Stomach ulcer (Gastric ulcer)
Stress ulcers
Stress ulcers occur after severe injuries, acute diseases of various organs, severe operations, terminal conditions (shock, collapse), acute renal or liver failure, severe tissue hypoxia.
When exposed to multiple stress factors, the likelihood of developing a stress gastric ulcer increases markedly. The development mechanism is an imbalance in the influence of factors that damage the mucous membrane and factors that protect it. In a situation where all organs and systems are operating in emergency mode, there is a significant release of corticosteroids and catecholamines into the blood, which increase the secretory activity of the mucosal glands and, at the same time, reduce its protective properties. The trophism of the stomach tissues is also disrupted, hemorrhages of the wall are formed, which in turn contributes to ulceration of the mucous membrane. Stress ulcers are localized mainly in the walls of the body and fundus of the stomach. Very rarely they form in the duodenum.
Types of stress ulcers:
- in case of severe damage to the body by burns and the development of burn disease, the resulting stress ulcer is called a Curling ulcer;
- Cushing's ulcer occurs as a result of severe damage to the central nervous system (traumatic brain injury, brain surgery, stroke);
- a distinction is also made between ulcers after myocardial infarction and traumatic ulcers.
Damage to the gastric mucosa such as erosions and ulcers occurs in half of the cases of these conditions, but in most patients a stress ulcer is not diagnosed, since after the condition improves and the underlying pathology that served as a stress factor is cured, the ulcer heals on its own. However, with prolonged exposure to a damaging situation, ulceration of the mucous membrane can be deep and lead to perforation of the stomach wall with the development of peritonitis.
Drug-induced ulcers
Drug-induced or drug-induced ulcers occur as a result of taking drugs that have gastrotoxic side effects. Most anti-inflammatory drugs (corticosteroid hormones, non-steroidal anti-inflammatory drugs), sulfonamides, potassium chloride, caffeine, glucocorticoids, digitalis preparations, anticoagulants, nitrofurans have an ulcerogenic (ulcer-causing) effect.
The mechanism of damage to the mucous membrane also varies from drug to drug; it can be a direct damaging effect (potassium chloride) or indirect: a decrease in the protective properties of the mucosa when the production of gastroprotective prostaglandins is suppressed (non-selective anti-inflammatory drugs of the hormonal and non-hormonal series), increased secretion of gastric juice (glucocorticosteroids, reserpine, caffeine), suppression of normal trophism of the gastric wall. Most drugs combine direct damage to the mucosa with an indirect effect.
As a rule, after discontinuation of drug therapy with ulcerogenic drugs, ulcerations and erosions of the mucous membrane heal safely. However, the danger of ulcers is that they can be complicated by bleeding and perforation of the stomach wall.
In case of gastritis and peptic ulcer of the stomach or duodenum, the administration of ulcerogenic drugs can provoke the development of an exacerbation of the disease; therefore, for such patients, drugs with gastrotoxic side effects are prescribed only when absolutely necessary and with caution, accompanying therapy with gastroprotective drugs.
Ulcers due to hyperparathyroidism
Excessive production of parathyroid hormone by the parathyroid glands is called hyperparathyroidism. These hormones are responsible for regulating calcium metabolism in the body, but one of the effects of parathyroid hormone is to increase the production of hydrochloric acid by the glands of the gastric mucosa. Excess calcium ions in the blood also stimulates the secretion of acid and gastrin. With hyperparathyroidism, ulcers often occur on the mucous membrane of the duodenum. In the stomach they are characterized by antral localization.
The course of a hyperparathyroid ulcer is quite severe, with frequent pain, does not respond well to conservative treatment, is prone to relapse and is often complicated by bleeding and perforation of the stomach wall. Often, ulceration of the gastric mucosa can be complicated by diseases of the digestive system: cirrhosis of the liver, pancreatitis. Ulcers can also occur as a consequence of chronic diseases of the respiratory and excretory systems, and with diabetes mellitus.
Gastric ulcer has the same development mechanisms as duodenal ulcer and is also classified.
Chronic ischemic disease of the digestive organs: diagnostic and treatment algorithm
About the article
31813
0
Regular issues of "RMZh" No. 9 dated April 29, 2010 p. 544
Category: Gastroenterology
Authors: Zvenigorodskaya L.A. 1, Samsonova N.G. , Toporkov A.S. 1 State Budgetary Institution "Moscow Clinical Scientific and Practical Center" of the Moscow Healthcare Department
For quotation:
Zvenigorodskaya L.A., Samsonova N.G., Toporkov A.S. Chronic ischemic disease of the digestive system: algorithm for diagnosis and treatment. RMJ. 2010;9:544.
Chronic ischemic disease of the digestive organs (CHD) is a disease that occurs when blood circulation is impaired along the unpaired visceral branches of the abdominal aorta (celiac trunk, superior and inferior mesenteric arteries), clinically manifested by abdominal pain, usually occurring after meals, disorders of the motor-secretory and absorption intestinal function and, in some patients, progressive weight loss [1]. The terminology of chronic abdominal ischemia is varied. There are more than 20 terms that define this symptom complex. The most famous of them are: “angina abdominalis”, “mesenteric arterial insufficiency”, “chronic intestinal ischemia”, “abdominal ischemic syndrome”. Many doctors know what this condition is, but not everyone understands its etiology, clinical manifestations, or is not fully proficient in the correct diagnostic and clinical algorithms for the management of CIBOP. This may be due to the fact that CIBOP is usually considered a rare and difficult to diagnose disease [1–3]. However, research by A.V. Pokrovsky (1988) showed that lesions of the unpaired visceral branches of the abdominal aorta occur in 73.5% of cases in persons with atherosclerosis of the coronary arteries of the heart, arteries of the brain, as well as in persons with arterial hypertension [4]. Valentine RJ et al. (1991) in 30% of examined patients with arterial hypertension and coronary heart disease, aortography also revealed atherosclerotic lesions of the celiac trunk and superior mesenteric artery [5].
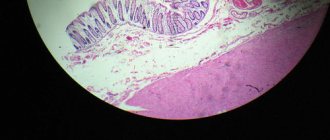
Chronic ischemic disease of the digestive organs (CHD) is a disease that occurs when blood circulation is impaired along the unpaired visceral branches of the abdominal aorta (celiac trunk, superior and inferior mesenteric arteries), clinically manifested by abdominal pain, usually occurring after meals, disorders of the motor-secretory and absorption intestinal function and, in some patients, progressive weight loss [1]. The terminology of chronic abdominal ischemia is varied. There are more than 20 terms that define this symptom complex. The most famous of them are: “angina abdominalis”, “mesenteric arterial insufficiency”, “chronic intestinal ischemia”, “abdominal ischemic syndrome”. Many doctors know what this condition is, but not everyone understands its etiology, clinical manifestations, or is not fully proficient in the correct diagnostic and clinical algorithms for the management of CIBOP. This may be due to the fact that CIBOP is usually considered a rare and difficult to diagnose disease [1–3]. However, research by A.V. Pokrovsky (1988) showed that lesions of the unpaired visceral branches of the abdominal aorta occur in 73.5% of cases in persons with atherosclerosis of the coronary arteries of the heart, arteries of the brain, as well as in persons with arterial hypertension [4]. Valentine RJ et al. (1991) in 30% of examined patients with arterial hypertension and coronary heart disease, aortography also revealed atherosclerotic lesions of the celiac trunk and superior mesenteric artery [5]. Difficulties in diagnosing damage to the visceral arteries are due to the fact that the clinical manifestations of CIBOP are characteristic of various diseases of the gastroduodenal zone, gallbladder, pancreas and intestines. These patients are more often hospitalized in gastroenterological hospitals, where the identified functional and morphological changes in the digestive organs are regarded as banal chronic inflammation, and therapy carried out accordingly is ineffective. The reasons leading to CIBOP are quite clearly and definitely divided into two groups. The first consists of arterial diseases (atherosclerosis, nonspecific aortoarteritis, anomaly of vascular development, angiopathy, etc.). The second group includes extravascular compression of the celiac trunk and mesenteric arteries by the medial leg and falciform ligament of the diaphragm, nerve ganglia of the solar plexus, periarterial fibrous tissues, and tumors. Intravasal lesions are more common (62–90%) than extravasal lesions (10–38%) [6,7]. Among intravasal causes of lesions of the visceral arteries, the first places belong to atherosclerosis (52.2–88.3%) and nonspecific aortoarteritis (22–31%). The most common cause of extravasal compression is the arcuate ligament of the diaphragm or its medial crura (40.8–72.5%). Thus, various etiological factors can cause damage to the visceral arteries and lead to circulatory disorders of the digestive organs [1,2,8–11]. Clinical picture The clinical picture of mesenteric circulation disorders manifests itself in two main forms - acute and chronic. The first form, leading to the development of intestinal infarction, has more or less distinct symptoms and is correctly diagnosed in a significant number of cases [8]. As for the clinical picture of chronic disorders of the blood supply to the digestive organs, it is less defined. Clinical manifestations of chronic ischemia of the digestive organs are extremely diverse. The disease has a lot of clinical “masks”, since the clinical picture of chronic ischemia of the digestive organs is similar to the clinical picture of a number of diseases of the gastrointestinal tract. In 94–96% of patients, the main symptom is pain that occurs after eating, and this fact is explained by insufficient blood flow to the digestive organs during their period of maximum activity, as well as by the sensitivity of the digestive organs to ischemia. The nature of the pain is also different: in the initial stage of the disease, the pain is equivalent to a feeling of heaviness in the epigastric region, then, with the worsening of circulatory disorders, aching pain appears, the intensity of which gradually increases [8,12]. The second common sign of chronic ischemia of the digestive organs is intestinal dysfunction, which is manifested by a violation of the secretory and absorption functions of the small intestine (flatulence, unstable stools, frequent loose stools), as well as a violation of the evacuation function of the colon with persistent constipation. Progressive weight loss is considered the third most common symptom of chronic ischemia of the digestive organs and is associated both with the refusal of patients to eat due to pain, and with a violation of the secretory and absorption functions of the small intestine, which is especially evident in the late stage of the disease [8,13,14 ]. A pathognomonic sign during an objective examination is a systolic murmur, determined with a predominant lesion of the abdominal aorta and/or celiac trunk (CS), 2–4 cm below the xiphoid process in the midline. With severe stenosis or occlusion of the visceral arteries, systolic murmur may be absent, which, however, is not a reason to exclude their damage [8,13]. The localization of ischemic damage to the digestive organs depends on the visceral artery feeding them. Thus, when an emergency occurs, the organs of the upper floor of the abdominal cavity are predominantly affected: the liver, pancreas, stomach, duodenum and spleen. Stenosis or occlusion of the superior mesenteric artery (SMA) is manifested by various dysfunctions of the small intestine, and damage to the inferior mesenteric artery (IMA) more often causes ischemia of the large intestine (IB) [3,14]. At the same time, the developed collateral network between the visceral arteries contributes to long-term functional compensation in conditions of impaired main blood flow, therefore, occlusive or stenotic lesions of the visceral branches of the abdominal aorta do not always lead to the appearance of symptoms of chronic ischemia of the digestive organs. The most striking clinical picture of chronic ischemia of the digestive organs is described when two or all three visceral arteries are affected [3,8,12,14]. The frequency of ulcerative lesions of the stomach and duodenum (duodenum) when the patency of unpaired visceral arteries is impaired is noteworthy. Thus, F. Olbert et al. [15] found them in 18% of patients with celiac trunk stenosis and in 50% of patients with SMA lesions. Other authors [3,9,16] found ulcerative lesions of the stomach and duodenum in more than 30% of patients with CIBOP of atherosclerotic origin and suggested that peptic ulcer disease in elderly and senile patients is the most common manifestation of CIBOP. According to a survey conducted at the Central Research Institute of Gastrointestinal Diseases, ischemic gastroduodenopathy was detected in 46.2% of cases and ranks first among the clinical forms of CIBOP [14]. With chronic disruption of the blood supply to the stomach and duodenum, a progressive evolution of the mucous membrane of these organs is observed in the form of atrophy. In this case, the mucous membrane of the antrum of the stomach is affected more often than the body and fundus, which is associated with the characteristics of vascularization and sensitivity to hypoxia. Impaired blood supply to the mucous membrane of the stomach and duodenum leads to a decrease in the production of protective mucosubstances by epithelial cells, which contributes to ulcer formation [17]. Characteristic clinical features of erosive and ulcerative lesions of the gastroduodenal zone in chronic abdominal ischemia are the manifestation of the disease in the form of bleeding, lack of seasonality of exacerbations, atypical clinical picture, high frequency of concomitant cardiovascular diseases, relapses, large size of the ulcer defect, low effectiveness of antiulcer therapy. The incidence of ischemic pancreatopathy in CIBOP is 33.9% [17]. The main feature of the blood supply to the pancreas is the absence of its own large arteries. The pancreas is supplied with blood from the branches of the common hepatic, superior mesenteric and splenic arteries. It is these features that determine the incidence of pancreatic necrosis, as well as the frequency of ischemic pancreatopathies during abdominal ischemia. There are certain difficulties in the differential diagnosis of ischemic pancreatopathy with banal chronic pancreatitis, because clinical manifestations of chronic ischemic pancreatitis are nonspecific. Both conditions are characterized by intense pain after eating in the epigastric region, left hypochondrium, which is not relieved (or poorly relieved) by antispasmodics, as well as sitophobia, pancreatic insufficiency, and weight loss [17]. Ischemic pancreatopathy can occur as acute ischemic pancreatitis, including fatal, chronic ischemic pancreatitis. It should be noted that chronic pancreatitis itself can be the cause of abdominal ischemia. Pancreatic cysts, exerting compression on nearby vessels, can eventually cause abdominal ischemia. Ischemic damage to the large intestine deserves special attention, which, according to our data, ranks third among other forms of CIBOP [17]. Thus, when examining patients with clinical symptoms of ischemic lesions of the colon (IPTC), in almost all of them, signs of impaired microcirculation and inflammation were found in the mucous membrane of the sigmoid colon, which is most vulnerable to disruption of the blood supply to the colon (since it is located in the area of poorly developed anastomoses). , characteristic of ischemic damage. Microscopic signs of ischemia appeared even before the development of macroscopic changes. Histological examination of the mucous membrane in these cases showed superficial necrosis of the epithelium, a decrease in the number of goblet cells, focal lymphoid cell infiltrates, paresis and plethora. These changes were accompanied by emptying of blood vessels, the development of stasis, thrombosis of the microvasculature and plasmorrhagia. We considered the described morphological changes in the mucous membrane of the sigmoid colon, identified by biopsy, to be the earliest reliable signs of IPTC. Based on the data obtained, we identified another form of IPTC - microscopic. By analogy with the well-known microscopic (lymphocytic and collagenous) colitis, we called this form “microscopic ischemic colitis” (MIC). This form of IPTC develops in elderly and senile patients suffering from diseases of the cardiovascular system. Characteristic symptoms of microscopic ischemic colitis are abdominal pain with a predominance in the left iliac region, appearing after eating, constipation, abdominal discomfort and flatulence. On objective examination, the sigmoid colon is painful, spasmodic, and the cecum is often dilated; a positive Obraztsov’s sign is characteristic [18]. Functional classes of CIBOP are distinguished depending on the severity of clinical manifestations of chronic ischemia of the digestive organs and the degree of disturbance of visceral blood flow [13,14]. The first functional class (I FC) – without pronounced clinical symptoms. These patients are characterized by the absence of disturbances in blood flow at rest and the appearance of abdominal pain only after a stress test. The second functional class (FC II) is the presence of signs of circulatory disorders at rest and their intensification after functional load, pronounced clinical symptoms: pain and dyspeptic syndromes, weight loss, impaired pancreatic function, impaired secretory-absorptive function of the intestine. The third functional class (III FC) includes patients with severe circulatory disorders, detected at rest and combined with constant pain, severe weight loss and dystrophic changes in the digestive organs. Diagnostic methods Diagnosis of CIBOP is based on the same principles as ischemic heart disease, i.e. detailing the patient's complaints, carefully collecting anamnesis, identifying risk groups for the possible development of atherosclerotic lesions of the abdominal aorta and its unpaired visceral branches (sensitivity 78%), on an objective examination of the abdominal aorta (palpation, auscultation). Analysis of the listed characteristic anamnestic data, complaints, signs of circulatory disorders in other arterial basins, as well as the systolic murmur heard in the projection of the visceral branches of the abdominal aorta give grounds to suggest a diagnosis of CIBOP. Due to the fact that objective data in the diagnosis of CIBOP are scarce, additional research is needed: studying the lipid spectrum of the blood, indicators of the blood coagulation system (fibrinogen, APTT and INR), aimed at identifying atherogenic dyslipidemia, disorders of the rheological properties of blood. Additional research methods that reveal pathological changes in the organs of the gastrointestinal tract provide some assistance in the diagnosis of CIBOP. All patients, along with laboratory research methods, also use instrumental ones, including esophagogastroduodenoscopy, colonoscopy with biopsy of the gastric mucosa, duodenum, colon mucosa, sonographic examination of the abdominal aorta, pancreas, in which the following parameters are studied: shape, contour size, echostructure and echo density of the organ. As a rule, an ultrasound examination of the abdominal aorta in transverse and longitudinal scanning visualizes its uneven, jagged intima, as well as echo-positive inclusions in its lumen, which indicates atherosclerotic lesions. However, the main role in verifying the diagnosis of CIBOP belongs to methods that directly detect occlusive-stenotic changes in the visceral arteries - Doppler ultrasound and angiography. There are great possibilities of Doppler ultrasound in the diagnosis of CIBOP, as well as a high correlation of the results obtained with angiography data [19]. Thus, to confirm the diagnosis of CIBOP, all patients undergo a Doppler examination of the main arteries of the abdominal cavity (ES, SMA, BA, splenic artery), both on an empty stomach and after a standard food load (500 ml of 3.5% fat milk and 300 g of unsweetened wheat bakery products), and when these indicators change compared to the norm, the degree of ischemia of the digestive organs is diagnosed. Nutritional load is a functional test for assessing mesenteric blood flow and allows us to determine the functional reserves of the digestive organs. In this case, the following parameters are determined that reflect the hemodynamics of the arterial bed: maximum linear blood flow velocity (Vmax), minimum linear blood flow velocity (Vmin), average blood flow velocity (TAMX), pulsatility index (PI), resistance index (RI), systole-diastolic ratio (S/D), and also conduct a qualitative assessment of Doppler curves. As a rule, when visceral blood flow is disrupted, an increase in all hemodynamic parameters is observed. When organic damage to the visceral arteries is detected according to Doppler studies, in order to determine treatment tactics, radiopaque aorto-arteriography is performed in direct and lateral projections according to the well-known Seldinger technique, and recently, in connection with the development of radiation diagnostic methods, computed tomographic angiography (CT angiography) is used ). This method combines traditional computed tomography with angiography, which allows you to obtain a detailed image of the blood vessels. Because this test injects contrast into a vein rather than an artery, it is considered less invasive than simple angiography. Treatment In the treatment of CIBOP, both conservative and surgical treatment methods are used. The tactics of conservative therapy depend on the severity of clinical manifestations of chronic ischemia of the digestive organs, i.e. functional class of the disease. Thus, patients with FC I are prescribed conservative treatment, which includes, first of all, strict adherence to a lipid-lowering diet: 10–15% proteins, 25–30% fats, 55–60% polysaccharide carbohydrates, vegetable fats, and foods containing fiber. Meals are fractional, in small portions. Diet recommendations take into account the individual characteristics of the patient’s body and concomitant diseases. The second important component of normalizing lipid levels is the use of lipid-lowering drugs. This type of therapy is used taking into account individual drug tolerance. It is possible to use drugs from the statin group: simvastatin 20–40 mg per day, fluvastatin 40 mg per day, atorvastatin at a dose of 10–40 mg per day. The maximum hypolipidemic effect occurs after 2-3 weeks from the beginning of treatment, however, the results of therapy to reduce cardiovascular complications begin to appear no earlier than 6–9 months from the start of statins. Due to the need for prolonged therapy, careful monitoring of the level of activity of liver enzymes is required. To prevent the manifestation of the hepatotoxic effect of statins, it is advisable to conduct hepatotropic therapy courses with essential phospholipids (Essential N and others) courses 2 months 2-3 times a year. The use of essential phospholipids helps to normalize the lipid blood spectrum, indicators of lipid peroxidation and antioxidant protection system. To correct the lipid spectrum of blood, patients with concomitant liver pathology (steatosis, steatogepatitis, fibrosis) as an alternative can be prescribed drugs of ursodeoxicholic acid in a standard dosage - 15 mg/kg. In patients with a high risk of developing atherosclerosis, to achieve target levels of cholesterol - LDL and reduce side effects, the most promising and providing high efficiency is a combination of statin with an inhibitor of the absorption of cholesterol. Modern provisions are based on double inhibiting the synthesis of cholesterol and its absorption, the use of selective intestinal absorption of cholesterol - ezetimib. The use of the Estimibe -Statin combination increases the decrease in the level of LDL cholesterol by 40%, without causing an increase in transaminase levels. During double therapy, it is possible to achieve the target values of the LDP cholesterol within 2 weeks. To improve the rheological properties of blood, drugs from a group of low molecular weight heparins are used, in particular, fraxyparin (calcium overparin), at a dose of 0.3 ml once a day for 2 weeks. For the purpose of antioxidant protection, the drug trimetasidine 20 mg x 3 r/day is used. During meals, within 3 months, twice a year. As an angioprotective effect and improvement of microcirculation, pentoxyphillin (Trental) 5.0 V/V is prescribed for 10 days. Patients with concomitant hypertension and coronary heart disease in order to normalize blood pressure and dilatation of coronary vessels, as well as improving the perfusion of internal organs, prescribe: nitro -group - isorbide dinitrate 10 mg x 3 times (maximum 20 mg x 4 times) per day,