What is a small intestinal ulcer: description of the pathology
A small intestinal ulcer is a lesion of the mucous and submucosal layer of the intestinal wall with the formation of a defect. The name has several synonyms - nonspecific, idiopathic, round, simple, etc.
Often the disease is asymptomatic for a long time, so it is diagnosed after it has become chronic. During the pathology, relapses (exacerbations) are replaced by periods of remission.
Most often, signs of intestinal ulcers are found in men 30-60 years old.
Classification
In the international classification ICD 10, the disease is coded as K63.3 - intestinal ulcer or primary ulcer of the small intestine.
Full explanation of the diagnosis:
- K00-K93 - diseases of the digestive system;
- K55-K63 - other intestinal diseases;
- K63 - other intestinal diseases;
- K 63.3 - intestinal ulcer.
Complications
They are quite rare (up to 3-5% of cases), but have a high incidence of deaths (up to 90%).
Complications include:
- Perforation of an ulcer (perforation) is a rupture of the intestinal wall with the release of contents into the abdominal cavity. Depending on the location of the perforation, diffuse or local peritonitis (inflammation of the peritoneum) may develop.
- Intestinal bleeding - develops when the vessels supplying the small intestine are damaged. Minor bleeding may occur without obvious symptoms. They are detected during laboratory tests (traces of blood are found in the stool). More massive bleeding is accompanied by changes in stool (melena - tarry stool), hemodynamic disturbances (increased heart rate, decreased blood pressure). A picture of posthemorrhagic anemia develops.
- Cicatricial narrowing of the lumen of the small intestine (stenosis) - slowing down the passage of the food bolus until the development of intestinal obstruction.
Complications most often develop in patients who have undergone surgery on the abdominal organs. Such conditions require emergency surgery.
Causes
The exact causes of primary small intestinal ulcers have not been established. Some provoking factors influencing the appearance of pathology have been identified.
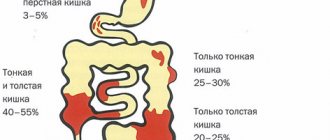
Anatomy of the small intestine (briefly about the departments)
The small intestine is the longest part of the digestive tube. In an adult, its length is 5-6 m. Anatomically, the organ consists of 3 sections - duodenum, jejunum and ileum. The length of the jejunum is approximately 2/5 of the total length of the small intestine.
There is no clear boundary between these sections; the ileum can be distinguished by:
- larger diameter;
- abundant blood supply;
- position on the right side of the midline of the human body.
The pylorus separates the small intestine from the stomach and the ileocecal valve from the large intestine.
Factors influencing the appearance and development of diseases of the small intestine
Factors that provoke diseases of the small intestine largely coincide with those in other parts of the digestive tract. These include:
- smoking and alcohol abuse;
- unbalanced diet with a violation of the regime - abuse of fatty, spicy and salty foods, snacks on the go, overeating or prolonged fasting, etc.;
- diseases associated with impaired hormone production (endocrine) - diabetes mellitus, hyperparathyroidism, etc.;
- atherosclerosis and other concomitant vascular diseases;
- abdominal injuries.
The risk increases in men aged 30-60 years, as well as patients suffering from other gastrointestinal diseases.
Common Causes of Small Intestinal Diseases
An ulcer can occur against the background of other acute and chronic diseases of the small intestine.
The causes may be:
- bacterial and viral infections, helminthiases;
- acute and chronic intoxication, including alcohol and drugs;
- autoimmune diseases;
- abdominal injuries;
- chronic diseases of the pancreas and biliary tract.
Predisposing factors include genetic predisposition, abuse of spicy and fatty foods, concomitant chronic diseases, and congenital intestinal abnormalities.
What causes the disease?
The most common sign of an infectious lesion is considered to be Yersinia infestation. In rare situations, such a disease occurs for the following reasons:
- Presence of salmonella.
- Presence of E. coli.
- Development of staphylococcal cells.
There is also a severe viral process that occurs as a result of exposure to rotovirus elements, as well as enteroviruses. Giardia parasites and worms can lead to the chronic type. The main factors causing such a negative effect in the human body include:
- Alcohol abuse.
- Tobacco addiction.
- Regular intake of fatty and spicy foods.
- Intoxication of the body with heavy metals, toxic substances and chemicals.
- Genetic predisposition.
- Surgical intervention in the intestinal area.
- Taking medications.
Symptoms of small intestinal ulcers in adults and children
All symptoms of ulcers are divided into intestinal and general (extraintestinal). The clinical picture depends on age - it may differ slightly in adults and children.
- Abdominal pain
- Heartburn
- Flatulence
- Vomit
- Nausea
Intestinal manifestations
In the early stages, a small intestinal ulcer may be asymptomatic. If a mucosal defect occurs against the background of an inflammatory process, the symptoms of the underlying disease (duodenitis, enteritis) come to the fore.
There are general intestinal symptoms and signs characteristic of damage to the small intestine.
General symptoms of intestinal ulcers
These clinical signs of intestinal ulcers are characteristic of all parts. These include:
- Abdominal pain. It can be constant aching or cramping, intensifying after eating.
- Vomiting - can be repeated, intensifies after eating. Relief after vomiting does not always occur.
- Nausea, heartburn.
- Increased gas formation in the intestines (flatulence).
- Diarrhea (loose stools). A characteristic symptom of a complicated intestinal ulcer is blood in the stool. The stool takes on a black, tarry appearance (melena).
If the ulcer occurs after surgery (pyloroplasty with vagotomy), it may be asymptomatic or atypical.
Signs of ulcers of the small and jejunal intestines
Damage to the jejunum is characterized by pain in the upper abdomen. Often it radiates to the spine, navel area or left half of the chest.
Initially, pain occurs 3-4 hours after eating. As the process becomes chronic, it becomes permanent.
The symptoms and treatment of intestinal ulcers in adults and children have some differences. In a child, the pathology is often asymptomatic or accompanied by dyspeptic disorders - diarrhea, nausea, bloating.
With a perforated ulcer, the pain becomes sharp and unbearable (dagger-like). It can occur in the upper or lower abdomen and is accompanied by uncontrollable, painful vomiting.
The pulse is slow at first, then increases sharply. The abdomen becomes tense (board-shaped).
Extraintestinal manifestations
The main function of the small intestine is to absorb substances needed by the body from food. When the mucous membrane is damaged, this function is disrupted, which causes the development of extraintestinal manifestations:
- Insufficient absorption of proteins and lipids leads to significant weight loss.
- Deficiency of vitamin B12, iron, and folic acid causes the development of chronic anemia.
- A lack of vitamins is manifested by cracks and jams in the corners of the mouth, dry skin, hair loss, and impaired twilight vision.
- The absorption of calcium and phosphorus is impaired, which leads to frequent fractures.
If the ulcer develops in childhood, normal growth and development are affected. In women, a sign of advanced intestinal ulcers may be menstrual irregularities.
What symptoms are accompanied by ileitis?
The characteristic symptoms of the described illness are:
- Discomfort and pain in the iliac region.
- Bloating and rumbling in the peritoneum.
- Passing liquid stool for more than a week.
- Nausea reflex.
- Vomiting.
- Increased body temperature.
- General weakness and fatigue.
- Acute pain in the head area.
Chronic ileitis is accompanied by patient complaints such as:
- Moderate pain in the iliac region and near the navel.
- Watery stool with remnants of incompletely digested food.
- Rapid weight loss.
- Development of diseases of hypovitaminosis and osteoporosis.
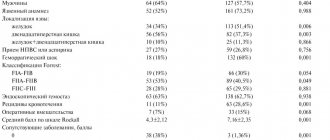
Diagnostic features
The clinical picture of a small intestinal ulcer is nonspecific, so making an accurate diagnosis can be difficult.
The algorithm includes:
- Interviewing the patient, collecting complaints and medical history.
- Physical examination, palpation of the abdomen.
- Lab tests.
- Instrumental research.
Differential diagnosis is carried out with secondary ulcers (for tuberculosis, typhoid fever), damage to the large intestine, and gastric ulcers.
Data collection and inspection
The examination begins with the collection of complaints and medical history. During a conversation with the patient or his relatives, the doctor finds out:
- The nature of the complaints is the severity of pain, the connection with food intake, physical activity and other factors, the presence of nausea and vomiting, and extraintestinal manifestations.
- How long ago did the complaints appear, how did the symptoms develop?
- Do the patient’s immediate blood relatives suffer from gastrointestinal diseases?
- How does a person eat, what foods predominate in the diet.
- What concomitant diseases, injuries, surgeries did he undergo?
During the examination, pay attention to the general condition, body weight (in patients with damage to the small intestine it is usually reduced). The skin is dry and pale, and there may be “seals” in the corners of the mouth.
Palpation of the abdomen reveals tension in the abdominal wall, local pain in the epigastric region or upper right.
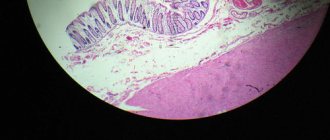
Instrumental studies
Endoscopic examination can identify ulcers. Diagnosis is carried out using a flexible endoscope and a miniature video camera. If necessary, a tissue sample can be taken for histological examination.
Examination of patients with ulcers of the jejunum and ileum is significantly difficult due to the anatomical features of these organs. Standard research methods (radiography, endoscopic methods) make it possible to identify pathology of the duodenum, but do not allow assessing the condition of the small intestine.
Experts call a relatively new method, capsule endoscopy, more effective. A special “video capsule” is introduced into the body, which moves through the intestines and takes a large number of pictures. The data is transferred to the recording device.
The effectiveness of such diagnosis may be reduced if the ulcerative defect is located in a fold or there is an area of stenosis in the intestine. Laparoscopic surgery and ultrasound of the abdominal organs help diagnose complicated ulcers.
Laboratory research
There are no specific laboratory tests that can identify an ulcer with 100% certainty. However, there are indirect signs that, in combination with complaints and instrumental studies, confirm the diagnosis:
- in a general blood test - a decrease in hemoglobin level (with anemia, lack of absorption of nutrients);
- in a general urine test - an increase in the amount of calcium (with hyperparathyroidism);
- in biochemical analysis – hypoproteinemia (decreased amount of protein);
- in the coprogram - altered red blood cells (a sign of bleeding).
For gastrojejunal ulcers, a test is performed for Helicobacter pylori, a bacterium that provokes an inflammatory and erosive-ulcerative process in the stomach and intestines.
Treatment methods
The choice of treatment tactics depends on the cause of the ulcer, its location, the presence of complications and other factors. A prerequisite for successful therapy is the prescription of a diet.
Conservative methods can cure simple, uncomplicated ulcers. They include medications and folk remedies. If conservative measures are ineffective or complications develop, the pathology is treated surgically.
Drug therapy
Drug treatment of intestinal ulcers is aimed at eliminating the cause, restoring intestinal functions and eliminating extraintestinal manifestations. To combat ulcers, the following are prescribed:
- Antibacterial agents - amoxicillin, clarithromycin, metronidazole, etc.
- Drugs that restore normal intestinal microflora - Lactobacterin, Bifikol.
- Astringents and enveloping agents – “Sucralfate”, “Almagel”, etc.
- Adsorbent – “Polyphepan”, “Enterodes”.
- Antidiarrheal drugs – “Smecta”, “Ectoban”.
To correct extraintestinal disorders, protein and saline solutions, complexes of vitamins and microelements, and iron preparations are used. Medicines are taken in tablets, injections and intravenous drips.
Surgery
Surgical treatment methods are used when medications are ineffective, as well as the development of complications - perforated ulcers, massive bleeding, stenosis with the development of intestinal obstruction, peritonitis.
Types of operations
The type of surgical treatment for symptoms of intestinal ulcers in adults depends on the location and number of defects, the nature of complications, age and general condition of the patient.
Main types of operations:
- excision of ulcerative defect;
- resection of part of the small intestine (for multiple lesions);
- suturing large single ulcers.
When peritonitis develops, the abdominal cavity is washed and drained.
Laparoscopic methods are widely used - the introduction of microsurgical equipment and video cameras into the abdominal cavity. Laparoscopy is not used for severe bleeding or perforated ulcer with peritonitis.
Recovery period
On the 1st day after surgery, the patient is prohibited from eating and drinking. Painkillers are administered according to indications. To restore protein and water-salt balance, parenteral nutrition is prescribed (all substances needed by the body are administered intravenously).
On days 3-4 the patient is transferred to therapeutic diet No. 1a, then 1b. Slimy soups and cereals, vegetable purees are introduced into the diet.
After 5-7 days (subject to a favorable recovery period), it is allowed to eat stewed, boiled and baked vegetables, lean meat and fish, and low-fat low-fat dairy dishes.
The average length of hospital stay is from 10 to 14 days.
Traditional methods
You can be treated with traditional recipes at home with the permission of the attending physician and under his supervision.
The most effective natural remedies for home treatment are:
- fresh potato and cabbage juice - drink ½ glass in the morning;
- water tincture of propolis – take according to the schedule for 2 weeks;
- aloe juice with honey - drink 1 tablespoon before meals;
- collections of medicinal herbs - yarrow, chamomile, St. John's wort, etc.
It is important to remember that folk remedies do not replace taking medications. To avoid the development of complications, it is necessary to simultaneously treat the intestinal ulcer with drugs prescribed by the doctor.
Diet therapy
Nutrition for intestinal ulcers should be gentle. During an exacerbation on the 1st day, fasting and drinking plenty of fluids (weak tea, rosehip decoction, still water) are recommended.
As the symptoms of an intestinal ulcer subside, slimy soups and cereals, vegetable purees, and low-fat dairy products are introduced into the diet. It is allowed to eat boiled, stewed or baked foods.
Avoid foods with coarse fiber, spicy and salty foods, alcoholic drinks, chocolate and coffee.
Treatment of the disease
At the first stage of the disease, treatment is carried out medically through the use of painkillers, anti-inflammatory, bactericidal, and hormonal drugs. Treatment must be accompanied by giving up bad habits, as well as following a special diet. Further, after the treatment, a person’s life is subject to a schedule in compliance with the time of taking medications and drugs.
If the patient's condition worsens, then in order to further cleanse the body, the patient is given a plasma transfusion. In the most severe cases of the disease, the patient cannot avoid surgical intervention in the process. Only in this way will it be possible to cleanse the intestinal mucosa, remove scars formed and the small or large intestine affected by infection and inflammation. After the operation, the patient must be under the supervision of specialists for several years.
Oncological processes and small intestinal ulcers
Oncological diseases of the small intestine are rare and account for no more than 1% of all cases of malignant tumors. The exact reasons for the development are unknown. However, it has been proven that cancer often develops against the background of chronic inflammatory and erosive-ulcerative lesions.
Alertness and risk groups
There are categories of the population with an increased risk of developing intestinal cancer. These include people:
- susceptible to bad habits and addictions (alcohol, smoking);
- those who violate their diet, often snack on the go, and abuse spicy and fatty foods;
- suffering from chronic diseases of the stomach and intestines.
Hereditary predisposition also matters.
Precautions and prevention
Preventive measures will help reduce the risk of developing intestinal tumors. These include maintaining a healthy lifestyle and proper nutrition, regular preventive examinations, treatment of inflammatory and erosive-ulcerative processes in the intestines.