine, ileum of the small intestine and colon.
Pain is the next most common symptom of Crohn's disease. “Stomach hurts and diarrhea”, “stomach hurts and I often go to the toilet” are the most common complaints of patients. There are different localizations and different types of pain:
- Severe cramping pain after eating (gastrointestinal syndrome with increased intestinal motility), complaints of “sharp pain after eating.”
- Dull, constant pain in the abdomen due to the spread of the inflammatory process throughout the entire thickness of the intestinal mucosa with the formation of adhesions with surrounding organs. So they complain: “constant dull abdominal pain”
- When the jejunum is affected, pain is most often localized in the left upper quadrant of the abdomen. Complaints of “abdominal pain in the upper left.”
- When localized in the ileum of the small intestine - in the right iliac region. They say “pain in the hypochondrium after eating.” In this regard, patients are often hospitalized and operated on for appendicitis, but an accurate diagnosis is established during the operation.
Fever in combination with abdominal pain at the site of the lesion (“fever and abdominal pain”) indicates the formation of infiltrates of the abdominal cavity, which is confirmed by laboratory tests that detect acute inflammation.
In 5% of patients, lesions of other organs of the gastrointestinal tract are detected - the oral mucosa, esophagus, stomach with the formation of erosive and ulcerative processes.
Extraintestinal manifestations of Crohn's disease:
- joint damage,
- rheumatoid arthritis,
- ankylosing spondylitis,
- skin lesions (erythema nodosum, eczema, furunculosis),
- eye damage (conjunctivitis, keratitis, etc.).
The severity of Crohn's disease is usually assessed by the activity index. The possibility of developing complications is determined by the results of a morphological study, the depth of damage to the intestinal wall, and the activity of the process. With Crohn's disease of the small intestine, abscesses, intestinal fistulas, and adhesions can form, complicated by intestinal obstruction.
Complications
Crohn's disease is dangerous not only for its unpleasant manifestations, but also for its severe complications that can only be eliminated surgically. These include:
- Perforation of the intestinal wall, with the addition of peritonitis;
- Intestinal obstruction;
- Heavy bleeding;
- External and internal fistulas, ulcers;
- Inflammatory infiltrates and strictures (narrowing of the lumen) of the intestine;
- Risk of adenocarcinoma;
- Weeping cracks and maceration of the rectum;
- Foci of suppuration (abscesses).
Crohn's disease is characterized by a chronic, long-term course; exacerbations of the disease can continue throughout the patient's life. The course of the disease in each specific case is different and in some patients the symptoms may be mild and not particularly affect their well-being, while in others the exacerbation of the disease may be accompanied by severe, life-threatening complications.
Crohn's disease - diagnosis
Diagnostic algorithm for Crohn's disease:
- endoscopic examination (colonoscopy) with examination of the ileum of the small intestine, a biopsy of the mucous membrane of this section of the intestine is required,
- endoscopic examination of the upper gastrointestinal tract - gastroscopy of the esophagus, stomach, duodenum - even in the absence of complaints from these organs,
- X-ray examination of the entire gastrointestinal tract is mandatory to identify the location of the lesion, foci of inflammation, adhesions, strictures, and filling defects. X-ray examination of the small intestine is the main instrumental method that allows, with a certain degree of probability, to confirm the diagnosis of “Crohn’s disease”,
- general clinical examination: clinical blood test, diagnosis of anemia (primarily B12 deficiency), expanded blood biochemistry with indicators of acute inflammation, examination of protein, carbohydrate, calcium metabolism, which is necessary if digestion and absorption in the small intestine are impaired,
- bacteriological and serological studies to exclude acute intestinal infections,
- bacteriological and scatological examination of stool,
- calprotectin in feces.
Operation
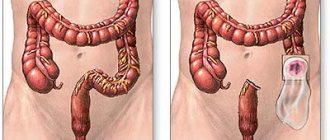
If diet, lifestyle changes, drug therapy and other methods are ineffective, the patient is recommended to undergo surgical treatment. About half of all Crohn's disease patients undergo at least one surgical procedure during treatment. However, this does not provide a cure for the disease.
Surgical treatment consists of removing the damaged section of the intestine, followed by an anastomosis between healthy areas. Surgery is also necessary to treat fistulas and drain abscesses, as well as in the development of intestinal obstruction.
The positive effect of surgical treatment for Crohn's disease is usually temporary. The disease often recurs, causing inflammation near the previous site. The best policy is to continue supportive drug therapy after surgery.
Crohn's disease - treatment and prognosis
Mild forms of Crohn's disease are treated on an outpatient basis; severe cases are treated in a hospital and observed by proctologists.
The treatment complex includes: therapeutic nutrition (as for chronic enteritis, individual, long-term). Basic therapy is carried out with drugs gr. Mesalazine, Pentase, depending on the location and activity of the process for a long time. According to indications, hormonal therapy is used until stable remission. Symptomatic therapy is carried out (chronic enteritis).
With segmental damage to the small intestine, the prognosis is favorable with prolonged drug treatment, and less favorable with complications of Crohn's disease.
Read about therapeutic nutrition for diseases of the small intestine, including Crohn's disease, here.
Diet
In combination with drug therapy, doctors pay great attention to a special diet, which is very important for reducing mechanical, thermal and chemical irritation of the intestines. The diet for Crohn's disease is not very strict, the main thing in it is respect for the intestines.
Prohibited products for this disease include:
- All types of legumes, mushrooms;
- Pasta, flour and confectionery products;
- Ice cream;
- Any spices, seasonings, hot sauces, mustard;
- Fatty fish and meats;
- Porridge made from pearl barley or millet;
- Chips, crackers, canned food, semi-finished products;
- Carbonated and cold drinks;
- Coffee, chocolate, strong tea;
- Pickles and smoked meats;
- Spicy, fried foods;
- Alcohol.
Eating hot food is not recommended; all dishes are served warm, with a serving temperature of at least 18°C and no more than 60°C. Meals should be fractional, food should be taken in small portions 5-6 times a day.
Mode
During exacerbations - inpatient, in the stage of remission - outpatient.
Diet
During the period of exacerbation of the disease, a mechanically and chemically gentle diet is prescribed with a high content of proteins, vitamins, the exclusion of milk in case of intolerance and a limited amount of coarse plant fiber, especially when sections of the intestine are narrowed (diet No. 4, then No. 4b). The calorie content of food can be increased through liquid nutrient solutions, protein preparations containing whole protein and devoid of lactose and plant fiber, special diets including hydrolyzed protein, also devoid of lactose and fiber. In case of strictures or repeated obstructions, the intake of rough and gas-forming foods should be avoided. For various forms of diarrhea, it is necessary to increase the amount of plant fiber and limit fat intake.
Observation
Dynamic observation, control examination every 3–6 months if the patient’s condition is stable (Hb level, ESR, body weight, pain, diarrhea, systemic manifestations). Control colonoscopy with biopsy of suspicious areas of the mucous membrane. Annually - biochemical blood test, liver tests, proteinogram. Determination of vitamin B12 content in the small intestinal form of the disease or after resection of a segment of the small intestine.
When to see a doctor
People should see a doctor if they experience the following symptoms:
- diarrhea that lasts longer than 7 days;
- frequent stomach pain and discomfort;
- blood in stool;
- unexplained weight loss.
In most cases, Crohn's disease requires lifelong treatment. You should see your doctor regularly and take any prescribed medications as directed.
We also recommend reading - What is the difference between Crohn's disease and ulcerative colitis?
Causes
Risk factors
- Genetic factors. In approximately 17% of cases, Crohn's disease is detected among the patient's immediate relatives (first degree of relationship). Predisposition to the development of inflammatory bowel diseases (Crohn's disease and ulcerative colitis) is determined by loci 12p13.2, 12q24.1, 7q22 and 3p21.2;
- Chronic inflammatory bowel diseases;
- Ileocecal valve insufficiency;
- Dysbacteriosis.
Pathomorphology Significant thickening of the affected intestinal wall with transmural inflammation. Characterized by a multiplicity of lesions (focal granulomas, deep convoluted or linear ulcerations), spaced at a great distance from each other. In this regard, the spread of the disease is figuratively compared to the jumping of a kangaroo.
Macroscopically: the appearance of a “cobblestone street” - areas of normal mucous membrane are replaced by ulcerations and granulomatous growths.
Microscopically: In the affected area there is edema and hyperplasia of lymphatic follicles in the submucosa. Proliferation of reticuloendothelial and lymphoid elements. Granulomas consisting of giant and epithelioid cells. Enlarged, dull mesenteric lymph nodes on section. Secondary strictures due to scarring, possible formation of fistulas.